Con el objetivo de investigar la capacidad predictiva de características psicopatológicas y sociodemográficas sobre el diagnóstico del trastorno obsesivo compulsivo (TOC) clínico y subclínico, y observar las posibles asociaciones entre estas variables y los dos tipos de diagnósticos, 1.514 escolares españoles con edades comprendidas entre 8 y 12 años completaron cuestionarios de riesgo de trastornos emocionales (obsesivo-compulsivos, de ansiedad y de depresión). Al año siguiente, 562 sujetos (grupo de riesgo y grupo sin riesgo) fueron re-evaluados realizándose el diagnóstico de TOC o de TOC subclínico. De ellos, 20 sujetos presentaron TOC clínico y 46 presentaron TOC subclínico. La ansiedad de separación y los síntomas somáticos resultaron ser buenos predictores para el diagnóstico de TOC clínico, mientras que la preocupación obsesiva fue un predictor significativo para el TOC subclínico. El TOC clínico está asociado a un nivel socioeconómico bajo y a síntomas de orden/comprobación/contaminación y el TOC subclínico se relaciona significativamente con manifestaciones de hiperactividad e impulsividad, preocupaciones obsesivas, supersticiones y compulsiones mentales. La detección precoz y el seguimiento de los síntomas ansiosos y de obsesividad en los niños pueden ser muy importantes para la prevención de trastornos como el TOC.
We assessed the presence of emotional disorders (obsessive-compulsive, anxiety and depressive) in 1,514 Spanish non-referred children (8-12 years old) to investigate the predictive ability of psychopathological and socio-demographic characteristics, and identify which of these were possible correlates for clinical obsessive-compulsive disorder (OCD) and subclinical OCD. At one year later, 562 subjects (risk group and without risk group) were re-assessed and we established the OCD diagnoses or the subclinical OCD diagnoses. We found that 20 participants presented clinical OCD and 46 participants presented subclinical OCD. Somatic and separation anxiety symptomatology were good predictors for clinical OCD, and obsessive concern was a predictor for subclinical OCD. Clinical OCD was associated with order/checking/pollution symptoms and with a lower socioeconomic status (SES). Subclinical OCD was associated with hyperactive and impulsive manifestations, obsessive concern, and superstition/mental compulsion. An early detection and the follow-up of anxiety or obsessive symptoms in children may be important for preventing the course of OCD.
Obsessive-compulsive disorder (OCD) is considered one of the most common serious mental illnesses (Heyman, Mataix-Cols, & Fineberg, 2006). According to some authors, it is indisputable that a significant number of individuals in the community suffer from OCD (Eisen et al., 2010; Stewart et al., 2004) and that they are at risk of experiencing other psychiatric conditions (Marcks, Weisberg, Dyck, & Keller, 2011). In addition, Micali et al. (2010) state that paediatric OCD can be a chronic condition that persists into adulthood, so early recognition and treatment might prevent chronicity. According to Stewart et al. (2004), OCD is now being reported to be more prevalent in the paediatric population than previously, when it was considered rare, and it is increasingly becoming the focus of interest in child and adolescent psychiatry because it is a condition with important implications for social functioning, school and family and quality of life (Eisen et al., 2006; Lochner et al., 2003). Several epidemiological studies in community samples of children and adolescents have reported prevalence ranging from 0.1% to 4% (Douglass, Moffitt, Dar, McGee, & Silva, 1995; Heyman et al., 2001; Lewinsohn, Hops, Roberts, Seeley, & Andrews, 1993) and in a recent study conducted in a Spanish community sample we found an estimated prevalence of OCD of 1.8% (Canals, Hernández-Martínez, Cosi, & Voltas, 2012).
Although plenty is known about how to treat OCD (Olatunji, Davis, Powers, & Smits, 2013; Rosa-Alcázar, Sánchez-Meca, Gómez-Conesa, & Marín-Martínez, 2008), there is little data regarding the risk factors that precede OCD. This disorder has a complex aetiology involving both genetic and environmental factors; the genetic causes of OCD are largely unknown despite the identification of several promising candidate genes and linkage regions (Mathews et al., 2012). In relation to the environmental factors, Grisham et al. (2011) have associated adverse prenatal, perinatal or postnatal experiences with an increased risk of developing obsessive-compulsive (OC) symptoms in adulthood. Also those authors found that a more difficult temperament in early childhood was associated with OCD. In other terms, the OCD may be caused by an autoimmune response to streptococcal infections (Paediatric Autoimmune Neuropsychiatric Disorder Associated with Streptococcal Infections, PANDAS) (Swedo et al., 1998).
In terms of socio-demographic factors, being male seems to be a risk factor in early onset cases (Walitza, Melfsen, Jans, & Zellmann, 2011) and although it has been poorly studied in children and adolescents, lower socioeconomic status (SES) has also been related to OCD (Heyman et al., 2001). In adults economic impairment and unemployment have been related to OCD (Grabe et al., 2000; Himle et al., 2008). Academic performance has also been related to OCD although the findings are still mixed as yet. Whereas Himle et al. (2008) found that adults with OCD had lower educational success because their academic performance began to suffer when they were children; others such as Degonda, Wyss, and Angst (1993) found that subjects with OC symptoms differed from controls by exhibiting higher educational levels.
Furthermore, as we have mentioned, the relationships between OCD and other psychiatric conditions are highly prevalent among children and adolescents. In this regard, we have found high rates of comorbidity for OCD in Canals, Hernández-Martínez, Cosi, and Voltas (2012), particularly in relation to anxiety and depression disorders. De Mathis et al. (2012) studied the impact of the first manifested psychiatric diagnosis on the clinical development of OCD using adult OCD patients. They found that participants who reported antecedent symptoms of separation anxiety were shown to develop further additional anxiety and somatoform disorders such as somatization and more severe current depressive symptoms. Likewise they found that patients presented a worsening course of OCD if they had first been diagnosed with attention deficit hyperactivity disorder (ADHD). In fact it is known that ADHD symptoms in adolescence predicted more OCD symptoms in early adulthood (Peterson, Pine, Cohen, & Brook, 2001).
Other authors found a relationship between OCD and eating disorders (Kim, Ebesutani, Wall, & Olatunji, 2012), particularly those disorders that present high body mass index (BMI), such as binge-eating disorder (Claes, Nederkoorn, Vandereycken, Guerrieri, & Vertommen, 2006). Some studies have demonstrated relationships between appetite regulating peptides and OC symptoms (Hillemacher et al., 2007), so it is difficult to know if having high BMI may be a cause or consequence of the OCD and eating disorders.
Recently, Taylor (2011) confirmed that OC symptomatology has a complex etiological architecture, which does not appear to be adequately captured yet, and so our purpose was to identify factors that could contribute to the early development of this disorder or to ascertain which variables could be related to OCD regardless of the genetic or other type of biological risk factors, because this is essential for the development of prevention and treatment programs. For this reason, our main aim was to carry out a follow-up epidemiological study to observe the predictive ability of psychopathological and socio-demographic characteristics and possible correlates for two levels of severity of OCD: clinical OCD and subclinical OCD.
Method
Participants
2,023 children were invited to participate in a follow-up study of emotional disorders. The children came from 13 primary schools in Reus (Catalonia, Spain) randomly chosen from the towns' state schools and state-subsidized private schools. The study began in 2007 and 1,514 children with a mean age of 10.23 (SD = 1.23) agreed to participate (720 boys and 794 girls). Of these 1,514 subjects, a total of 39.5% belonged to families with low SES, 42.5% to families of medium SES and 18% to families of high SES. 87.5% of the sample was born in Spain, and 85.9% belonged to a nuclear family. One year later, in the second stage, 562 subjects (254 boys and 308 girls) between 9 and 13 years of age (M = 11.25; SD = 1.04) were selected either as subjects at risk of emotional disorders (41.8%) or as belonging to a control group with no risk (58.2%). The attrition of the risk subjects from the 1st to the 2nd phase was 16%. If a control subject was invited to participate in the 2nd phase and declined, we selected another participant with similar characteristics from the 1st phase.
Instruments
• Leyton Obsessional Inventory-Child Version Survey (LOICV; Berg, Whitaker, Davies, Flament, & Rapoport, 1988) is a self-report of a 20-item questionnaire that aims to determine the presence or absence (using in the item Yes/No) of a number of obsessive preoccupations and behaviours, and that includes a rating of interference with personal functioning for each positive response (range 0-3, no interference-interferes a lot). The internal consistency of the Spanish version is good (Cronbach's α = .90) and is composed of three factors called Order/ checking/pollution (7 items; Cronbach's α = .82), Obsessive concern (7 items¸ Cronbach's α = .81) and Superstition/mental compulsion (6 items; Cronbach's α = .77). This questionnaire has been proven to be a valid screening instrument for assessing OCD or OC symptoms in children and adolescents (Canals, Hernández-Martínez, Cosi, Lázaro, & Toro, 2012).
• Screen for Childhood Anxiety and Related Emotional Disorders (SCARED; Birmaher et al., 1997). The SCARED is a self-report questionnaire that assesses DSM-IV anxiety disorder symptoms in children and adolescents from 8 to 18 years old. It consists of 41 items, and children are asked the frequency of each symptom on a 3-point-scale: 0 (almost never), 1 (sometimes), 2 (often). The internal consistency of the Spanish version is good (Cronbach's α = .86) and is composed of 4 factors called Somatic/panic (12 items; Cronbach's α = .78), Social phobia (7 items; Cronbach's α = .69), Generalized anxiety (9 items; Cronbach's α = .69), and Separation anxiety (13 items, Cronbach's α = .70) (Vigil-Colet et al., 2009).
• Children's Depression Inventory (CDI; Kovacs, 1992) is a 27-item, self-report, symptom-oriented scale suitable for young people aged 7 to 17. The CDI is sensitive to changes in depressive symptoms over time, and is a useful index of the severity of the depressive syndrome. The Spanish version has demonstrated good internal consistency in community and clinical samples (Cronbach's α = .81 to Cronbach's α = .85) (Figueras, Amador-Campos, Gómez-Benito, & Del Barrio, 2010).
• Child Symptom Inventory (CSI-4; Gadow & Sprafkin, 1998) is a screening instrument based on DSM-IV criteria. The parent version used in this study contains 97 items with a 4-point response format. There are two scoring procedures: symptom count (categorical) and symptom severity (dimensional). For the categorical correction, a specific symptom is considered to be a clinically relevant problem if it is rated as occurring often or very often, whereas the dimensional correction is simply the sum of the item scores for a particular symptom category. The CSI-4 has been demonstrated to be valid (Sprafkin, Gadow, Salisbury, Schneider, & Loney, 2002) and the Spanish version of CSI-4 has shown excellent internal consistency (Cronbach's α = .99) (Angulo et al., 2010).
• Mini-International Neuropsychiatric Interview for Kids (MINI-Kid; Sheehan et al., 1998) is a structured diagnostic interview for children from 6 to 17 years old based on DSM-IV and ICD-10 psychiatric disorders. It is a short and accurate instrument for diagnosing 23 axis I disorders. Interrater and test-retest Kappa were substantial to almost perfect (.64-1) for all individual MINI-Kid disorders except dysthymia. For OCD the interrater test kappa was .94 and the retest Kappa was .75. The interview takes approximately 30 minutes to administer. The reliability and validity of MINI-Kid has recently been demonstrated (Sheehan et al., 2010). OCD were assessed as well as depressive, bipolar, anxiety, tic, psychotic, eating and adjustment disorders and disruptive (ADHD, and conduct) disorders. The OCD diagnostic agreement (Kappa index) between the MINI-Kid and the LOI-CV was .45.
• Anthropometry, weight and height were evaluated and we obtained the BMI.
• In order to assess the socio-demographic characteristics of the sample, a socio-demographic questionnaire designed for this study was used. The children answered questions about age, gender, place and date of birth, family type, occupation of parents and other subjects. To assess academic performance, teachers were asked by one question about the children's academic performance with three response options: below average, average or above average. SES was determined using the Hollingshead index (Hollingshead, 2011). This index allows the social status of each individual to be determined by categorizing his or her occupation into one of nine categories (from unskilled work to highly skilled work) and his or her level of education into one of seven categories (from non-completed primary education to completed higher education). The status score is estimated by multiplying the occupation scale value by a weight of five and the education scale value by a weight of three and then combining the two scores. For this study, we determined family SES by combining the data obtained from the father and the mother. The scores range from 0 to 66, therefore, to obtain three categories (low, medium and high) we considered scores lower than 22 to be low SES, scores between 23 and 44 to be medium, and scores over 44 to be high.
Procedure
Before beginning the study, permission from the Department of Education of the Catalan Government was obtained. Then we selected a representative sample of subjects. Cluster sampling was conducted by randomly selecting a set of 13 schools (7 state schools and 6 state-subsidized private schools) from a total of 26 schools and from all five representative areas of Reus, Spain (a medium-sized town of 100,000 inhabitants). We then contacted the 13 school boards, all of whom agreed to participate. After that, we sent all parents a letter to inform them about the study and to ask for their written informed consent. A two-phase epidemiological study design was used. In the 1st phase we assessed the anxiety symptoms (SCARED), depressive symptoms (CDI), OC symptoms (LOI-CV), and the socio-demographic data of 1,514 subjects. This data was collected using a questionnaire designed for this study in which we asked children about their parents' jobs, family structure and other socio-demographic variables. Over the following academic year, the 2nd phase was conducted. A subsample of subjects at high risk of emotional and obsessive-compulsive disorders and a subsample of control subjects at low risk paired by age, gender and school were selected. High risk status was determined when the subject in the 1st phase obtained a high score in the SCARED and/or in the CDI and/or in the LOI-CV. In this second stage, the MINI-Kid was administered and the SCARED, the CDI and the LOI-CV were re-administered. The interviews were administered to the children on the same day or during the week after the questionnaires were completed and the interviewers were blind to the test results. To obtain diagnoses, data from a psychopathological test completed by the students' parents (CSI-4) were taken into account, and when researchers had questions, parents were telephoned to obtain more information. When the child met the full criteria for OCD diagnosis according to the DSM-IV, clinical OCD was assigned, and when the child met all criteria for OCD diagnosis except the criteria of interference, subclinical OCD was assigned. So, 20 subjects presented OCD diagnosis, and 46 subjects presented subclinical OCD diagnosis. The parents of children, who were diagnosed with any disorder, were notified about it by telephone.
The participants completed the questionnaires in groups of three or four subjects. Professional child psychologists gave the children instructions on how to answer the surveys and helped them during the session. The MINI-Kid was individually administered by these same child psychologists, who had been trained to administer the interview until they agreed on the diagnoses in 90% of the cases.
Data analysis
To examine the risk factors, stepwise logistic regression models were used. Before performing the regression models, collinearity between the variables were assessed by computing Pearson correlations between the candidate variables to enter in the model. The LOI-CV total score was collinear with LOI-CV factors, and the SCARED total score was also collinear with the SCARED factors, so the SCARED and LOI-CV factors were selected instead of the total scores. The correlation between the SCARED and the LOICV factors for the 1st and 2nd phases were below .5 and were therefore not considered collinear.
The regression models were performed in two steps. In the first step the socio-demographic, anthropometric and psychopathological variables collected in the 1st phase (LOI-CV factor scores, SCARED factor scores, CDI total score, BMI, SES, age, gender, family type, and birth place) were considered, and in the second step the academic performance and all the psychopathological variables collected in the 2nd phase (LOI-CV factor scores, SCARED factor scores, CDI total score, CSI-4 scores related to Disruptive Behavior Disorders such as Attention Deficit Hyperactivity Disorder-Inattentive (ADHD-I), Attention Deficit Hyperactivity Disorders-Hyperactive-Impulsive (ADHD-HI), Oppositional Defiant Disorder (ODD), Conduct Disorder (CD), and Generalized Developmental Disorder (GDD) were added to the first step variables.
The Bonferroni correction was applied to control the increase in type I error caused by multiple comparisons, which meant that the level of significance used was .01. The data were analyzed using the SPSS 19.0.
Results
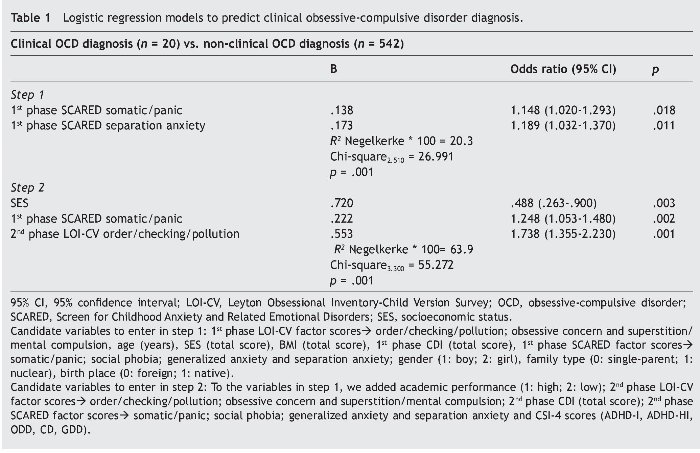
Logistic regression models were conducted to examine whether socio-demographic and psychopathological factors predicted clinical OCD or subclinical OCD diagnoses. As regards the clinical OCD diagnosis (see Table 1), we used the psychopathological, the socio-demographical and the anthropometrical data collected in the 1st phase to step 1, and we observed that somatic/panic and separation anxiety factors of the SCARED were good predictors. Step 1 explained 20.3% of the OCD diagnoses. We added the psychopathological data (emotional data from the child and behavioural data from the parents) and the academic performance obtained in the 2nd phase to step 2, which accounted for 63.9%, and we found that the best related factors were the SES, the somatic/panic factor of the SCARED administered in the 1st phase, and the score in the order/checking/pollution factor of the LOI-CV administered in the 2nd phase.
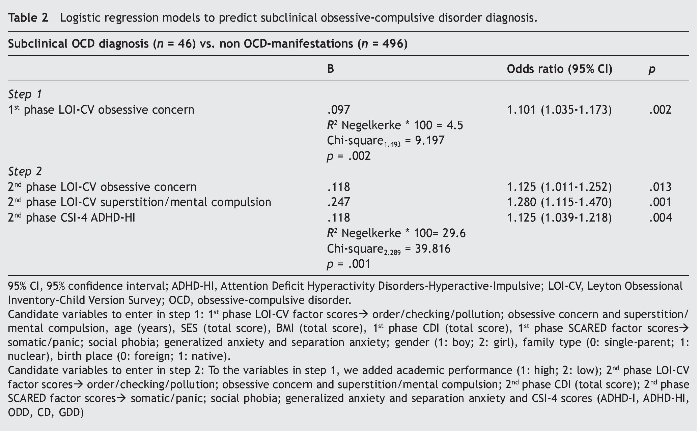
When we performed the logistic regression models for the subclinical OCD diagnosis (see Table 2), we found that the model explained 4.5% of the subclinical OCD and that the best predictor in step 1 was the obsessive concern factor of the LOI-CV. When we introduced the 2nd phase variables (step 2), the obsessive concern and the superstition/mental compulsion factors of the LOI-CV administered in the 2nd phase were significantly related to the subclinical OCD and, moreover, we could observed that the ADHD-HI score was a significant correlate with the subclinical OCD. The explained variance increased to 29.6%.
Discussion
The objective of this study was to examine the possible ability of psychopathological and socio-demographic characteristics to predict the subsequent diagnosis of early childhood clinical OCD or subclinical OCD, and there have been few studies in this area and very few that have used children from community samples. Moreover we wanted to observe the possible relation between some of these characteristics and the two types of diagnoses. These results provide important evidence that has clinical implications; the risk factors associated with subclinical OCD, either as predictors or related factors, are obsessive symptoms such as obsessive concern or superstition, whereas factors that could predict or that were related to clinical OCD were anxiety symptoms. Therefore, we suggest that subclinical OCD children present a pattern of obsessiveness and subjects with a more severe OCD diagnosis have previously present a pattern of anxiety symptoms. We also believe that it is interesting to take into account the less severe form of OCD because it could be a possible indicator of long term clinical OCD. Alternatively, the subjects could present subclinical OCD symptoms during the prospective period because full remission is rare, which is consistent with the view of OCD as a chronic and persistent disorder (Eisen et al., 2010).
In agreement with the results showed in this study, Brynska and Wolanczyk (2005) found more obsessive symptoms in the subclinical OCD group than compulsive symptoms. The most common obsessions were a fear of saying certain things, which can be linked to the obsessive concern factor, and obsessive symptomatology, such as magical thoughts or lucky/unlucky numbers, which are symptoms that can be related to the superstition/mental compulsion factor. On the other hand, we know that order/checking/pollution as a manifestation of OC is more severe, and this may be the reason why this type of symptom was more highly related to clinical rather than subclinical OCD in our study. These results also support those of Brynska and Wolanczyk (2005), who found in subjects with clinical OCD that the most frequent compulsions were checking, ordering and washing and cleaning. In addition, our results have shown that some anxious symptoms such as somatic/panic and separation anxiety could be positive predictors of clinical OCD. These data are consistent with those found in adults by Cath, Van Grootheest, Willemsen, Van Oppen, and Boomsma (2008), which supported the hypothesis that somatic was one of the major complaints and which showed the highest scale scores for somatic complaints in concordant high monozygotic pairs of twins with OC symptoms. Furthermore, Storch, Merlo et al.(2008) observed that somatic symptoms were highly prevalent among young people with OCD and had a significant impact on the clinical presentation of the disorder. In this regard, Zolog et al. (2011) found that somatic complaints were frequently associated with emotional problems and in our study somatic complaints are previous manifestations of OCD. On the other hand, data showing that separation anxiety symptomatology is a predictor of OCD supports the data of Ballesteros and Ulloa (2011), who found that OCD is frequently comorbid with anxiety disorders such as separation anxiety, and the data of Kossowsky, Wilhelm, Roth, and Schneider (2012), who found that separation anxiety disorder (SAD) is one of the most common anxiety disorders in childhood and is highly predictive of adult anxiety disorders. In this regard, Mroczkowski et al. (2011) stated that SAD usually has onset earlier than OCD and may influence the clinical course of OCD. Furthermore, worries that children with separation anxiety have can take on obsessional qualities and it can sometimes be difficult to distinguish between SAD and OCD. Moreover Mroczkowski et al. (2011) also concluded that this kind of anxiety could be correlated with adult emotional disorders, including panic disorder and major depression. On the other hand, the relation found in our study between OCD and the most common anxiety symptoms in children corroborate the classification of OCD as an anxiety disorder.
Although there are studies suggesting that levels of depression may be the product of OC symptoms (Storch et al., 2012), this is not reflected in our results, which means that depressive symptoms may be a more long term consequence for children who have suffered OCD. On the other hand, our results did not show any relation between OCD and age, gender, birth place or family type. The absence of any relation may indicate that socio-cultural factors do not influence OCD, as stated by Himle et al. (2008).
Regarding the remaining factors, despite the known relationship between OCD and eating problems (Kim et al., 2012) we found no significant results indicating that the high BMI was a risk factor for OCD. Our data also did not support the association between OCD and academic performance as suggested by Himle et al. (2008). However, in their sample Heyman et al. (2001) found that subjects belonging to lower socioeconomic classes presented higher rates of OCD, and this was in keeping with our results, which showed a relation between lower SES and clinical OCD. Another interesting finding of our work was the association between ADHD-HI and subclinical OCD, and this finding is comparable with that of Sheppard et al. (2010), who found that ADHD symptoms are quite prominent among OCD affected individuals. In this regard, Grisham et al. (2011) suggested that higher levels of hyperactive problems in middle childhood were associated with increased risk of some OC symptoms. Therefore we have to be careful when hyperactive and impulsive symptoms are presented together with the less severe form of the disorder because, as Geller (2006) reported, both disorders contribute to morbid dysfunction and require independent treatment.
In conclusion, we believe that data provided by our study contributes to the understanding of paediatric OCD because we have studied a non-clinical sample whose age period has been described in the literature as the period when OCD first emerges. Another strength of our study was that we used OC symptoms and also OCD diagnoses. We aimed to use the best informant for each type of psychopathological manifestation (Comer & Kendall, 2004; Cosi, Canals, Hernández-Martínez, & Vigil-Colet, 2010) and so we used the CSI-4 to obtain information about behavioural symptoms from the parents and we obtained information about emotional symptoms from the children. However, our study does have some limitations that are worth mentioning. First, our follow-up was only one year and we believe that a longer follow-up study could be useful in this area, because as stated by Eisen et al. (2010), little is known about the long-term course of OCD. Another limitation could be the sample size, because the number of subjects with diagnoses was limited. Furthermore, although we speak of predictor factors of OCD, we do not know if the children diagnosed of OCD in the 2nd phase had had any OCD diagnosis the previous year (1st phase).
In summary, the results showed in the present study suggest that behavioural symptoms and obsessive concern indicate the development of subclinical OCD. Also, the early detection of anxiety symptoms in children is very important because it means that the appropriate treatment can be undertaken, to prevent or improve the course of anxiety disorders such as OCD.
Funding
This research was supported by a grant from the Fondo de Investigaciones Sanitarias (PI07/0839), Instituto de Salud Carlos III of the Spanish Ministry of Health and Consumption and by a doctoral grant from the Department of Universities, Research and the Information Society of the Generalitat de Catalunya (Catalan Government) and the European Social Fund.
*Corresponding author at:
CRAMC (Centre de Recerca en Avaluació i Mesura de la Conducta) - Departament de Psicologia, Universitat Rovira i Virgili,
Carretera de Valls, s/n, 43007 Tarragona, Spain
E-mail address:josefa.canals@urv.cat (J. Canals Sans).
Received June 7, 2012;
accepted October 25, 2012
References
Angulo, R., Jané, M. C., Bonillo, A., Viñas, F., Corcoll-Champredonde, A., González, G., Marina, R., Dos Santos, N. C., & Carbonés, J. (2010). Evaluación de la sintomatología negativista desafiante en niños de seis a ocho años: concordancia entre padres y maestros. Psicothema, 22, 455-459.
Ballesteros, A. T., & Ulloa, R. E. (2011). Estudio comparativo de las características clínicas, demográficas y el funcionamiento familiar en niños y adolescentes con trastorno obsesivocompulsivo leve a moderado vs. grave. Salud Mental, 34, 121-128.
Berg, C. Z., Whitaker, A., Davies, M., Flament, M. F., & Rapoport, J. L. (1988). The survey form of the Leyton Obsessional Inventory-Child Version: Norms from an epidemiological study. Journal of the American Academy of Child & Adolescent Psychiatry, 27, 759-763.
Birmaher, B., Khetarpal, S., Brent, D., Cully, M., Balach, L., Kaufman, J., & Neer, S.M. (1997). The Screen for Child Anxiety Related Emotional Disorders (SCARED): Scale construction and psychometric characteristics. Journal of the American Academy of Child & Adolescent Psychiatry, 39, 545-553.
Brynska, A., & Wolanczyk, T. (2005) Epidemiology and phenomenology of obsessive-compulsive disorder in non-referred young adolescents: A Polish perspective. European Child & Adolescent Psychiatry, 14, 319-327.
Canals, J., Hernández-Martínez, C., Cosi, S., Lázaro, L., & Toro, J. (2012). The Leyton Obsessional Inventory-Child Version and reliability in Spanish non-clinical population. International Journal of Clinical and Health Psychology, 12, 81-96.
Canals, J., Hernández-Martínez, C., Cosi, S., & Voltas, N. (2012). The epidemiology of obsessive-compulsive disorder in Spanish school children. Journal of Anxiety Disorders, 26, 746-752.
Cath, D. C., Van Grootheest, D. S., Willemsen, G., Van Oppen, P., & Boomsma, D. I. (2008). Environmental factors in obsessive-compulsive behavior: Evidence from discordant and concordant monozygotic twins. Behavior Genetics, 38, 108-120.
Claes, L., Nederkoorn, C., Vandereycken, W., Guerrieri, R., & Vertommen, H. (2006). Impulsiveness and lack of inhibitory control in eating disorders. Eating Behaviors, 7, 196-203.
Comer, J. S., & Kendall, P.C. (2004). A symptom-level examination of parent-child agreement in the diagnosis of anxious youths. Journal of the American Academy of Child & Adolescent Psychiatry, 43, 878-886.
Cosi, S., Canals, J., Hernández-Martínez, C., & Vigil-Colet, A. (2010). Parent-child agreement in SCARED and its relationship to anxiety symptoms. Journal of Anxiety Disorders, 24, 129-133.
De Mathis, M. A., Diniz, J. B., Hounie, A. G., Shavitt, R. G., Fossaluza, V., Ferrao, Y., Leckman, J. F., De Bragança Pereira, C., Do Rosario, M. C., & Miguel, E. C. (2012). Trajectory in obsessive-compulsive disorder comorbidities. European Neuropsychopharmacology. Available from:http://dx.doi.Org/10.1016/j.euroneuro.2012.08.006
Degonda, M., Wyss, M., & Angst, J. (1993). The Zurich Study. XVIII. Obsessive-compulsive disorders and syndromes in the general population. European Archives of Psychiatry and Clinical Neuroscience, 243, 16-22.
Douglass, H. M., Moffitt, T. E., Dar, R., McGee, R., & Silva, P. (1995). Obsessive-compulsive disorder in a birth cohort of 18-year-olds: Prevalence and predictors. Journal of the American Academy of Child & Adolescent Psychiatry, 34, 1424-1431.
Eisen, J. L., Mancebo, M. A., Pinto, A., Coles, M. E., Pagano, M. E., Stout, R., & Rasmussen, S. A. (2006). Impact of obsessive-compulsive disorder on quality of life. Comprehensive Psychiatry, 47, 270-275.
Eisen, J. L., Pinto, A., Mancebo, M. C., Dyck, I. R., Orlando, M. E., & Rasmussen, S. A. (2010). A 2-year prospective follow-up study of the course of obsessive-compulsive disorder. Journal of Clinical Psychiatry, 71, 1033-1039.
Figueras, A., Amador-Campos, J. A., Gómez-Benito, J., & Del Barrio, V. (2010) Psychometric properties of the Children's Depression Inventory in community and clinical simple. The Spanish Journal of Psychology, 13, 990-999.
Gadow, K. D., & Sprafkin, J. (1998). Child Symptom Inventory - 4 screening manual. Stony Brook, NY: Checkmate Plus.
Geller, D. A. (2006). Obsessive-compulsive and spectrum disorders in children and adolescents. The Psychiatric Clinics of North America, 29, 353-370.
Grabe, H. J., Meyer, C., Hapke, U., Rumpf, H. J., Freyberger, H., Dilling, H., & John, U. (2000). Prevalence, quality of life and psychosocial function in obsessive-compulsive disorder and subclinical obsessive-compulsive disorder in northern Germany. European Archives of Psychiatry and Clinical Neuroscience, 250, 262-268.
Grisham, J. R., Fullana, M. A., Mataix-Cols, D., Moffitt, T. E., Caspi, A., & Poulton, R. (2011). Risk factors prospectively associated with adult obsessive-compulsive symptom dimensions and obsessive-compulsive disorder. Psychological Medicine, 41, 2495-2506.
Heyman, I., Fombonne, F., Simmons, H., Ford, T., Meltzer, H., & Goodman, R. (2001). Prevalence of obsessive-compulsive disorder in the British nationwide survey of child mental health. The British Journal of Psychiatry, 179, 324-329.
Heyman, I., Mataix-Cols, D., & Fineberg, N. A. (2006). Obsessive-compulsive disorder. British Medical Journal, 333, 424-429.
Hillemacher, T., Kraus, T., Rauh, J., Weiss, J., Schanze, A., Frieling, H., Wilhelm, J., Heberlein, A., Gröschl, M., Sperling, W., Kornhuber, J., & Bleich, S. (2007). Role of appetite-regulating peptides in alcohol craving: An analysis in respect to subtypes and different consumption patterns in alcoholism. Alcoholism: Clinical & Experimental Research, 31, 950-954.
Himle, J. A., Muroff, J. R., Taylor, R. J., Baser, R. E., Abelson, J. M., Hanna, G. L., Abelson, J. L., & Jackson, J. S. (2008). Obsessive-compulsive disorder among African Americans and Blacks of Caribbean descent: Results from the National Survey of American Life. Depression and Anxiety, 25, 993-1005.
Hollingshead, A. B. (2011). Four Factor Index of Social Status. Yale Journal of Sociology, 8, 21-52.
Kim, E. H., Ebesutani, C., Wall, D., & Olatunji, B. O. (2012). Depression mediates the relationship between obsessive-compulsive symptoms and eating disorder symptoms in an inpatient sample. Journal of Obsessive-Compulsive and Related Disorders, 1, 62-68.
Kossowsky, J., Wilhelm, F. H., Roth, W. T., & Schneider, S. (2012). Separation anxiety disorder in children: Disorder-specific responses to experimental separation from the mother. Journal of Child Psychology and Psychiatry, 53, 178-187.
Kovacs, M. (1992). Children's Depression Inventory (CDI). North Tonawanda, NY: Multi-HeBaialth Systems INC.
Lewinsohn, P. M., Hops, H., Roberts, R. E., Seeley, J. R., & Andrews, J. A. (1993). Adolescent psychopathology: I. Prevalence and incidence of depression and other DSM-III-R disorders in high school students. Journal of Abnormal Psychology, 102, 133-144.
Lochner, C., Mogotsi, M., Du Toit, P. L., Kaminer, D., Niehaus, D. J., & Stein, D. J. (2003). Quality of life in anxiety disorders: A comparison of obsessive-compulsive disorder, social anxiety disorder, and panic disorder. Psychopathology, 36, 255-262.
Marcks, B. A., Weisberg, R. B., Dyck, I., & Keller, M. B. (2011). Longitudinal course of obsessive-compulsive disorder in patients with anxiety disorders: A 15-year prospective follow-up study. Comprehensive Psychiatry, 52, 670-677.
Mathews, C. A., Badner, J. A., Andresen, J. M., Sheppard, B., Himle, J. A., Grant, J. E., Williams, K. A., Chavira, D. A., Azzam, A., Schwartz, M., Reus, V. I., Kim, S. W., Cook, E. H., & Hanna, G. L. (2012). Genome-wide linkage analysis of obsessive-compulsive disorder implicates chromosome 1p36. Biological Psychiatry, 72, 629-636.
Micali, N., Heyman, I., Pérez, M., Hilton, K., Nakatani, E., Turner, C., & Mataix-Cols, D. (2010). Long-term outcomes of obsessive-compulsive disorder: Follow-up of 142 children and adolescents. The British Journal of Psychyatry, 197, 128-134.
Mroczkowski, M. M., Goes, F. S., Riddle, M. A., Grados, M. A., Bienvenu, O. J., Greenberg, B. D., Fyer, A. J., McCracken, J. T., Rauch, S. L., Murphy, D. L., Knowles, J. A., Piacentini, J., Cullen, B., Rasmussen, S. A., Geller, D. A., Pauls, D. L., Liang, K. Y, Nestadt, G., & Samuels, J. F. (2011). Separation anxiety disorder in OCD. Depression and Anxiety, 28, 256-262.
Olatunji, B. O., Davis, M. L., Powers, M. B., & Smits, J. A. (2013). Cognitive-behavioral therapy for obsessive-compulsive disorder: A meta-analysis of treatment outcome and moderators. Journal of Psychiatric Research, 47, 33-41.
Peterson, B. S., Pine, D. S., Cohen, P., & Brook, J. S. (2001). Prospective, longitudinal study of tic, obsessive-compulsive, and attention-deficit/hyperactivity disorders in an epidemiological sample. Journal of the American Academy of Child & Adolescent Psychiatry, 40, 685-695.
Rosa-Alcázar, A. I., Sánchez-Meca, J., Gómez-Conesa, A., & Marín-Martínez, F. (2008). Psychological treatment of obsessive-compulsive disorder: A meta-analysis. Clinical Psychology Review, 28, 1310-1325.
Sheehan, D., Lecrubier, Y., Sheehan, K. H., Amorim, P., Janavs, J., Weiller, E., Hergueta, T., Baker, R., & Dunbar, G. C. (1998). The Mini-International Neuropsychiatric Interview (M.I.N.I): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. Journal of Clinical Psychiatry, 59, 22-33.
Sheehan, D. V., Sheehan, K. H., Shytle, R. D., Janavs, J., Bannon, Y., Rogers, J. E., Milo, K. M., Stock, S. L., & Wilkinson, B. (2010). Reliability and validity of the Mini International Neuropsychiatric Interview for Children and Adolescents (MINI-KID). Journal of Clinical Psychiatry, 71, 313-326.
Sheppard, B., Chavira, D., Azzam, A., Grados, M. A., Umaña, P., Garrido, H., & Mathews, C. A. (2010). ADHD prevalence and association with hoarding behaviors in childhood-onset OCD. Depression and Anxiety, 27, 667-674.
Sprafkin, J., Gadow, K. D., Salisbury, H., Schneider, J., & Loney, J. (2002). Further evidence of reliability and validity of the Child Symptom Inventory-4: Parent Checklist in clinically referred boys. Journal of Clinical Child and Adolescent Psychology, 31, 513-524.
Stewart, S. E., Geller, D. A., Jenike, M., Pauls, D., Shaw, D., Mullin, B., & Faraone, S. V. (2004). Long-term outcome of pediatric obsessive-compulsive disorder: A meta-analysis and qualitative review of the literature. Acta Psychiatrica Scandinavica, 110, 4-13.
Storch, E. A., Lewin, A. B., Larson, M. J., Geffken, G. R., Murphy, T. K., & Geller, D. A. (2012). Depression in youth with obsessive-compulsive disorder: Clinical phenomenology and correlates. Psychiatry Research, 196, 83-89.
Storch, E. A., Merlo, L. J., Keeley, M. L., Grabill, K., Milsom, V. A., Geffken, G. R., Ricketts, E., Murphy, T. K., & Goodman, W. K. (2008). Somatic symptoms in children and adolescents with obsessive-compulsive disorder: Associations with clinical characteristics and cognitive-behavioural therapy response. Behavioural and Cognitive Psychotherapy, 36, 283-297.
Swedo, S. E., Leonard, H. L., Garvey, M., Mittleman, B., Allen, A. J., Perlmutter, S., Lougee, L., Dow, S., Zamkoff, J., & Dubbert, B. K. (1998). Pediatric autoimmune neuropsychiatric disorders associated with streptococcal infections: clinical description of the first 50 cases. The American Journal of Psychiatry, 155, 264-271.
Taylor, S. (2011). Etiology of obsessions and compulsions: A meta-analysis and narrative review of twin studies. Clinical Psychology Review, 31, 1361-1372.
Vigil-Colet, A., Canals, J., Cosi, S., Lorenzo-Seva, U., Ferrando, P.J., Hernández-Martínez, C., Jané, M.C., Viñas, F., & Domènech, E. (2009). The factorial structure of the 41-item version of the Screen for Child Anxiety Related Emotional Disorders (SCARED) in a Spanish population of 8 to 12 years-old. International Journal of Clinical and Health Psychology, 9, 313-327.
Walitza, S., Melfsen, S., Jans, T., & Zellmann, H. (2011). Obsessive-compulsive disorder in children and adolescents. Deutsches Ärzteblatt International, 108, 173-179.
Zolog, T., Jané, M. C., Bonillo, A., Canals, J., Hernández-Martínez, C., Romero, K., & Domènech, E. (2011). Somatic complaints and symptoms of anxiety and depression in a school-based sample of preadolescents and early adolescents. Functional impairment and implications for treatment. Journal of Cognitive and Behavioral Psychotherapies, 11, 191-208.