An instrumental study of 392 households with sick or disabled members was conducted to analyze the psychometric properties of the Family Disease Management Scale. Three different models were analyzed using the Confirmatory Factor Analysis (CFA). One was a single-dimensional factor (family disease management) with 30 items; and two hierarchical models with three factors, which represent the dimensions, family support, family normalization and family participation, that placed the workload into another of higher order called family disease management, the first with 30 items and the second with 29. The CFA results showed that the latter 29-item model provided a better fit. The internal consistency analysis using the Cronbach alpha test showed a value of .93 for the complete scale and above .80 in the three subscales. This instrument may be useful to assess how families manage the illness or disability of its members, especially in clinical practice given the importance of the family as the primary caregiver. As well as in performing epidemiological studies, and in the field of management, planning and assistance.
Se realizó un estudio instrumental en 392 familias con miembros enfermos o discapacitados para estudiar las propiedades psicométricas de la Escala Manejo Familiar de la Enfermedad. Se analizaron tres modelos mediante Análisis Factorial Confirmatorio (AFC): uno con un factor (Manejo familiar de la enfermedad) con 30 ítems y otros dos jerárquicos, con tres factores, para las dimensiones apoyo familiar, normalización familiar y participación familiar, cuyos pesos se depositan en otro factor de orden mayor denominado Manejo familiar de la enfermedad, el primero con 30 ítems y el segundo con 29. Los resultados del AFC mostraron que el último modelo de 29 ítems obtuvo mejor ajuste. El análisis de la consistencia interna mostró valores de 0,93 para la escala completa y mayores de 0,80 en las tres subescalas. El instrumento podría usarse para valorar el manejo de la enfermedad o discapacidad de sus miembros por parte de las familias, especialmente en la práctica clínica, dada la importancia de la familia como cuidadora principal. También podría ser útil en estudios epidemiológicos o en la gestión y planificación sanitaria.
Disease is a phenomenon that becomes part of family life producing structural, procedural and emotional changes that affect family health; this is understood as the family's ability to function and adapt to stressful life events, which include the illness or disability of any of its members (Gabriel, Figueiredo, Jácome, Cruz, & Marques, 2014; Knafl & Gilliss, 2002). Different authors have tried to explain the psychological phases that families go through when a member is diagnosed with a condition. In these situations families usually have a period of crisis that is followed by a period of post-crisis, which are influenced by different modulate variables, such as illness characteristics, family background, perception of situation, family burden, resources, and other capabilities including resilence, hardiness, coping, and other family characteristics such as cohesion, flexibility, communication, organization or mutually supportive relationships (Gabriel et al., 2014; Joseph, Goodfellow, & Simko, 2014; Knafl et al., 2011; Olson, 2011). The families tend to adapt to illness by way of normalization strategies to integrate this situation into daily family life. In this sense, both mastery and routinization of the treatment are important aspects of family's response to illness (Knafl & Gilliss, 2002).
The family disease management could be defined as daily behavior that families perform to manage and adapt when a member is diagnosed with a condition (Knafl et al., 2011) and aims at generating a positive family environment, with emotional stability and ways of coping appropriately that allow the patient and all family members to adapt to the crisis and obtain the services and resources needed. So that, families must initiate strategies aimed at coping with the impact of the illness or disability on the patient by offering support and assistance, at obtaining the necessary normalization to continue functioning and to minimize its consequences for other family members, and also must actively participate in the health care provided to the sick member (Ford, Courtney-Pratt, & Fitzgerald, 2012; Lima-Rodríguez, Lima-Serrano, & Sáez-Bueno, 2009).
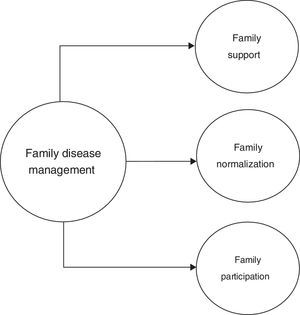
Conceptual definition of the construct under assessmentNursing outcomes classification (NOC) for family health domain, was used as a reference, from which family support during treatment, family normalization and family participation in professional care outcomes were selected (Lima-Rodríguez, Lima-Serrano, Jiménez-Picón, & Domínguez-Sánchez, 2013). NOC is a standardized classification of health outcomes, which has previously been used in designing clinometric instruments (Morales-Asencio et al., 2015). We considered that family disease management should be oriented to achieve the named outcomes given that they refer to key elements related to disease management, i.e., sick person, his/her family, and family participation in professional care.
Family support is related to the functions of support and care, providing for the patient's well-being and independence, and assisting in disease surveillance, decision-making and implementation of appropriate actions. The family should maintain good communication and empathy, provide information, material and emotional assistance, thus meeting the patient's basic needs. Previous studies have shown that the people with higher levels of family support have better adherence to the regime, better management of disease and lower hospitalization rates (Strom & Egede, 2012).
Family normalization starts acknowledging the new condition of the sick or disabled member and the potential changes needed to manage this situation (Knafl & Gilliss, 2002). It is related to changes in family functioning and organization, in which family has to be flexible in the performance of family roles, in modifying the family routine and housing conditions if necessary, and adjust their resources and apply for help for the extended family as well as the existing community social services (Ávila-Jiménez, Cerón, Ramos-Hernández, & Velázquez, 2013). Previous research showed the importance of including the care of the sick or disabled member in daily family life, especially for sick children and chronic disease (Emiliani, Bertocchi, Potì, & Palareti, 2011).
Family participation in the care process is particularly necessary in the case of children, disabilities or mental illness, terminally ill patients, etc., where the family should be involved in taking decisions about who to consult, when or where to go for treatment. The family is responsible for managing the sick person's day to day life, accompanying them regularly to the care professional or during hospitalization, providing key support to the professional in the communication with the patient, and identifying the factors that affect attendance and the attitudes and behaviors that are most effective for coping with the problem (Rosland et al., 2013; Wolff & Roter, 2011); and the participation of the family in the care plan is also a positive motivator in achieving results (Blomqvist & Ziegert, 2011; Osawa & Maeshima, 2010).
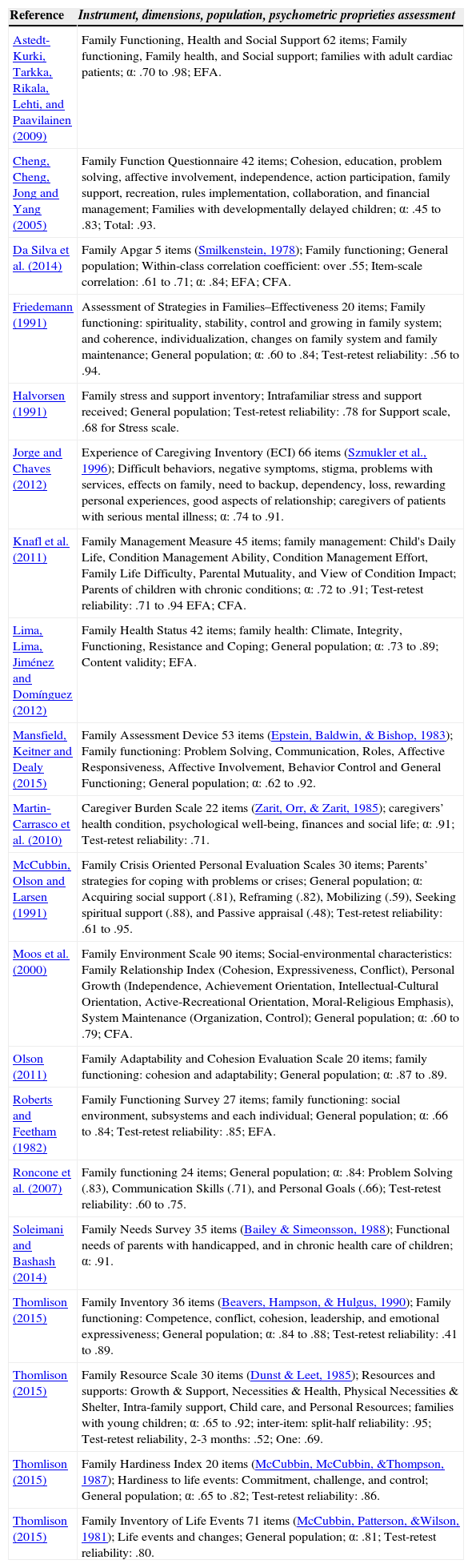
Different instruments were designed to measure different aspects relating to family health, focused mainly on family functioning, stressing life events or strategies for coping with these situations (Table 1). We could point the Family APGAR (Da Silva et al., 2014), the Family Cohesion and Adaptability Evaluation Scale (Olson, 2011), the Social Climate Scale (Moos, Moos, & Trickett, 2000), or the Family Management Measure for Families of Children with Chronic Conditions (Knafl et al., 2011).
Scales for assess family needs: Literature review.
| Reference | Instrument, dimensions, population, psychometric proprieties assessment |
|---|---|
| Astedt-Kurki, Tarkka, Rikala, Lehti, and Paavilainen (2009) | Family Functioning, Health and Social Support 62 items; Family functioning, Family health, and Social support; families with adult cardiac patients; α: .70 to .98; EFA. |
| Cheng, Cheng, Jong and Yang (2005) | Family Function Questionnaire 42 items; Cohesion, education, problem solving, affective involvement, independence, action participation, family support, recreation, rules implementation, collaboration, and financial management; Families with developmentally delayed children; α: .45 to .83; Total: .93. |
| Da Silva et al. (2014) | Family Apgar 5 items (Smilkenstein, 1978); Family functioning; General population; Within-class correlation coefficient: over .55; Item-scale correlation: .61 to .71; α: .84; EFA; CFA. |
| Friedemann (1991) | Assessment of Strategies in Families–Effectiveness 20 items; Family functioning: spirituality, stability, control and growing in family system; and coherence, individualization, changes on family system and family maintenance; General population; α: .60 to .84; Test-retest reliability: .56 to .94. |
| Halvorsen (1991) | Family stress and support inventory; Intrafamiliar stress and support received; General population; Test-retest reliability: .78 for Support scale, .68 for Stress scale. |
| Jorge and Chaves (2012) | Experience of Caregiving Inventory (ECI) 66 items (Szmukler et al., 1996); Difficult behaviors, negative symptoms, stigma, problems with services, effects on family, need to backup, dependency, loss, rewarding personal experiences, good aspects of relationship; caregivers of patients with serious mental illness; α: .74 to .91. |
| Knafl et al. (2011) | Family Management Measure 45 items; family management: Child's Daily Life, Condition Management Ability, Condition Management Effort, Family Life Difficulty, Parental Mutuality, and View of Condition Impact; Parents of children with chronic conditions; α: .72 to .91; Test-retest reliability: .71 to .94 EFA; CFA. |
| Lima, Lima, Jiménez and Domínguez (2012) | Family Health Status 42 items; family health: Climate, Integrity, Functioning, Resistance and Coping; General population; α: .73 to .89; Content validity; EFA. |
| Mansfield, Keitner and Dealy (2015) | Family Assessment Device 53 items (Epstein, Baldwin, & Bishop, 1983); Family functioning: Problem Solving, Communication, Roles, Affective Responsiveness, Affective Involvement, Behavior Control and General Functioning; General population; α: .62 to .92. |
| Martin-Carrasco et al. (2010) | Caregiver Burden Scale 22 items (Zarit, Orr, & Zarit, 1985); caregivers’ health condition, psychological well-being, finances and social life; α: .91; Test-retest reliability: .71. |
| McCubbin, Olson and Larsen (1991) | Family Crisis Oriented Personal Evaluation Scales 30 items; Parents’ strategies for coping with problems or crises; General population; α: Acquiring social support (.81), Reframing (.82), Mobilizing (.59), Seeking spiritual support (.88), and Passive appraisal (.48); Test-retest reliability: .61 to .95. |
| Moos et al. (2000) | Family Environment Scale 90 items; Social-environmental characteristics: Family Relationship Index (Cohesion, Expressiveness, Conflict), Personal Growth (Independence, Achievement Orientation, Intellectual-Cultural Orientation, Active-Recreational Orientation, Moral-Religious Emphasis), System Maintenance (Organization, Control); General population; α: .60 to .79; CFA. |
| Olson (2011) | Family Adaptability and Cohesion Evaluation Scale 20 items; family functioning: cohesion and adaptability; General population; α: .87 to .89. |
| Roberts and Feetham (1982) | Family Functioning Survey 27 items; family functioning: social environment, subsystems and each individual; General population; α: .66 to .84; Test-retest reliability: .85; EFA. |
| Roncone et al. (2007) | Family functioning 24 items; General population; α: .84: Problem Solving (.83), Communication Skills (.71), and Personal Goals (.66); Test-retest reliability: .60 to .75. |
| Soleimani and Bashash (2014) | Family Needs Survey 35 items (Bailey & Simeonsson, 1988); Functional needs of parents with handicapped, and in chronic health care of children; α: .91. |
| Thomlison (2015) | Family Inventory 36 items (Beavers, Hampson, & Hulgus, 1990); Family functioning: Competence, conflict, cohesion, leadership, and emotional expressiveness; General population; α: .84 to .88; Test-retest reliability: .41 to .89. |
| Thomlison (2015) | Family Resource Scale 30 items (Dunst & Leet, 1985); Resources and supports: Growth & Support, Necessities & Health, Physical Necessities & Shelter, Intra-family support, Child care, and Personal Resources; families with young children; α: .65 to .92; inter-item: split-half reliability: .95; Test-retest reliability, 2-3 months: .52; One: .69. |
| Thomlison (2015) | Family Hardiness Index 20 items (McCubbin, McCubbin, &Thompson, 1987); Hardiness to life events: Commitment, challenge, and control; General population; α: .65 to .82; Test-retest reliability: .86. |
| Thomlison (2015) | Family Inventory of Life Events 71 items (McCubbin, Patterson, &Wilson, 1981); Life events and changes; General population; α: .81; Test-retest reliability: .80. |
Note. EFA: exploratory factor analysis; CFA: confirmatory factor analysis.
We are unaware of the existence of a general instrument aimed at assessing family disease management where there is a sick or disabled member; and previous authors have stated the value of designing and validating new instruments where there are no others that assess the construct that it is really sought to measure (Carretero-Dios & Pérez, 2007). This instrument could be useful for having a better understanding of the common challenges experienced by families in these situations, making it easier to compare family management across different conditions rather than a specific one (Knafl et al., 2011).
Construction and qualitative assessmentWe performed an exhaustive literature review of family health and family management (Psycinfo, Pubmed, Scopus, and Web of Science) to clarify and develop the main concepts. The originally Family Disease Management scale was designed, consisting on 36 items and three dimensions of family support, family normalization and family participation with twelve each in dimension. A content validation by a quali-quantitative study was performed using an on-line Delphi panel as a consensus technique with eighteen experts on the study topic, including doctors, nurses and psychologists. The degree of adequacy of each item was established, according to five-points Likert-scale; the opportunity to suggest new items or propose amendments was also offered. The items were assessed according to the following criteria: Validated: mean ≥ 3.5 and median ≥ 3 and high ratings (4-5) ≥ 80% and/or standard deviation ≤ 0.90. Eliminated: mean <3.5 and median <3. Finally, it took a total of two rounds to reach the necessary level of consensus and to refine a 30-items scale (Lima-Rodríguez et al., 2013).
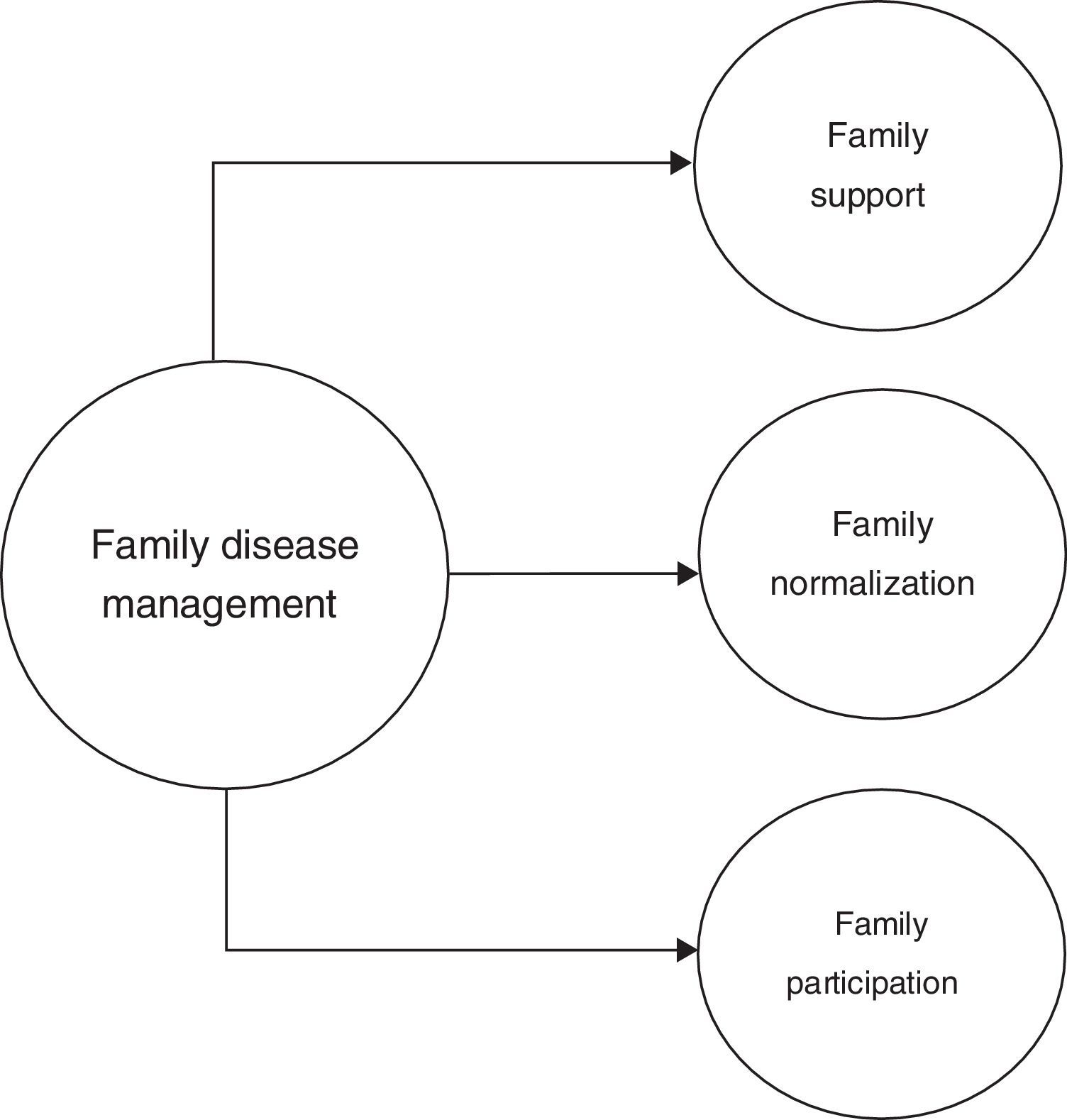
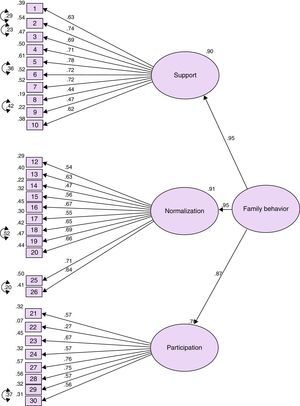
The aim of the present work was to study the factor structure (Confirmatory Factor Analysis [CFA]) and the internal consistence of the Family Disease Management Scale. Taking into account the theoretical and empirical issues previously discussed we hypothesize a one-dimensional construct (Family Disease Management) with three sub-dimensions, family support, family normalization, and family participation in the care process (Figure 1).
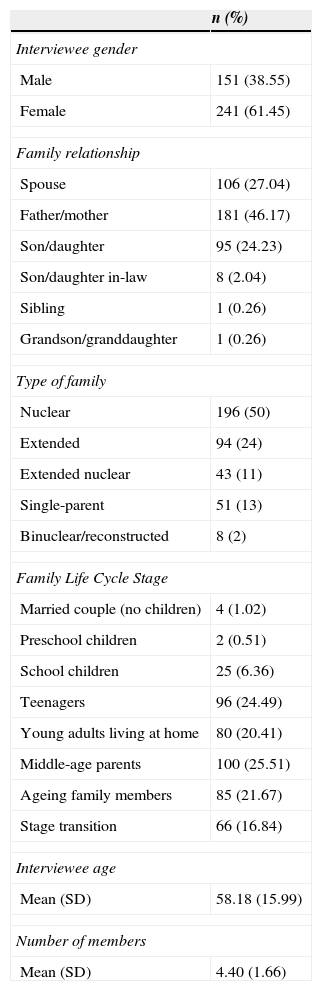
MethodParticipantsThe sample size was arrived following the recommendations of over 200 individuals to perform the confirmatory factor analysis (Morales, 2006). Finally, an intentional sample of 392 households of two or more members with sick or disabled members was interviewed. The interviewee was a caregiver, adult (more than 18 years of age). Those that showed cognitive decline were excluded. The households had an average size of 4.4 members. Most of them were nuclear (50%) or extended families (24%). Regarding the stage of family life cycle, 25.5% were middle age parents and 25% had adolescent children. Rest of descriptions is shown in Table 2.
Descriptive for the sample.
| n (%) | |
|---|---|
| Interviewee gender | |
| Male | 151 (38.55) |
| Female | 241 (61.45) |
| Family relationship | |
| Spouse | 106 (27.04) |
| Father/mother | 181 (46.17) |
| Son/daughter | 95 (24.23) |
| Son/daughter in-law | 8 (2.04) |
| Sibling | 1 (0.26) |
| Grandson/granddaughter | 1 (0.26) |
| Type of family | |
| Nuclear | 196 (50) |
| Extended | 94 (24) |
| Extended nuclear | 43 (11) |
| Single-parent | 51 (13) |
| Binuclear/reconstructed | 8 (2) |
| Family Life Cycle Stage | |
| Married couple (no children) | 4 (1.02) |
| Preschool children | 2 (0.51) |
| School children | 25 (6.36) |
| Teenagers | 96 (24.49) |
| Young adults living at home | 80 (20.41) |
| Middle-age parents | 100 (25.51) |
| Ageing family members | 85 (21.67) |
| Stage transition | 66 (16.84) |
| Interviewee age | |
| Mean (SD) | 58.18 (15.99) |
| Number of members | |
| Mean (SD) | 4.40 (1.66) |
In order to characterize the sample we asked questions about composition, typology, and the Family Life Cycle Stage. The 30-item Family Disease Management scale was used for testing its psychometric properties (Appendix 1).
Data collection and procedureIt took place between October 2012 and November 2013. A self-administered format was used by interviewers previously trained at health centers belonging to the Andalusian Health Service or family homes. Anonymity, confidentiality and data protection were guaranteed, by using informed consent. The study was approved by the ethics committee of the University of Seville.
Statistical analysisWe performed a CFA with AMOS 22.0. This provides an appropriate statistical framework to evaluate psychometric properties where there is a clear idea of the scale dimensionality and specific hypotheses that relate indicators and latent dimensions (Batista-Foguet, Coenders, & Alonso, 2004). In fact, there are precedents for using this technique in both validating new scales (Carlos & Rodrigues, 2015) and transcultural adaption of scales (Malegiannaki, Metallidou, & Kiosseoglou, 2015). Different factor solutions were tested, a first formula with 30 items characterized by a one-dimensional construct (family disease management), a second formula with 30 items characterized by three first-order factors (support, normalization, and participation) and one second-order factor (family disease management), and a third formula with 29 items characterized by three first-order factors (support, normalization, and participation) and one second-order factor (family disease management). In this last formula, empirical modifications to the reference models were introduced taking into account changes in modification indices, goodness of fit indices and factorial charges, and regarding the results this showed a better fit. The Kaiser-Meyer-Olkin index (KMO) and Bartlett's test of sphericity were examined, whose results greater than .80 and levels of significance lower than .001 respectively indicated the appropriateness of conducting CFA. In addition, we used Mardia's coefficient (Bollen, 1989), considering multivariate normal distribution if this coefficient is lower than p (p+2) where p is a number of observed variables (30 observed variables).
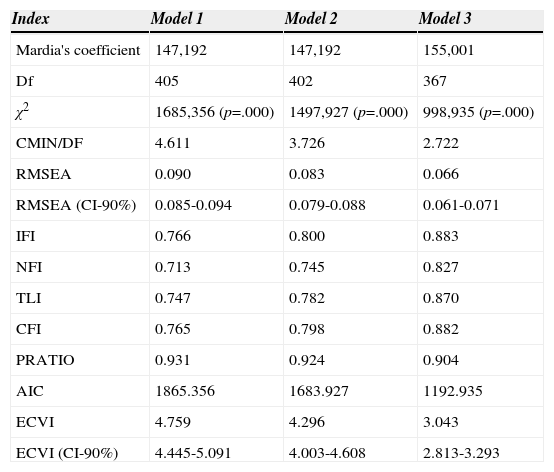
Goodness of fit indices. We examined the magnitude χ2 to chose the model in which this is smaller; the discrepancy divided by its degrees of freedom (CMIN/DF [should be lower than 3]); Root Mean Square Error of Approximation (RMSEA<.08); Incremental fit index (IFI); Normed fit index (NFI); Comparative Fit Index (CFI); Tucker-Lewis Index (TLI); Parsimony ratio (PRATIO). The values of these indices should be close to .90 to be considered a good fit. Information Criterion (AIC) and Expected Cross-Validation Index (ECVI) were calculated, indicating the lower the values, the better the fit (Akaike, 1987; Hu & Bentler, 1998; Steiger, 1990; Tabachnick & Fidell, 2013). Regarding internal consistence, we tested whether the Cronbach's alpha coefficient became greater if an item was deleted, and we considered that reliability indices located around .80 are adequate. We analyzed the discrimination index of corrected item-total correlations that should be higher than 1/√k (k=number of items) (Morales, 2006). We tried to confirm internal consistency and each item's contribution to the respective examination's total score of three different models. Analysis was carried out with SPSS 22.0.
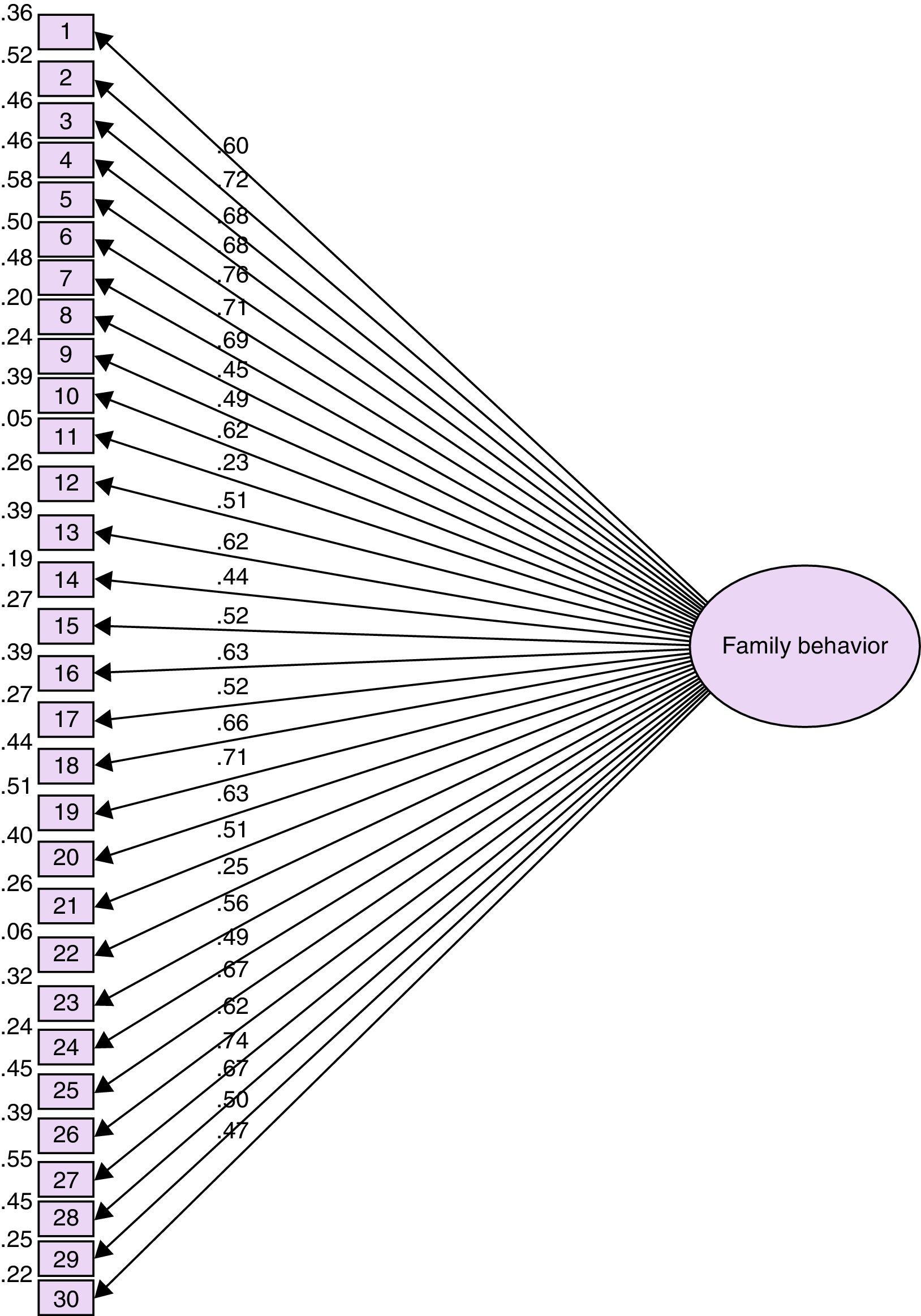
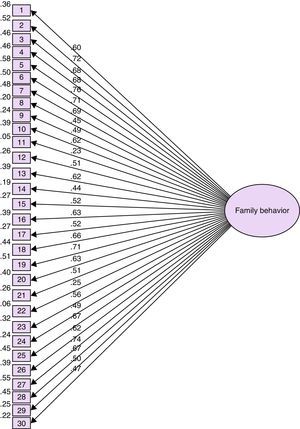
ResultsFactor structureThe KMO was .92 and Bartlett's test showed non-significant values (p=.000). In the first model, family disease management was considered as a one-dimensional construct determined by 30 observed variables (items) [Figure 2]. Factor loadings ranged between .23 (item 11) and .76 (item 5) whereas measurement errors ranged between .05 (item 11) and .58 (item 5). Only PRATIO=.93 indicates a possible fit (Table 3).
Goodness of fit indices for three tested confirmatory factor analysis models.
| Index | Model 1 | Model 2 | Model 3 |
|---|---|---|---|
| Mardia's coefficient | 147,192 | 147,192 | 155,001 |
| Df | 405 | 402 | 367 |
| χ2 | 1685,356 (p=.000) | 1497,927 (p=.000) | 998,935 (p=.000) |
| CMIN/DF | 4.611 | 3.726 | 2.722 |
| RMSEA | 0.090 | 0.083 | 0.066 |
| RMSEA (CI-90%) | 0.085-0.094 | 0.079-0.088 | 0.061-0.071 |
| IFI | 0.766 | 0.800 | 0.883 |
| NFI | 0.713 | 0.745 | 0.827 |
| TLI | 0.747 | 0.782 | 0.870 |
| CFI | 0.765 | 0.798 | 0.882 |
| PRATIO | 0.931 | 0.924 | 0.904 |
| AIC | 1865.356 | 1683.927 | 1192.935 |
| ECVI | 4.759 | 4.296 | 3.043 |
| ECVI (CI-90%) | 4.445-5.091 | 4.003-4.608 | 2.813-3.293 |
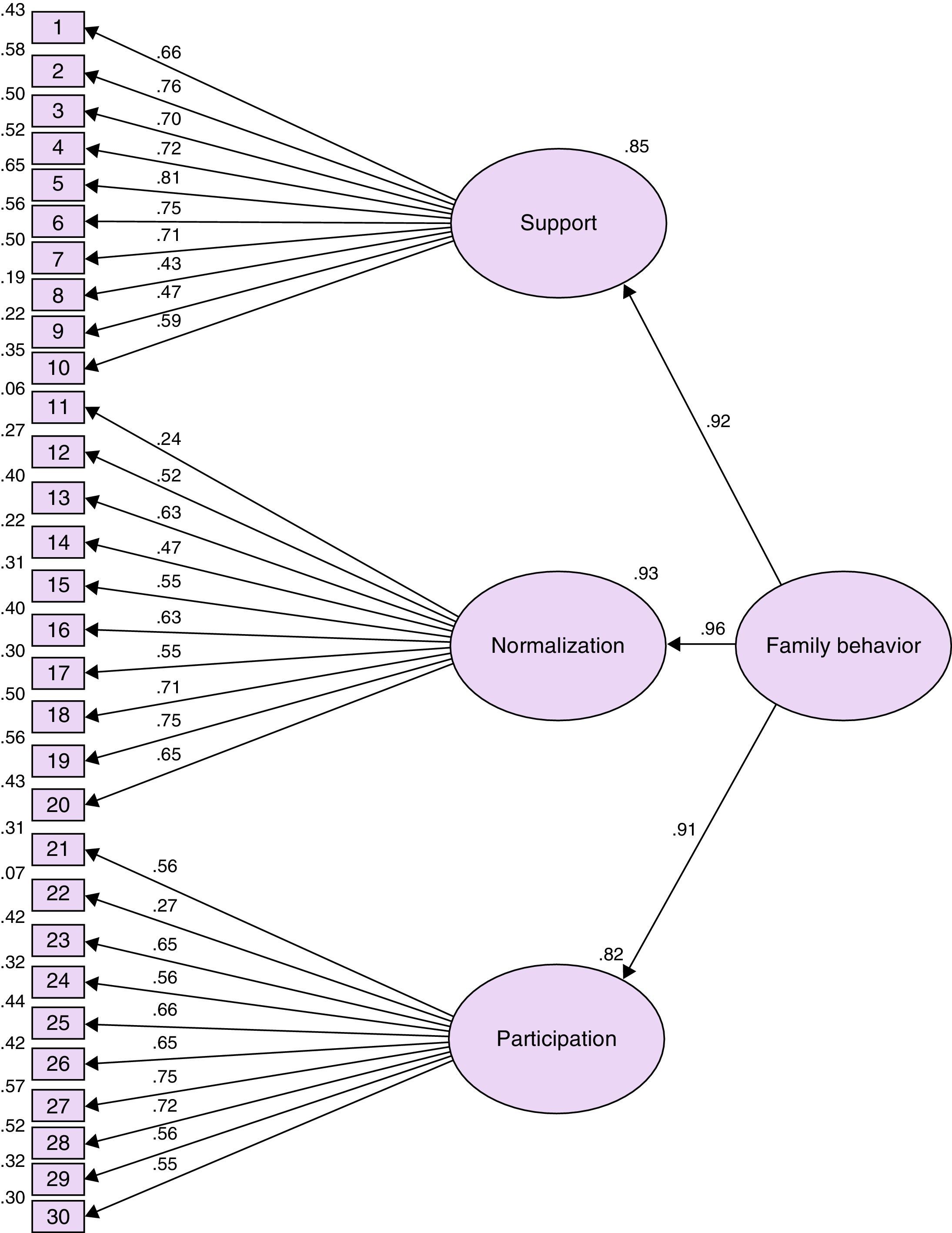
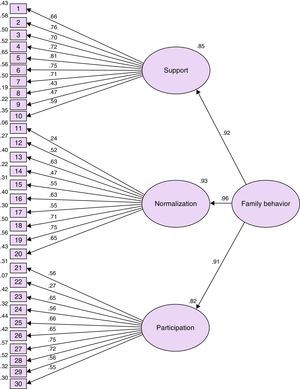
We then tested a second model, more potentially plausible, determining three first-order factors (support, normalization and participation), each one measured by ten items, with these first-order factors all loading onto one higher-order factor (family disease management) [Figure 3]. Factor loadings ranged between .24 (item 11) and .81 (item 5) whereas measurement errors ranged between .06 (item 11) and .65 (item 5). The amount of variance explained by the latent traits ranged between .91 and .96. This model showed a better fit, close to being acceptable.
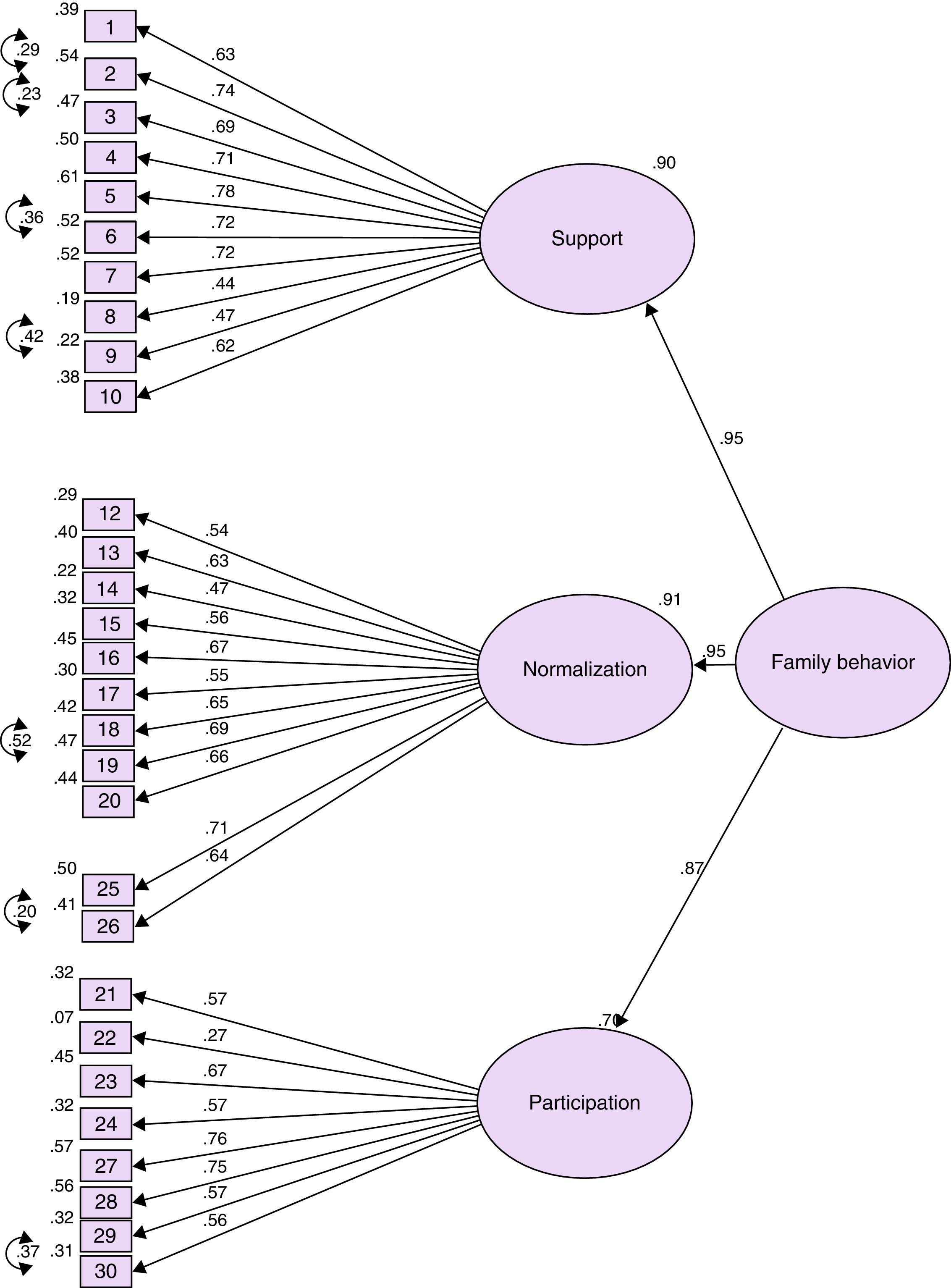
Finally, we introduced several sequential empirical modifications, by re-examining the results, and we tested a third model consisted of factor solutions with three first-order factors that involved 29 items (support with ten items, normalization with eleven items and participation with eight) loading onto one higher-order factor (family disease management). Modification indices suggested the liberalization of the covariance between seven par error measures, those corresponding to par e1*e2 (r=.25, p<.001), par e5*e6 (r=.56, p<.001), par e12*e13 and par e13*e14 (r=.24, p<.001), par e16*e17 (r=.39, p<.001), par e19*e20 (r=.47, p<.001), and par e27*e28 (r=.35, p<.001) [Figure 4]. The factor loadings ranged between .27 (item 22) and 0.78 (item 5) whereas measurement errors ranged between .07 (item 22) and .61 (item 5). The amount of variance explained by the latent traits ranged between .87 and .95. This model showed the best goodness of fit indices as can be seen in Table 3.
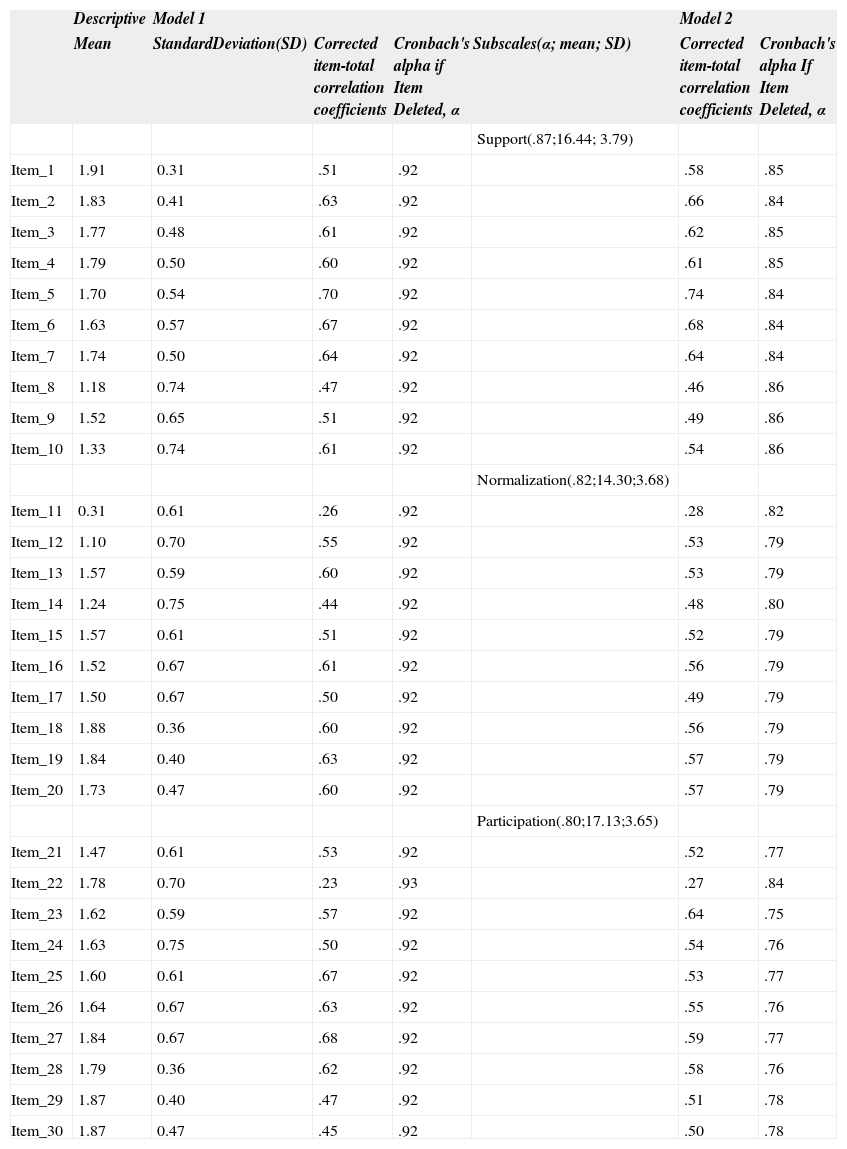
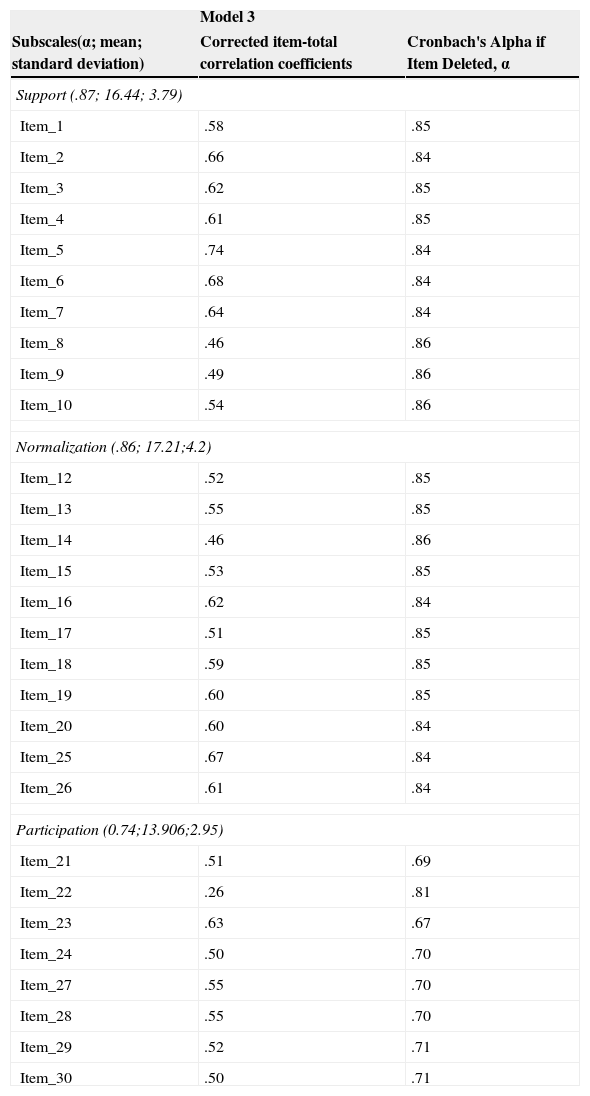
Internal consistency reliabilityIn the three models tested Cronbach's Alpha was higher than .70 for the whole scale and subscales. It was stable or decreased if an item was deleted, except for item 22 in the participation subscale (in both model 2 and 3). Moreover, corrected item-total correlation coefficients were higher than 1/√k, except in item-11 (model 1 and model 2) and item 22 in the three tested models. For the rest of the items, coefficients were higher than .40 (Tables 4 and 5).
Descriptive and internal consistency reliability of Models 1 and 2.
| Descriptive | Model 1 | Model 2 | |||||
|---|---|---|---|---|---|---|---|
| Mean | StandardDeviation(SD) | Corrected item-total correlation coefficients | Cronbach's alpha if Item Deleted, α | Subscales(α; mean; SD) | Corrected item-total correlation coefficients | Cronbach's alpha If Item Deleted, α | |
| Support(.87;16.44; 3.79) | |||||||
| Item_1 | 1.91 | 0.31 | .51 | .92 | .58 | .85 | |
| Item_2 | 1.83 | 0.41 | .63 | .92 | .66 | .84 | |
| Item_3 | 1.77 | 0.48 | .61 | .92 | .62 | .85 | |
| Item_4 | 1.79 | 0.50 | .60 | .92 | .61 | .85 | |
| Item_5 | 1.70 | 0.54 | .70 | .92 | .74 | .84 | |
| Item_6 | 1.63 | 0.57 | .67 | .92 | .68 | .84 | |
| Item_7 | 1.74 | 0.50 | .64 | .92 | .64 | .84 | |
| Item_8 | 1.18 | 0.74 | .47 | .92 | .46 | .86 | |
| Item_9 | 1.52 | 0.65 | .51 | .92 | .49 | .86 | |
| Item_10 | 1.33 | 0.74 | .61 | .92 | .54 | .86 | |
| Normalization(.82;14.30;3.68) | |||||||
| Item_11 | 0.31 | 0.61 | .26 | .92 | .28 | .82 | |
| Item_12 | 1.10 | 0.70 | .55 | .92 | .53 | .79 | |
| Item_13 | 1.57 | 0.59 | .60 | .92 | .53 | .79 | |
| Item_14 | 1.24 | 0.75 | .44 | .92 | .48 | .80 | |
| Item_15 | 1.57 | 0.61 | .51 | .92 | .52 | .79 | |
| Item_16 | 1.52 | 0.67 | .61 | .92 | .56 | .79 | |
| Item_17 | 1.50 | 0.67 | .50 | .92 | .49 | .79 | |
| Item_18 | 1.88 | 0.36 | .60 | .92 | .56 | .79 | |
| Item_19 | 1.84 | 0.40 | .63 | .92 | .57 | .79 | |
| Item_20 | 1.73 | 0.47 | .60 | .92 | .57 | .79 | |
| Participation(.80;17.13;3.65) | |||||||
| Item_21 | 1.47 | 0.61 | .53 | .92 | .52 | .77 | |
| Item_22 | 1.78 | 0.70 | .23 | .93 | .27 | .84 | |
| Item_23 | 1.62 | 0.59 | .57 | .92 | .64 | .75 | |
| Item_24 | 1.63 | 0.75 | .50 | .92 | .54 | .76 | |
| Item_25 | 1.60 | 0.61 | .67 | .92 | .53 | .77 | |
| Item_26 | 1.64 | 0.67 | .63 | .92 | .55 | .76 | |
| Item_27 | 1.84 | 0.67 | .68 | .92 | .59 | .77 | |
| Item_28 | 1.79 | 0.36 | .62 | .92 | .58 | .76 | |
| Item_29 | 1.87 | 0.40 | .47 | .92 | .51 | .78 | |
| Item_30 | 1.87 | 0.47 | .45 | .92 | .50 | .78 |
Total Scale, α: .93; Mean: 47.88; SD: 10.04
Scale Descriptive, internal consistency reliability of Model 3.
| Model 3 | ||
|---|---|---|
| Subscales(α; mean; standard deviation) | Corrected item-total correlation coefficients | Cronbach's Alpha if Item Deleted, α |
| Support (.87; 16.44; 3.79) | ||
| Item_1 | .58 | .85 |
| Item_2 | .66 | .84 |
| Item_3 | .62 | .85 |
| Item_4 | .61 | .85 |
| Item_5 | .74 | .84 |
| Item_6 | .68 | .84 |
| Item_7 | .64 | .84 |
| Item_8 | .46 | .86 |
| Item_9 | .49 | .86 |
| Item_10 | .54 | .86 |
| Normalization (.86; 17.21;4.2) | ||
| Item_12 | .52 | .85 |
| Item_13 | .55 | .85 |
| Item_14 | .46 | .86 |
| Item_15 | .53 | .85 |
| Item_16 | .62 | .84 |
| Item_17 | .51 | .85 |
| Item_18 | .59 | .85 |
| Item_19 | .60 | .85 |
| Item_20 | .60 | .84 |
| Item_25 | .67 | .84 |
| Item_26 | .61 | .84 |
| Participation (0.74;13.906;2.95) | ||
| Item_21 | .51 | .69 |
| Item_22 | .26 | .81 |
| Item_23 | .63 | .67 |
| Item_24 | .50 | .70 |
| Item_27 | .55 | .70 |
| Item_28 | .55 | .70 |
| Item_29 | .52 | .71 |
| Item_30 | .50 | .71 |
Total Scale, α: .93; Mean:47.56; Standard deviation: 9.86
A scale designed to measure family disease management in families with sick or disabled members was assessed. The psychometric properties were tested in a large sample of families of different composition, type, and stages of the family life cycle; this sample was consistent with the indications from previous which gives more power and strength to the validation process. On the other hand, the analysis of internal consistency values have been appropriated according to the recommendations, as reliability indices located around around α=.80 are adequate for diagnosis or classification (Morales, 2006).
Regarding the factor structure the suitability of three models was tested; and the third hierarchical model showed the best goodness of fit indices. This involved 29 items with three first-order factors that represent the constructs, family support, family normalization and family participation, where these three factors deposit all the load onto another higher order called family disease management. In this model, items 1 to 10 assess family support; items 12 to 20, 25 and 26 assess family normalization; and items 21 to 29 family participation. The factor loads of all items were above .40, with significant values, except item 22 but it was maintained to improve its goodness of fit.
The family support subscale assesses basic help functions and the necessary demands for obtaining good family support, being related to adherence to therapeutic regime, control and management of the disease (Joseph et al., 2014; Strom & Egede, 2012). The family normalization subscale assesses the way the family adapts to meet the daily needs of the patient and the rest of its members, which contribute to improved normal functioning, satisfaction and family caregivers’ health, and strengthen families by allowing them to take the necessary measures to meet emerging needs, reducing their levels of family concern (Ávila-Jiménez et al., 2013; Ford et al., 2012; Knafl & Gilliss, 2002). Finally, the family participation subscale assesses how the family is involved in the care process, either participating in or accompanying and maintaining the system support to the sick relative, significantly contributing to professional practice (Blomqvist & Ziegert, 2011; Osawa & Maeshima, 2010).
Limitations. First, although previous authors state the goodness of CFA for testing psychometric properties (Batista-Foguet et al., 2004), it might be appropriate to carry out previously other techniques regarding classical test theory, including exploratory factorial analysis. Second, although we accepted the third model as more adequate regarding goodness of fit indices proposed, other authors proposed stricter cut-off points such as RMSEA<.05 whereas TLI and CFI greater than .95 (Arias, Verdugo, Navas, & Gómez, 2013), and in our study these indices have reached .066, .870 and .882 respectively. Third, the external validity of the instrument, including cross-validation techniques, is not shown and should be carried out in future research. Fourth, we did not ask about the kind and grade or the number of years of disease/disability of the sick family member and it could be interesting for comparing family disease management regarding these factors.
In spite of limitations, this study provides evidence of factor structure and internal consistence of a scale and subscales designed to evaluate family disease management. The instrument provides specific indicators to measure family support to a sick or disabled family member, family normalization and family participation in the care process. This scale could be useful for clinical practice, since the family is the main provider of care; and for epidemiological studies and other types of research in the field of management, planning and assistance.
| When someone falls ill in my family (Cuando hay un enfermo en la familia): | HE | ST | NA |
|---|---|---|---|
| 1. We worry about their condition (Nos preocupamos por su estado) | |||
| 2. We take care of their needs (Nos encargamos de cubrir sus necesidades) | |||
| 3. We help them with those tasks they cannot do (Le ayudamos con aquellas tareas que no pueda realizar) | |||
| 4. We help them follow the medical treatment (Le ayudamos a seguir el tratamiento médico) | |||
| 5. We try to communicate and listen to them (Tratamos de escucharlo y comunicarnos con él) | |||
| 6. We try to understand their situation (Intentamos entender su situación) | |||
| 7. We encourage them to participate in improving their health (Le animamos a que ponga de su parte para mejorar su salud) | |||
| 8. We ask other family members for help (Pedimos ayuda a otras personas de la familia) | |||
| 9. We let the rest of the family know about their condition. (Informamos de su estado al resto de la familia) | |||
| 10. We all collaborate in caring for them (Colaboramos todos en su cuidado) | |||
| 11. We go to associations of people who have the same problem* (Acudimos a asociaciones de personas con el mismo problema*) | |||
| 12. We observe how this can affect the rest of the family (Vemos cómo puede afectar al resto de la familia) | |||
| 13. We are part of the daily care of their illness (Integramos en el día a día el cuidado de su enfermedad) | |||
| 14. We try to help other affected members (Intentamos ayudar a otros miembros afectados) | |||
| 15. We encourage them to be as independent as possible (Lo animamos a que sea lo más autónomo posible) | |||
| 16. We organize the tasks that they cannot perform (Nos organizamos con las tareas que no pueda realizar) | |||
| 17. We adapt the house to their needs (Adaptamos la casa a sus necesidades) | |||
| 18. We want them to feel as well as possible (Pretendemos que se encuentre lo mejor posible) | |||
| 19. We want them to live the situation as well as possible (Intentamos que viva la situación lo mejor posible) | |||
| 20. We ensure that the family works normally (Procuramos que la familia funcione con normalidad) | |||
| 21. We participate in the decisions about what to do (Participamos en las decisiones sobre lo que va a hacer) | |||
| 22. We take the decision if the patient cannot (Tomamos decisiones si el enfermo no puede hacerlo) | |||
| In my family when someone receives health care (En mi familia cuando alguien recibe asistencia sanitaria): | |||
| 23. We actively collaborate with the professionals (Colaboramos activamente con los profesionales) | |||
| 24. We assess whether the assistance is provided adequately (Valoramos si la asistencia se presta de forma adecuada) | |||
| 25. We are organized to help whenever it is necessary (Nos organizamos para ayudar cuando es necesario) | |||
| 26. We try to obtain the necessary resources (Tratamos de conseguir los recursos necesarios) | |||
| 27. We ensure that the patient has everything they need (Aseguramos que el enfermo tenga lo que necesite) | |||
| 28. We accompany them during care (Lo acompañamos durante la misma) | |||
| 29. We give the professional the information they need (Ofrecemos al profesional la información que necesite) | |||
| 30. We ask the professional to inform us about their state (Pedimos al profesional que nos informe sobre su estado) |
Note. Hardly Ever (HE), Sometimes (ST), Nearly always (NA).