Background/Objective: The evidence on efficacy of cognitive-behavioral interventions in Eating Disorders (ED) still shows inconclusive results with respect to the role of purging behaviors, more so in uncontrolled situations. Evolution of ED patients with and without purging behavior was studied 30 months after start of a multicomponent treatment. Method: 162 women (87 purging, 75 non-purging) treated in outpatient or hospitals+outpatient care units in Spain participated. The evaluation instruments were: BSQ, EAT-40, EDI, STAI, BDI and BITE. Results: At the beginning of the treatment, participants with purging behavior showed higher bulimic symptomatology, more body dissatisfaction, drive for thinness, perfectionism and ineffectiveness, anxiety and depressive symptomatology. After thirty months, intervention produced improvement in ED characteristics, emotional alterations and personal development variables, in both groups, but less in patients with no purging behavior. The effect of intervention was stronger in purging patients and variables with larger effect size: body dissatisfaction, bulimic symptomatology and anxiety. Conclusions: Purging behaviors must be considered in the design of these treatments with a view to prognosis.
La evidencia sobre la eficacia de intervenciones cognitivo-conductuales en los Trastornos de la Conducta Alimentaria (TCA) aún presenta resultados no concluyentes respecto al papel que desempeñan en las conductas purgativas, más aún cuando se realizan en situaciones no controladas. Se pretende conocer la evolución tras un tratamiento multicomponente en pacientes con TCA, con presencia o ausencia de conductas purgativas, después de 30 meses del inicio del tratamiento.
MétodoParticiparon 162 mujeres (87 purgativas y 75 no purgativas), tratadas en régimen ambulatorio o hospitalario+ambulatorio, en España. Los instrumentos de evaluación fueron: BSQ, EAT-40, EDI, STAI, BDI y BITE.
ResultadosAl inicio del tratamiento, las participantes con conductas purgativas presentaban mayor sintomatología bulímica, más insatisfacción corporal, obsesión por la delgadez, perfeccionismo e ineficacia, ansiedad y sintomatología depresiva. Tras 30 meses, en ambos grupos, la intervención produjo mejoría en las características de TCA, alteraciones emocionales y variables de desarrollo personal, siendo menor en las pacientes sin conductas purgativas. El efecto de la intervención fue mayor en las participantes purgativas y las variables con mayor tamaño de efecto: insatisfacción corporal, sintomatología bulímica y ansiedad.
ConclusionesEs importante considerar las conductas purgativas en el diseño de estos tratamientos de cara al pronóstico.
Empirical evidence has demonstrated the efficacy of cognitive-behavioral treatment (CBT) in eating disorders (ED), especially in bulimia nervosa (BN) (Fairburn et al., 2013; Poulsen et al., 2014; Watson & Bulik, 2013; Zipel et al., 2014). Studies have shown the role of recurrent purging behaviors in ED, purging subtype, such as self-induced vomiting for its effect on weight or shape. Several authors have tried to identify similarities and differences in the severity of eating disorder symptomatology and personality characteristics in disorders with purging behaviors, however, results are still not conclusive (Brown, Haedt-Matt, & Keel, 2011). Thus, Núñez-Navarro et al. (2011), comparing patients with and without purgative behavior did not observe any difference in personality traits. However, they did find higher scores on psychopathological symptomatology in patients with purging bulimia nervosa (BNp) followed by those with non-purging bulimia nervosa (BNnp), and these with patients diagnosed with binge-eating disorder (BED). They concluded that the symptoms were more severe in patients with purging behavior.
The study by Köch, Quadflieg and Manfred (2013) focused on finding the influence of purging behaviors on therapeutic improvement. These authors thought most research had concentrated on controlled studies of cognitive-behavioral intervention efficacy, while studies done in uncontrolled environments, such as outpatient or hospital care provided by healthcare services are infrequent (Turner, Marshall, Stopa, & Waller, 2015; Turner, Tatham, Lant, Mountford, & Waller, 2014; Waller et al., 2014). In general, the results showed significant improvement in psychopathology of ED, psychological functioning and psychosocial adjustment similar to the results of a systematic review done by Zöe and Kim (2014). These authors emphasized the effectiveness of outpatient treatment in reducing purging behavior.
Most studies concerning therapeutic improvement concentrate on disorders with purging behaviors, while few studies compare patients, such as restrictive anorexia nervosa (ANr), BNnp and BED, with and without purging behaviors. Thus findings are not conclusive. In some studies, no posttreatment differences are found between BNp and BNnp disorders. Concerning symptomatology, they show greater distortion of body image, anxiety about thinness and dissociative symptoms, among others, in patients with purging behaviors. Moreover, more severe affectation is observed in ANp patients than BNp (Agüera et al., 2013; Fassino et al., 2002; Muñoz, Beato, & Rodríguez, 2011; Tasca et al., 2012).
Recent studies show more treatment efficacy in concurrent psychopathology in BN than AN. Thus, a review by Mischoulon et al. (2011) emphasized that patients with ANr were less prone to recovery from major depression than those with BN. Nor were findings conclusive in determining the effectiveness of CBT for AN. Finally, Fassino et al. (2002) concluded that BN could be a protection factor as novelty seeking could facilitate motivation for change.
In summary, empirical evidence found to date on CBT provided in outpatient or hospital care suggests that there are no significant differences in the evolution of patients with purging behaviors. Few studies compare such patients with those without these behaviors, and their findings are inconclusive. In some cases no significant differences are found and in others there are indicators of better prognosis in patients with purging behaviors. From this perspective, it seems of interest to study this subject in greater depth, specifically, analyze the influence of purging behaviors on the prognosis of patients with ED treated in outpatient or hospital care units.
The general aim of this study was to find out the evolution of patients diagnosed with ED with versus without purging behaviors based on a multi-component treatment protocol adapted to the characteristics of each patient, enabling their care in an uncontrolled context such as public healthcare services. The following specific objectives were posed for this: First, evaluate improvement of specific ED symptoms (satisfaction with shape, high-risk eating behavior, drive for thinness and bulimic symptomatology), in the variables of personal development (perfectionism, self-esteem and ineffectiveness) and emotional alterations (anxiety and depression) after 30 months from start of treatment. Second, determine the variables and subgroup where treatment was most effective.
MethodThis quasi-experimental study is specifically a pre-post group design according to Montero and León (2007). A group of women was evaluated before and after receiving treatment in the natural context of clinical care in a healthcare environment.
ParticipantsThe sample was made up of 162 women with restrictive anorexia nervosa (ANr: n=35; 21.60%), purging anorexia nervosa (ANp: n=16; 9.87%), non-purging bulimia nervosa (BNnp: n=10; 6.17%), purging bulimia nervosa (BNp: n=54; 33.33%) and unspecified eating disorder (USED: n=47; 29.01%) according to DSM-IV diagnostic criteria. They received a multidisciplinary treatment in a specialized ED outpatient or hospital unit employing empirically validated techniques, in a public hospital in the Region of Castilla-La Mancha (Spain). Data were taken on their social characteristics, family and education and history. The mean age was 22 years and 11 months (M=22.90; SD=6.68; range=16-44) and the average BMI was within the parameters of normality (normal ≥18 and<25; M=21.49; SD=7.03). Many of the participants were single (58.2%), 43.2% had finished high school and 29% had gone to university. Many of the participants were over 25 (69.9%).
In this study, patients were classified in two subgroups by whether they showed purging behavior (n=87) or not (n=75) based on the diagnostic interview and Item 7 of the BITE (Bulimic Investigatory Test Edinburgh). All the patients in the purging subgroup showed vomiting behaviors and 30% of them also recurred to other types of behavior such as use of laxatives or diuretics.
Inclusion criteria. The sample was made up of women because of the exploratory nature of this study and low incidence of men. The minimum age was 16. The final and definitive criteria for inclusion were reading and filling in the informed consent document and filling in the test battery at different times in the evaluation.
InstrumentsThe demographic and clinical variables were found during the course of a direct interview. Barefoot participants were weighed on a calibrated scale and their height measured by a height calibrator.
Versions validated for Spanish samples of the Body Shape Questionnaire (BSQ) (Raich et al., 1996), Eating Attitudes Test (EAT-40) (Castro, Toro, Salamero, & Guimerá, 1991), and Eating Disorder Inventory (EDI-2) (Corral, González, Pereña, & Seisdedos, 1998) were used to evaluate the presence and severity of EDs. Validated Spanish versions of the State-Trait Anxiety Inventory (STAI) (Seisdedos, 1982) and the Beck Depression Inventory (BDI) (Vázquez & Sanz, 1999) were used to evaluate anxiety and depression emotional alterations, respectively. Purging behavior was evaluated with the Bulimic Investigatory Test (BITE) (Henderson & Freeman, 1987).
ProcedureThe 162 participants who came to a public general hospital and were diagnosed with ED were evaluated. After receiving their informed consent, they were treated in outpatient or hospital+outpatient care units according to the therapeutic requirements of each participant throughout intervention. They filled in the evaluation scales, including baseline measurements in this study (Time 1) at different times and after 30 months from start of treatment (Time 2), when patients had carried out at least one year of follow-up. The sessions were individual and in group. They received individual, group and family therapy as well as nutritional therapy and psychopharmacological treatment, adapting the multimodal treatment to the specific characteristics of each patient with special emphasis on treatments with demonstrated efficacy, that is, with empirical validity. Psychoeducation, strategies motivating to change and cognitive-behavioral (training in relaxation and activation control, in vivo and imaginary exposure and cognitive restructuring and prevention of relapse) psychotherapeutic techniques were employed. Although the treatment's design components were homogeneous (care system, modality, type of therapy, etc.), it was applied in a variable number of sessions based on ED severity and adapted to the characteristics and goals set for each patient to maximize the external validity of the therapeutic procedure. The procedure and documents used were approved by the Hospital Ethics Committee.
Statistical analysesFirst descriptive analyses were done for the entire sample of 162 patients as well as for presence or absence of purging behavior. The relationship between qualitative variables was evaluated by Chi squared test (χ2). In this case, to evaluate the effect size, the contingency coefficient (r2φ) was used with the reference values of <0.30, 0.30-0.50 and>0.50 as small, medium and large sizes, respectively (Cohen, 1992). To analyze for the existence of differences among the participants with presence or absence of purging behavior on the variables of personal development and emotional alterations on the various scales related to ED, t tests were used to compare means according to the characteristics of the sample. To evaluate the size of effect in this type of comparisons, the Cohen d was calculated using the Lipsey and Willson (2001) formula, considering the sample sizes in the two groups (presence/absence of purging behavior) and the Student's t. Reference values were the parameters mentioned above (Cohen, 1992). A multivariate variance analysis was done with the variables related to ED (BSQ, EAT-40, EDI-OD, BITE-SI) combined with the personal development characteristics (EDI-P, EDI-I) and emotional alterations (STAI-R, BDI) to analyze the existence of differences among participants with and without purging behavior as well as treatment efficacy. The effect size was evaluated by partial eta-squared (η2p) where 0.01-0.06=small effect,>0.06-0.14=medium effect and >0.14=large effect (Cohen, 1992). Furthermore, for a more exhaustive analysis of the differences found, a 2×2 mixed analysis of variance (AVAR) was done with the scores from the time condition (Time 1 or baseline versus Time 2 or at 30 months) with the within-subject variable and purging behavior condition (presence versus. absence) as the between-subjects variable. The effect size was also evaluated by partial eta-squared (η2p). All statistical analyses were done using the Statistical Package for the Social Sciences for Windows (SPSS, version 21.0).
ResultsDescriptive analysesFirst, the descriptive analyses done for the entire sample showed that body dissatisfaction, -BSQ (M=125.81; SD=38.61)-, high-risk eating behaviors, -EAT-40 (M=46.70; SD=21.69)-, and bulimic symptomatology, -BITE-SI (M=16.78; SD=8.29)-, reached clinical levels, but not drive for thinness, -EDI-OD (M=12.57; SD=6.04)-. Ineffectiveness, -EDI-I (M=11.90; SD=8.03)-, anxiety, -STAI-R (M=37.31; SD=11.54)-, and depressive symptomatology, -BDI (M=22.34; SD=9.02)- were also present at higher levels than those usually found in the normative population, but not perfectionism,- EDI-P (M=6.83; SD=4.70)-.
Between-group comparisons of descriptive variablesAt baseline (Time 1), of the five descriptive variables analyzed (age, marital status, education, number of siblings and position among siblings), significant (p≤.005) associations with presence or absence of purging behavior were found only in age (χ2=14.92; r2φ=0.29) and number of siblings (χ2=10.73; r2φ=0.24) and with a nearly medium effect size. A higher proportion of participants with purging behaviors were from 21 to 35 years old than those without, with stronger differences in the 26 to 30 age range (22.9% purging behaviors compared to 8% without). Examining the association between the number of siblings and presence or not of purging behavior, the highest percentage of participants with purging behaviors had 2 or 3 siblings; it was also among the latter, where the percentage of participants with purging behaviors was higher than those without (28.7% purging behavior compared to 24% without). Furthermore, the body mass index (BMI) was also significantly associated with purging behavior (χ2=33.53, p≤.01) with a medium effect size (r2φ=0.41), and with a higher percentage of underweight (BMI<18) (69.3%) in the group with no purging behavior.
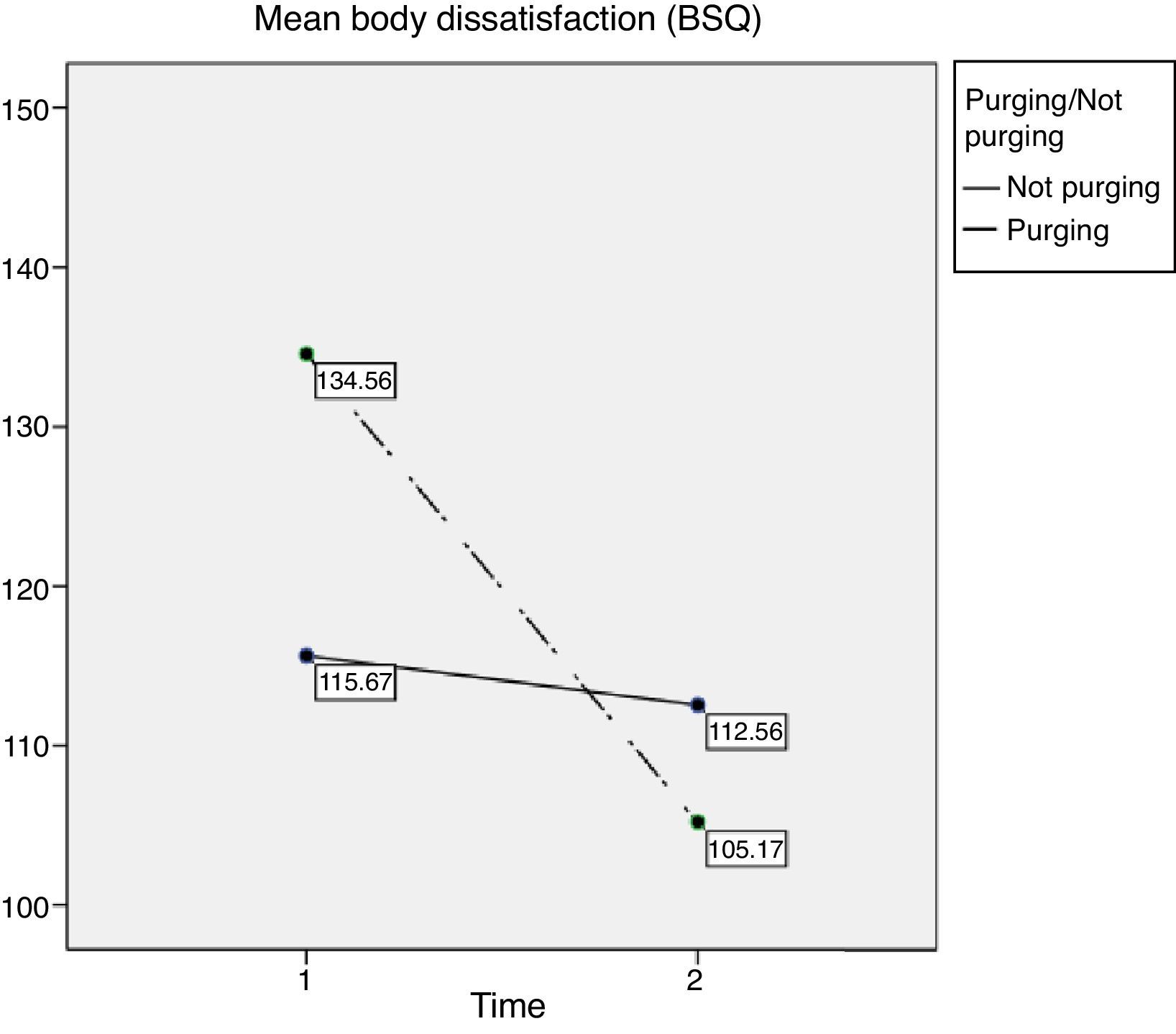
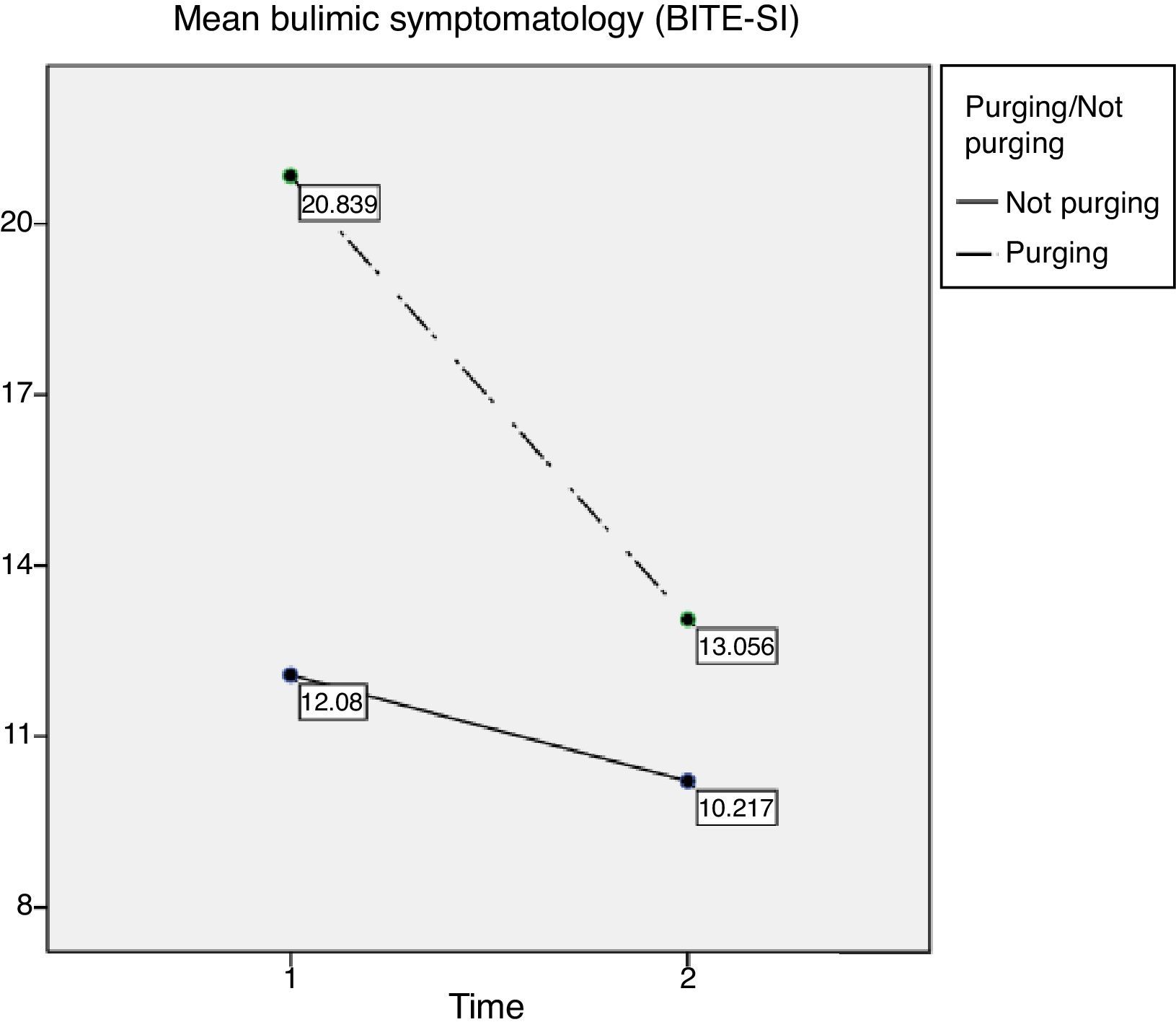
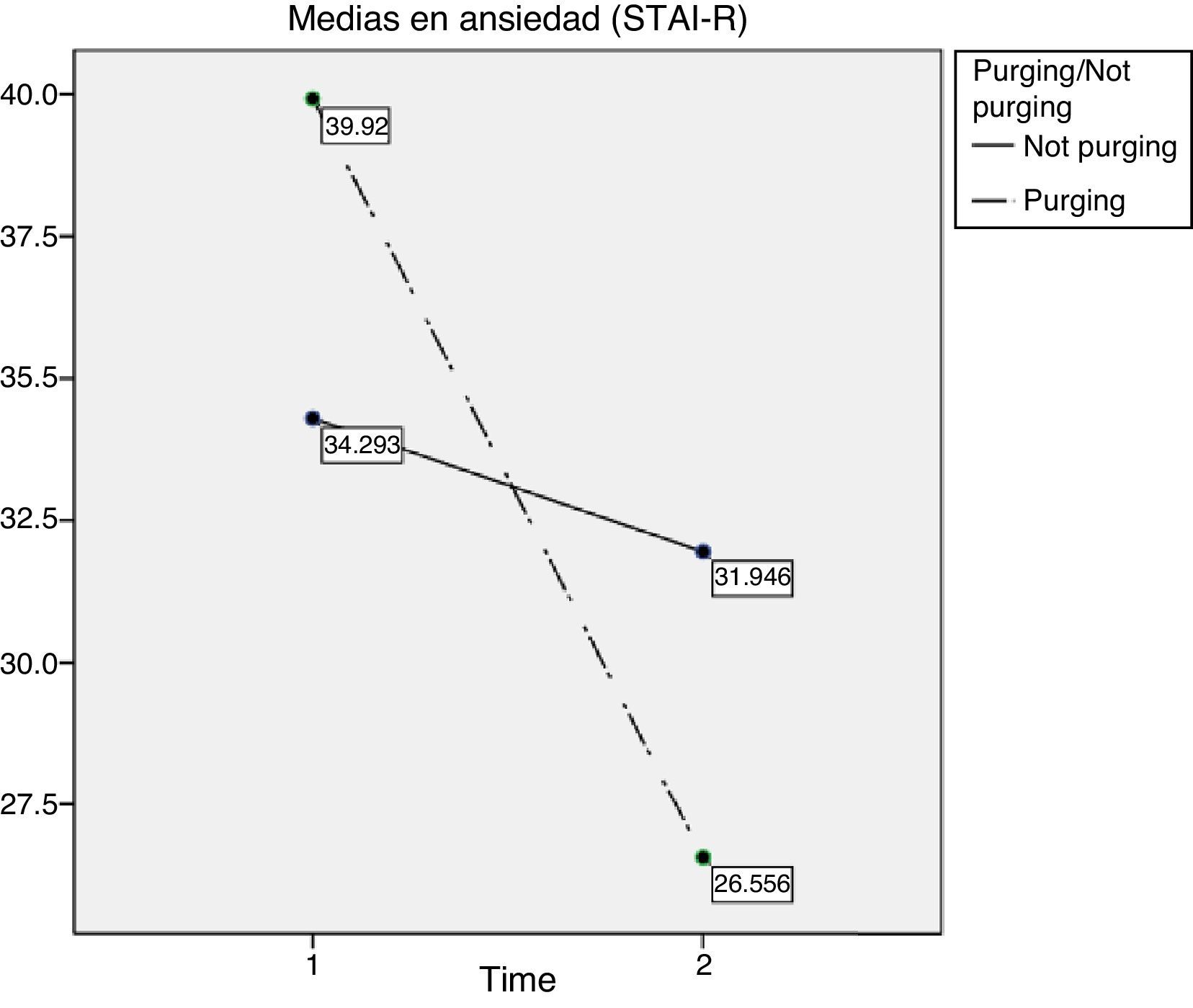
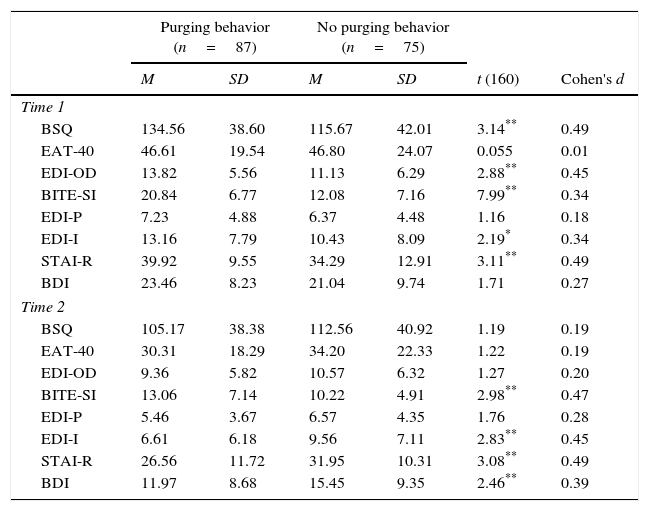
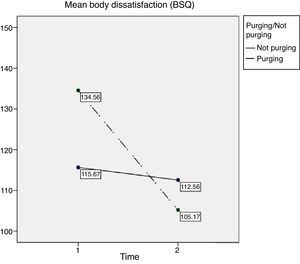
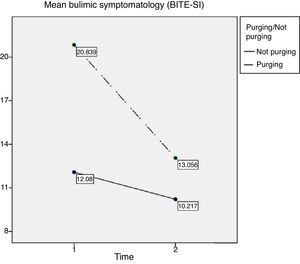
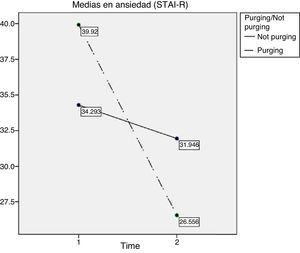
Between-group comparisons of the scalesAs may be observed in Table 1, at baseline (Time 1), the means on the ED scales with personal development and emotional alteration variables were higher in the participants with purging behaviors, except in high-risk eating behaviors, where means were similar (M=46.61; SD=19.54 versus M=46.80; SD=24.07). Compared to the participants without purging behavior, the mean scores show that the participants with purging behavior present, in addition to a more altered bulimic eating behavior pattern (M=20.84; SD=6.77 versus M=12.08; SD=7.16), more body dissatisfaction (M=134.56; SD=38.60 versus M=115.67; SD=42.01), drive for thinness (M=13.82; SD=5.56 versus M=11.13; SD=6.29), perfectionism (M=7.23; SD=4.88 versus M=6.37; SD=4.48) and ineffectiveness (M=13.16; SD=7.79 versus M=10.43; SD=8.09), anxiety (M=39.92; SD=9.55 versus M=34.29; SD=12.91) and depressive (M=23.46; SD=8.23 versus M=21.04; SD=9.74) symptomatology.
Between-group comparisons on the various scales.
| Purging behavior (n=87) | No purging behavior (n=75) | |||||
|---|---|---|---|---|---|---|
| M | SD | M | SD | t (160) | Cohen's d | |
| Time 1 | ||||||
| BSQ | 134.56 | 38.60 | 115.67 | 42.01 | 3.14** | 0.49 |
| EAT-40 | 46.61 | 19.54 | 46.80 | 24.07 | 0.055 | 0.01 |
| EDI-OD | 13.82 | 5.56 | 11.13 | 6.29 | 2.88** | 0.45 |
| BITE-SI | 20.84 | 6.77 | 12.08 | 7.16 | 7.99** | 0.34 |
| EDI-P | 7.23 | 4.88 | 6.37 | 4.48 | 1.16 | 0.18 |
| EDI-I | 13.16 | 7.79 | 10.43 | 8.09 | 2.19* | 0.34 |
| STAI-R | 39.92 | 9.55 | 34.29 | 12.91 | 3.11** | 0.49 |
| BDI | 23.46 | 8.23 | 21.04 | 9.74 | 1.71 | 0.27 |
| Time 2 | ||||||
| BSQ | 105.17 | 38.38 | 112.56 | 40.92 | 1.19 | 0.19 |
| EAT-40 | 30.31 | 18.29 | 34.20 | 22.33 | 1.22 | 0.19 |
| EDI-OD | 9.36 | 5.82 | 10.57 | 6.32 | 1.27 | 0.20 |
| BITE-SI | 13.06 | 7.14 | 10.22 | 4.91 | 2.98** | 0.47 |
| EDI-P | 5.46 | 3.67 | 6.57 | 4.35 | 1.76 | 0.28 |
| EDI-I | 6.61 | 6.18 | 9.56 | 7.11 | 2.83** | 0.45 |
| STAI-R | 26.56 | 11.72 | 31.95 | 10.31 | 3.08** | 0.49 |
| BDI | 11.97 | 8.68 | 15.45 | 9.35 | 2.46** | 0.39 |
Note. BSQ=Body Shape Questionnaire; EAT-40=Eating Attitude Test; EDI-OD=Eating Disorder Inventory, Drive for thinness; BITE-SI=Bulimic lnvestigatory Test Edinburgh, Symptom subscale; EDI-P=Eating Disorder Inventory, Perfectionism; EDI-I=Eating Disorder Inventory, Ineffectiveness; STAI-R=State-Trait Anxiety Inventory; BDI=Beck Depression Inventory.
After 30 months from start of treatment (Time 2), except in bulimic symptomatology (M=13.06; SD=7.14 versus M=10.22; SD=4.91), it was observed that means of participants with purging behavior fell more on all seven scales than the group without purging behavior, especially in bulimic symptomatology (d=1.26), body dissatisfaction (d=0.49), anxiety (d=0.49), drive for thinness (d=0.45) and ineffectiveness (d=0.34) (Table 1).
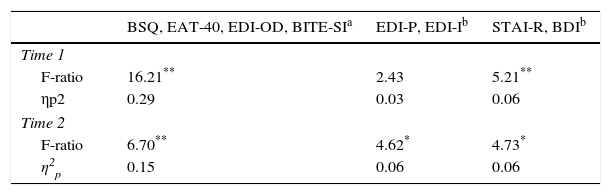
Between-group comparisons in overall measures and treatment efficacyAt baseline (Time 1) significant differences were observed on the scales related to eating behavior (F(4, 157)=16.21; p<.01; Wilks’ Lambda=0.71; η2p=0.29) and emotional alterations (F(2, 159)=5.21; p<.01; Wilks’ Lambda=0.94, η2p=0.06) (Table 2). At 30 months from start of treatment, significant differences remained in the combined scales related to ED (F(4, 157)=6,70; p<.01; Wilks’ Lambda=0.85; η2p=0.15) and emotional alterations (F(2, 159)=4,73; p=.01; Wilks’ Lambda=0.94; η2p=0.06), with a smaller effect size than baseline (Time 1). There were also differences in the combined scales related to the personal development characteristics (F(2, 159)=4.62; p=.01; Wilks’ Lambda=0.95, η2p=0.06). Furthermore, in the results for each of the scales considered individually, differences were observed in anxiety symptomatology (t(160)=3.08; p<.01; d=0.49), bulimic symptomatology (t(160)=2.98; p<.01; d=0.47), ineffectiveness (t(160)=2.83; p=.01; d=0.45) and depressive symptomatology (t(160)=2.46; p=.02; d=0.39) (Table 2).
Multivariate analysis of variance and effect sizes for ED, personal development and emotional alteration variables.
| BSQ, EAT-40, EDI-OD, BITE-SIa | EDI-P, EDI-Ib | STAI-R, BDIb | |
|---|---|---|---|
| Time 1 | |||
| F-ratio | 16.21** | 2.43 | 5.21** |
| ηp2 | 0.29 | 0.03 | 0.06 |
| Time 2 | |||
| F-ratio | 6.70** | 4.62* | 4.73* |
| η2p | 0.15 | 0.06 | 0.06 |
Note. BSQ=Body Shape Questionnaire; EAT-40=Eating Attitude Test; EDI-OD=Eating Disorder Inventory, Drive for thinness; BITE-SI=Bulimic lnvestigatory Test Edinburgh, Symptom subscale; EDI-P=Eating Disorder Inventory, Perfectionism; EDI-I=Eating Disorder Inventory, Ineffectiveness; STAI-R=State-Trait Anxiety Inventory; BDI=Beck Depression Inventory.
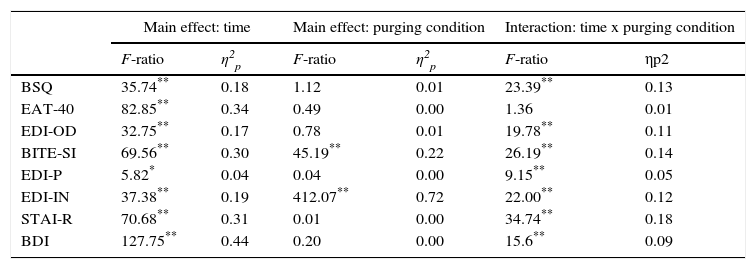
Analyzing the differences detected more exhaustively in a 2×2 mixed analysis of variance, treatment effectiveness was observed in all of the variables, especially in depressive symptomatology (F(1, 160)=127.75; p<.01; η2p=0.44), high-risk eating behaviors (F(1, 160)=85.85; p<.01; η2p=0.34), anxiety (F(1, 160)=70.68; p<.01, η2p=0.31) and bulimic symptomatology (F(1, 160)=69.56; p<.01; η2p=0.30), which were the variables with the largest effect sizes (Table 3).
2×2 Mixed Analysis of Variance (AVAR).
| Main effect: time | Main effect: purging condition | Interaction: time x purging condition | ||||
|---|---|---|---|---|---|---|
| F-ratio | η2p | F-ratio | η2p | F-ratio | ηp2 | |
| BSQ | 35.74** | 0.18 | 1.12 | 0.01 | 23.39** | 0.13 |
| EAT-40 | 82.85** | 0.34 | 0.49 | 0.00 | 1.36 | 0.01 |
| EDI-OD | 32.75** | 0.17 | 0.78 | 0.01 | 19.78** | 0.11 |
| BITE-SI | 69.56** | 0.30 | 45.19** | 0.22 | 26.19** | 0.14 |
| EDI-P | 5.82* | 0.04 | 0.04 | 0.00 | 9.15** | 0.05 |
| EDI-IN | 37.38** | 0.19 | 412.07** | 0.72 | 22.00** | 0.12 |
| STAI-R | 70.68** | 0.31 | 0.01 | 0.00 | 34.74** | 0.18 |
| BDI | 127.75** | 0.44 | 0.20 | 0.00 | 15.6** | 0.09 |
Note. BSQ=Body Shape Questionnaire; EAT-40=Eating Attitude Test; EDI-OD=Eating Disorder Inventory, Drive for thinness; BITE-SI=Bulimic lnvestigatory Test Edinburgh, Symptom subscale; EDI-P=Eating Disorder Inventory, Perfectionism; EDI-I=Eating Disorder Inventory, Ineffectiveness; STAI-R=State-Trait Anxiety Inventory; BDI=Beck Depression Inventory.
Differences were observed between participants with and without purging behavior, especially in effectiveness (F(1, 160)=412.07; p<.01; η2p=0.72) and bulimic symptomatology (F(1, 160)=45.19, p<.01; η2p=0.22). Finally, the interaction effect between with and without the purging condition and time (evaluations at Time 1 and Time 2) was observed to be significant in seven out of eight variables analyzed. Considering the effect size, the interaction was significant in anxiety (F(1, 160)=34,74; p<.01; η2p=0.18), bulimic symptomatology (F(1, 160)=26.19; p<.01; η2p=0.14), ineffectiveness (F(1, 160)=22.00; p<.01; η2p=0.12), body dissatisfaction (F(1, 160)=23.39; p<.01; η2p=0.11), drive for thinness (F(1, 160)=19.78; p<.01; η2p=0.11), depressive symptomatology (F(1, 160)=15.26; p<.01; η2p=0,09) and perfectionism (F(1, 160)=9.15, p<.01; η2p=0.05). After 30 months from start of treatment (Time 2), when means of participants with and without purging behavior were compared, the decrease in each variable, considered the effect of intervention, was greater in one group than the other. Specifically, the treatment effect was stronger in patients with purging behavior. The figures below show the effect for the variables with the largest effect sizes: body dissatisfaction (Figure 1), bulimic symptomatology (Figure 2) and anxiety (Figure 3).
Two objectives were posed in this study. The first was to find out the improvement in specific ED eating symptoms, personal development variables and emotional alterations after 30 months from start of a multicomponent treatment in women diagnosed with ED with and without purging behavior. At start of intervention or baseline (Time 1), body dissatisfaction, high-risk eating behavior and bulimic symptomatology were on clinical levels. Ineffectiveness, anxiety and depressive symptomatology levels were also above usual levels in the normative population. Furthermore, the participants with purging behavior also had a more altered bulimic eating behavior pattern, more body dissatisfaction, drive for thinness, perfectionism and ineffectiveness, anxiety and depressive symptomatology. The effect was also greater considering these variables together, that is, as an overall index, both in variables related to ED (drive for thinness+high-risk eating behavior+bulimia+body dissatisfaction), and personal development characteristics (perfectionism+ineffectiveness) and emotional alterations (anxiety+depressive symptomatology). These results are consistent with findings by Tasca et al. (2012), who found that purging patients (BNp and ANp) had more anxiety about thinness and body dissatisfaction than ANr patients. Núñez-Navarro et al. (2011) also analyzed patients with BNp, BNnp and ED purging disorders. Their results showed that although there were no differences in personality traits, the BNp patients showed higher scores in psychopathological symptomatology than those with BNnp and ED, and concluded that symptoms were more severe in purging patients.
Concerning changes after intervention, previous findings have shown that CBT improves anxiety and depressive symptoms, drive for thinness, body dissatisfaction, and bulimic symptomatology in ED. However, in personal development measures, such as perfectionism and ineffectiveness, results observed were more moderate (Turner et al., 2014, 2015; Waller et al., 2014; Zöe & Kim, 2014).
In line with previous research, in this study, treatment led to improvement after 30 months from startup (Time 2) in participants with and without purging, with a differential effect between the two groups. Specifically, participants with purging behavior showed less resistance to change. In other words, decrease in means in the seven measures evaluated separately was observed to be greater in purging patients than in the group without purging behavior, except for bulimic symptomatology (which improved, but scores were still higher). These data are in line with what has been reported by authors such as Mischoulon et al. (2011) concerning the efficacy of psychological treatments in BN and AN. However, as mentioned above, there are few studies comparing treatment evolution in patients with and without purging. Muñoz et al. (2011) analyzed evolution of a group of 54 patients diagnosed with ANr, ANp, BNnp and BNp after one year of treatment, and found improvement in self-esteem and ED-specific psychopathology (increase in BMI and lower scores on the BSQ as well as decreased dissociative symptoms). Fassino et al. (2002), who analyzed evolution of patients with ANr who received treatment at an ED center, found that patients who did not improve after over a year of treatment were characterized by high levels of asceticism and fear of maturity and lower novelty seeking. Those who improved had gone through an episode of BN, concluding that the BN episodes, associated with more novelty seeking, could be a driver or strategy for change, and therefore, have positive effects for improvement.
The second objective of this study was to determine the variables and group of participants with the best effect of treatment after 30 months from start (Time 2). It was observed that the effect of treatment over time was greater in purging participants, and that the variables with the largest effect size were body dissatisfaction and anxiety symptomatology, in addition to the bulimic symptomatology itself. These results agree with the findings of authors such as Turner et al. (2015), who observed a significant improvement in ED psychopathology, emotional alterations and psychosocial adjustment in patients at a national healthcare ED center in in the United Kingdom. Furthermore, the attitudes and high-risk eating behavior that changed in the first sessions were maintained at the end of treatment. However, in this study, the proportion of participants with binge-eating or induced vomiting was not evaluated. In fact, the effect size of the changes at the end of treatment was high for all the variables evaluated except for use of vomiting and laxatives, which was medium size. The authors point out this limitation for comparing their results to findings in other studies. Similarly, this study had a limitation in not having considered the participants who in addition to vomiting used some other type of purging behavior as an independent group to evaluate the effect this other type of behavior could have on prognosis and recovery from the illness.
Continuing with the limitations, it should be mentioned that although the treatment is homogeneous in its design, it was applied in a variable number of sessions depending on ED severity, slightly impeding the replicability of the study. However, the characteristics of the multicomponent treatment adapted to the characteristics of each patient maximized the external validity of the therapeutic procedure, considering that it is a clinical intervention based on treatments that have shown their efficacy in ED, but designed to be implemented in daily clinical practice, as argued by Turner et al. (2015).
In brief, it may be said that the findings of this study are consistent with the contributions made in previous research in which the efficacy of interventions based on cognitive-behavioral therapy has been demonstrated in uncontrolled environments. In addition to this, our findings enable another step to be taken in the attempt to explain what patient characteristics have to be taken into consideration in planning and designing effective interventions. Specifically, the role of purging behavior, especially vomiting, in the evolution and prognosis with this type of intervention, since the findings to date would indicate that these behaviors, understood as inadequate coping strategies, could actually be a protective factor for therapeutic change.
Finally, it would be of interest to widen the study of these variables to the male population, since recent research, such as the studies by Dakanalis et al. (2015, 2016), have demonstrated the importance that the variables studied here, such as body dissatisfaction, negative affect and binge-eating have in the development and maintenance of ED in men. This would make it possible to find out whether the practical implications derived from this study could e extrapolated to the design of intervention studies for that group.