The Short Health Anxiety Inventory (SHAI) is a widely used self-report instrument to evaluate health anxiety. To assess the SHAI's factor structure, psychometric properties, and accuracy in differentiating Spanish non-clinical individuals from patients with severe health anxiety or hypochondriasis.
MethodA total of 342 community participants (61.6% women; Mage=34.60, SD=14.91) and 31 hypochondriacal patients (51.6% women; Mage=32.74, SD=9.69) completed the SHAI and other self-reports assessing symptoms of hypochondriasis, depression, anxiety sensitivity, worry, and obsessive-compulsive.
ResultsThe original two-factor structure was selected as the best structure, based on its parsimony and empirical support (Factor 1: Illness likelihood; Factor 2: Negative consequences of illness). Moreover, the Spanish version of the SHAI demonstrated good construct and concurrent and discriminant validity, and internal consistency. A cutoff of 40.5 (total score) accurately distinguished non-clinical individuals from patients with severe health anxiety or hypochondriasis.
ConclusionsThe SHAI is an adequate screening instrument to measure health anxiety in Spanish-speaking community adults.
El Inventario Breve de Ansiedad por la Salud (SHAI, por sus iniciales en inglés) es un autoinforme ampliamente empleado para evaluar ansiedad por la salud. El objetivo es evaluar la estructura factorial del SHAI, sus propiedades psicométricas, y exactitud diferenciando entre población española no clínica y pacientes con hipocondría.
MétodoUn total de 342 participantes extraídos de la población general (66% mujeres, Medad=35, DT=14,91) y 31 pacientes con hipocondría (51,6% mujeres; Medad=32,74, DT=9,69 completaron el SHAI y otros autoinformes de síntomas hipocondriacos, depresión, sensibilidad a la ansiedad, preocupaciones y obsesivo-compulsivos.
ResultadosLa estructura de dos factores propuesta originalmente fue seleccionada como la mejor estructura debido a su parsimonia y soporte empírico (Factor 1: Probabilidad de enfermar; Factor 2: Consecuencias negativas enfermedad). La versión española del SHAI muestra una buena consistencia interna, y validez de constructo, concurrente y discriminante. El punto de corte de 40,5 (puntuación total) permite distinguir entre los individuos no clínicos y los pacientes con elevada ansiedad por la salud o hipocondría.
ConclusionesEl SHAI es un instrumento adecuado para la detección de ansiedad por la salud en población adulta hispano hablante.
Health anxiety is conceptualized as a continuum that ranges from mild non- clinical health concerns to severe or hypochondriacal concerns (Bailer et al., 2016; Bobevski, Clarke, & Meadows, 2016; Warwick & Salkovskis, 1990). Individuals with health anxiety will vary in their resistance to medical reassurance, and in their distress level, functional impairment, and use of health care services. In addition, these individuals can experience intrusive thoughts related to illness contents (Arnáez, García-Soriano, & Belloch, 2017; Pascual-Vera & Belloch, 2018). The cognitive-behavioral approach proposes that individuals with health anxiety tend to catastrophically misinterpret ambiguous illness-related information, medical information, and bodily signs or symptoms. Moreover, this misinterpretation could lead individuals with severe health anxiety to believe that they are suffering from a serious illness (Warwick & Salkovskis, 1990). In order to measure the aforementioned continuum from non-clinical to clinical health anxiety, Salkovskis, Rimes, Warwick, and Clark (2002) developed a self-rated questionnaire, the Health Anxiety Inventory (HAI), containing 64 items. Each item consists of a group of four statements, and respondents are asked to indicate the single statement in each group that best applies to them (e.g., from ‘I do not worry about my health’ to ‘I spend most of my time worrying about my health’). The HAI demonstrated excellent internal consistency and satisfactory test-retest reliability, was sensitive to treatment effects, and differentiated between patients with hypochondriasis, patients with anxiety disorders, and community participants (Salkovskis et al., 2002). The authors also developed a shortened version with 18 items, the Short Health Anxiety Inventory (SHAI), as a screening instrument to assess health anxiety independently of the person's physical health status, thus providing a brief and quick instrument to differentiate between disabling and normal health anxiety in both medical and non-medical samples. The 18 items were distributed in two factors: the first included 14 items and assessed the likelihood of becoming ill, whereas the second factor (4 items) evaluated the negative consequences or ‘awfulness’ of illness (Salkovskis et al., 2002).
Since its development and publication, the SHAI has been widely used to assess health anxiety, and several studies in different countries have supported its reliability and validity in both clinical and non-clinical samples (see Alberts, Hadjistavropoulos, Jones, & Sharpe, 2013 for a review). For example, the SHAI internal consistency ranged from α=.82 (Morales, Reis, Espada, & Orgilés, 2016) to α=.96 (Abramowitz, Olatunji, & Deacon, 2007), and test-retest reliability ranged from r=.56 (Zhang, Liu, Li, Mao, & Yuan, 2015) to r=.90 (Salkovskis et al., 2002). Moreover, the questionnaire showed high associations with hypochondriacal symptoms, but the associations were only moderate with worry, anxiety sensitivity, obsessive-compulsive, or depressive symptoms (Abramowitz, Deacon, & Valentiner, 2007; Abramowitz, Olatunji, & Deacon, 2007; Wheaton, Berman, Flanking, & Abramowitz, 2010). However, the original two-factor structure (Salkovskis et al., 2002) has been questioned. Abramowitz, Deacon, and Valentiner (2007) obtained a three-factor structure -Illness likelihood, Illness severity, and Body vigilance- in a sample of medically healthy university students. The first and third factors or subscales differed from those proposed by Salkovskis et al. (2002), whereas the Illness severity subscale overlapped with the Negative consequences of illness subscale originally described by Salkovskis et al. (2002). In addition, Abramowitz, Olatunji et al. (2007) compared the original two-factor structure to the three-factor structure (Abramowitz, Deacon et al., 2007) in two clinical samples of patients with hypochondriasis and patients with anxiety disorders. The results showed a similar fit for both models. Thus, following the parsimony principle, they selected the original two-factor model. Later, Wheaton et al. (2010) proposed a two-factor model similar to Salkovskis et al. (2002), but removing item 13 because it loaded in both factors. The subscales were labelled Illness likelihood and Illness severity. Finally, Alberts, Sharpe, Kehler, and Hadjistavropoulos (2011) analyzed the factor structure of the original scale of Likelihood of becoming ill (comprising items 1 to 14) in two different samples: a not seriously ill sample and a sample with multiple sclerosis. They derived a model with two factors labelled Thought intrusion and Fear of illness. Item 14 was not included because it did not load in any factor. The authors did not include the Negative consequences of illness factor proposed by Salkovskis et al. (2002) in their analyses because they thought it did not directly assess health anxiety and was not suitable for medical samples with a diagnosed illness. Although the discrepancies about the SHAI's structure are evident, the original two-factor model has received further support from research (i.e., Morales, Espada, Carballo, Piqueras, & Órgiles, 2015; te Poel, Hartmann, Baumgartner, & Tanis, (2017). The SHAI has been translated and validated in a wide range of countries and languages, such as Chinese (Zhang et al., 2015), Dutch (te Poel et al., 2017), Polish (Kocjan, 2016), Portuguese (Morales et al., 2016), or Spanish (Morales et al., 2015). This latter study used a sample of adolescents (Mage=15.72 years, SD=0.72). Nonetheless, no studies have analyzed the psychometric properties and structure of the SHAI in Spanish non-clinical adults (>18 years) and compared their scores to those of patients with a clinical diagnosis of hypochondriasis in order to establish a cutoff score.
With all this in mind, the current study has three objectives. The first objective is to examine the factor structure (factor validity) that best fits the SHAI Spanish version in an adult community sample, compared to the different proposals reported in the literature. The second objective is to investigate the psychometric properties (internal consistency and associations among the subscales) and convergent and divergent validity of the SHAI Spanish version and its subscales. The third objective is to compare the scores of non-clinical participants and patients with hypochondriasis on the SHAI and determine its diagnostic utility by examining the accuracy of different cutoff scores in differentiating patients with a primary diagnosis of hypochondriasis from non-clinical individuals.
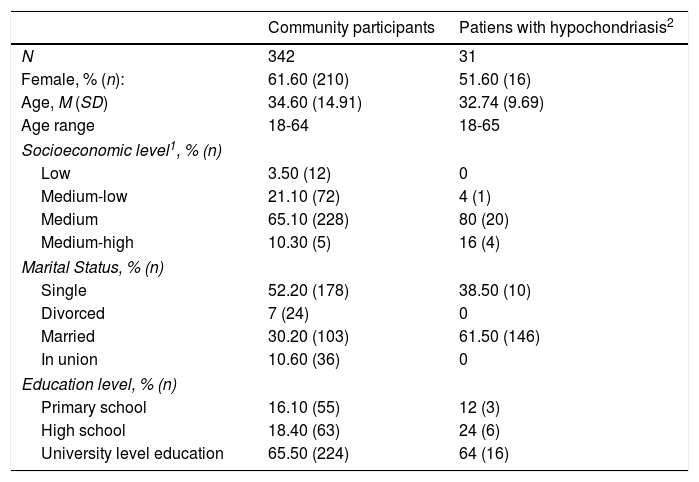
MethodParticipantsTwo groups of Spanish participants were included in the study. The first group consisted of 342 community participants, and the second group consisted of 31 individuals who met the diagnostic criteria for hypochondriasis according to the Diagnostic Statistical Manual of Mental Disorders Fourth Edition (DSM-IV) text revision and the International Classification of Diseases, 11th (World Health Organization WHO, 2018). Descriptive data for both groups are included in Table 1.
Descriptive statistics of the samples.
| Community participants | Patiens with hypochondriasis2 | |
|---|---|---|
| N | 342 | 31 |
| Female, % (n): | 61.60 (210) | 51.60 (16) |
| Age, M (SD) | 34.60 (14.91) | 32.74 (9.69) |
| Age range | 18-64 | 18-65 |
| Socioeconomic level1, % (n) | ||
| Low | 3.50 (12) | 0 |
| Medium-low | 21.10 (72) | 4 (1) |
| Medium | 65.10 (228) | 80 (20) |
| Medium-high | 10.30 (5) | 16 (4) |
| Marital Status, % (n) | ||
| Single | 52.20 (178) | 38.50 (10) |
| Divorced | 7 (24) | 0 |
| Married | 30.20 (103) | 61.50 (146) |
| In union | 10.60 (36) | 0 |
| Education level, % (n) | ||
| Primary school | 16.10 (55) | 12 (3) |
| High school | 18.40 (63) | 24 (6) |
| University level education | 65.50 (224) | 64 (16) |
Note.1 Socioeconomic level described following the parameters of the Spanish National Institute of Statistics. 2 In the clinical sample, socioeconomic and educational level was calculated based on 25 participants, and marital status based on 26 participants.
Patients were diagnosed by experienced clinicians using the Structured Diagnostic Interview for Hypochondriasis (SDIH) and comorbidity was assessed using the International Neuropsychiatric Interview (MINI). At the time of the study, none of the patients met the criteria for a mental disorder other than hypochondriasis, and one of them had a lifetime history of Generalized Anxiety Disorder. Disorder severity was assessed with the Hypochondriasis-YBOCS-M, with scores ranging from 15 to 58 (M=46.12, SD=9.41). The inclusion criteria were as follows: a primary diagnosis of hypochondriasis (DSM-IV-TR criteria), age range between 18 and 65 years, a duration of hypochondriasis of at least one year, absence of any organic mental disorder, mental retardation, psychotic disorder, Cluster A personality disorder, or current history of substance abuse disorders, and having an adequate level of reading ability.
InstrumentsSocio-demographic data sheet. The data required were the following: age, gender, years of education or maximum level of studies reached, marital status, and socio-economic level.
Short Health Anxiety Inventory (SHAI; Salkovskis et al., 2002. Spanish translation: Caballo, 2006). As described above, the SHAI is a self-report instrument that evaluates health anxiety in medical and non-medical contexts. Each item consists of a group of four statements that are scored from 1 to 4. Because this is the target measure in the current study, its psychometric properties in the two samples will be described in the results section.
Whiteley Index (WI; Pilowsky, 1967. Spanish version: Avia, 2017). A 14-item self-report questionnaire measures hypochondriasis using a dichotomous yes/no format. It has demonstrated good validity and reliability. The internal consistency in the non-clinical sample of the current study was α=.70.
Beck Depression Inventory (BDI-II; Beck, Steer, & Brown, 1996. Spanish version: Sanz, Perdigón, & Vázquez, 2003). It is a 21-item self-report measure of depressive symptoms ranging from 0 (symptom not present) to 3 (symptom very intense). It has demonstrated stability over time and across countries (Schürmann & Margraf, 2018). The BDI-II showed adequate internal consistency in this study (α=.89).
Anxiety Sensitivity Index-3 (ASI-3; Taylor et al., 2007. Spanish version: Sandín, Valiente, Chorot, & Santed, 2007). It is an 18-item measure that assesses the tendency to fear anxiety symptoms based on the belief that they could have harmful consequences. Items are rated from 0=very little to 4=very much. The ASI-3 has three subscales related to fears of social concerns, fears of physical symptoms, and fears of cognitive decontrol. In the current study, internal consistency for the total score in the non-clinical sample was good (α=.80).
Penn State Worry Questionnaire (PSWQ; Meyer, Miller, Metzger, & Borkovek, 1990. Spanish version: Sandín, Chorot, Valiente, & Lostao, 2009). It is a 16-item self-report questionnaire rated on a 5-point Likert scale and designed to evaluate the tendency to worry excessively without regard to the specific content. Reliability in the present study was α=.87 (non-clinical sample).
Obsessive-Compulsive Inventory-Revised (OCI-R; Foa et al., 2002. Spanish version: Belloch et al., 2013). It is an 18-item self-report instrument to measure OCD symptoms. Respondents rate the distress caused by OCD symptoms in the past month from 0 (not at all) to 4 (extremely). The OCI-R consists of six subscales, and its total score, used in the current study, provides a general index of OCD severity. In the current study, an α=.80 was obtained for the total score in the non-clinical sample.
ProcedureCommunity participants were recruited by undergraduate psychology students, under the supervision of three of the authors. In order to ensure the quality of the data, students were chosen due to their interest in research. Prior to their participation in the research, all the students voluntarily attended a seminar where the aim of the study and the administration of the questionnaires to future participants were explained, emphasizing aspects such as the relevance of privacy, sincerity of participants’ responses, etc. Students received academic credits for their collaboration. Each student administered the questionnaires individually to at least three friends or relatives. Inclusion criteria were age ranging from 18 to 65 years, good reading level, and not having a recent history of mental disorders or disabling medical disease in the preceding year. All the participants were previously informed of the purpose of the study, and they gave their formal written consent to participate. Then, they were given a booklet containing the questionnaires described above, which were presented in a randomized order to avoid response biases.
Clinical participants were recruited from outpatient mental health clinics pertaining to the University and to the Spanish National Health System. All potential participants were individually screened with a full history and examination by one of the authors. As mentioned above, the intake assessment included the SDIH and the MINI diagnostic interviews, a full history, and the Hypochondriasis-YBOCS-M. Then, patients were informed about the purpose and assessment procedure of the study and asked for their explicit consent to participate. After the patient had given his or her explicit consent, individualized, face-to-face administration of the SHAI was carried out. The study was approved by the ethics committees of the University and the outpatient mental health clinic.
Data analysesThis study was carried out using an instrumental, transversal design (Montero & León, 2007). To examine the factorial structure of the SHAI we conducted an exploratory factor analysis (EFA) and a confirmatory factor analyses (CFA) using the SPSS statistical package (version 22.0) and the EQS 6.1, respectively. First, we explored the factorial structure of the SHAI using EFA in community participants (n=219), and second, through CFA, we studied whether the factorial structure obtained (including a single-factor model) and the structures proposed in the literature fit our data. Specifically, the following six CFA models were examined: Model 1 was a single-factor model representing the possibility of including all the health concern contents in a single homogenous dimension of health anxiety. This model is used as a baseline (or default) model for the data. Model 2 tested the factorial structured obtained in the EFA. Model 3 included the original two-factor solution proposed by Salkovskis et al. (2002), that is, the likelihood of becoming ill (items 1 to 14) and negative consequences of illness (items 15 to 18). Model 4 tested the almost identical two-factor solution proposed by Wheaton et al. (2010) (subscale 1: Illness likelihood including items 1 to 12 and 14 [item 13 was removed], and subscale 2: Illness severity, items 15 to 18). Model 5 consisted of the three-factor model proposed by Abramowitz, Deacon et al. (2007): Illness likelihood (items 1, 4-9, 11, 12, and 14), Illness severity (items 15 to 18), and Body vigilance (items 2, 3, and 10). Finally, Model 6 included the two-factor solution proposed by Alberts, Sharpe, Kehler, & Hadjistavropoulos (2011): Thought intrusion (items 1-4, 6-7, 10, and 13) and Fear of illness (items 5, 8, 9, 11, and 12). To avoid distribution problems in the data set, the Maximum Likelihood (ML) method with robust correction was applied. To assess the fit of the factor structure, we used the chi-square (χ2), Akaike's information criterion (AIC), as well as the Comparative Fit Index (CFI), Goodness of Fit Index (GFI), Root Mean Square Error of Approximation (RMSEA), with a 90% confidence interval. The following criteria indicate a good fit of the models to the data: CFI and GFI ≥ .90, RMSEA ≤ .06, and a non-significant chi-square (Hu & Bentler, 1999). Moreover, CFI values ≥.90 and RMSEA values ≤.08 are considered acceptable, and CFI ≥ 95 and RMSEA ≤.06 are considered optimal (Marsh, Hau, & Wen, 2004). Smaller chi-square and AIC values indicate better fit.
Pearson's correlation coefficients were used to examine the relationships between the SHAI and other measures. Differences between groups (clinical vs. non-clinical) were examined by using t tests. Cohen d values were calculated to estimate the effect size of comparisons. Receiver operating characteristic (ROC) analysis was conducted to examine the accuracy of the SHAI-total score in differentiating patients with hypochondriasis from non-patients. The ROC analysis uses the association between sensitivity and specificity to estimate the area under the curve (AUC), with a 95% CI, in order to indicate how well a measure distinguishes between positive (i.e., a diagnosis of hypochondriasis) and negative (i.e., absence of psychopathology) cases. To determine the appropriate cutoff-point for severe health anxiety, the Youden index (sensitivity+specificity−1) was calculated, and the corresponding cutoff value for the highest Youden index was considered as the optimal cutoff value.
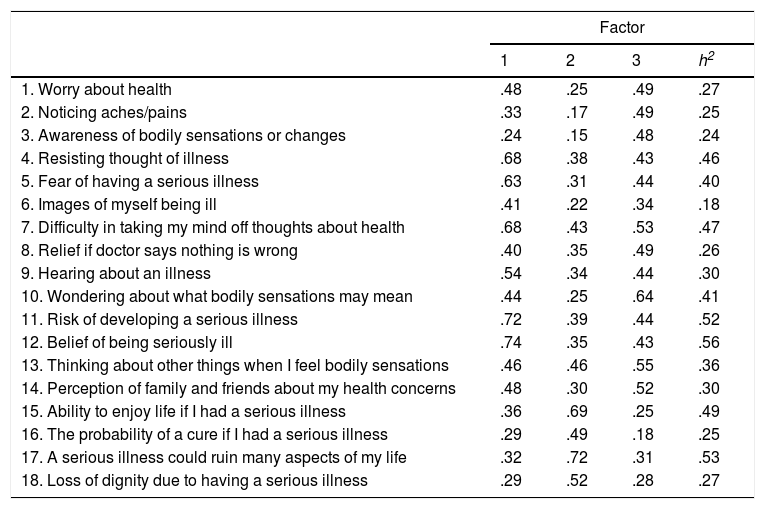
ResultsFactor structure of the SHAI: Exploratory factor analysisFirst, the suitability of the data for the factor analysis was tested. The Kaiser–Meyer–Olkin measure of sampling adequacy was .89, above the recommended cut-off point of .60, and Bartlett's Test of Sphericity was significant (X2 [153]=1673.35, p<.001), indicating that factor analysis was appropriate. Factor analysis was carried out using principal axis factoring with promax (oblique) rotation because it was anticipated that the factors would be correlated. The eigenvalues greater than one suggested three factors that explained 36.75% of the variance after rotation. The first factor accounted for 27.58% of the total variance, the second accounted for 5.76%, and the third accounted for 3.41%. Significant loadings were set at .40 or higher. Table 2 shows the factor loadings and communalities for the three-factor solution.
Exploratory factor analysis of the SHAI: Factor loadings and communalities (h2).
| Factor | ||||
|---|---|---|---|---|
| 1 | 2 | 3 | h2 | |
| 1. Worry about health | .48 | .25 | .49 | .27 |
| 2. Noticing aches/pains | .33 | .17 | .49 | .25 |
| 3. Awareness of bodily sensations or changes | .24 | .15 | .48 | .24 |
| 4. Resisting thought of illness | .68 | .38 | .43 | .46 |
| 5. Fear of having a serious illness | .63 | .31 | .44 | .40 |
| 6. Images of myself being ill | .41 | .22 | .34 | .18 |
| 7. Difficulty in taking my mind off thoughts about health | .68 | .43 | .53 | .47 |
| 8. Relief if doctor says nothing is wrong | .40 | .35 | .49 | .26 |
| 9. Hearing about an illness | .54 | .34 | .44 | .30 |
| 10. Wondering about what bodily sensations may mean | .44 | .25 | .64 | .41 |
| 11. Risk of developing a serious illness | .72 | .39 | .44 | .52 |
| 12. Belief of being seriously ill | .74 | .35 | .43 | .56 |
| 13. Thinking about other things when I feel bodily sensations | .46 | .46 | .55 | .36 |
| 14. Perception of family and friends about my health concerns | .48 | .30 | .52 | .30 |
| 15. Ability to enjoy life if I had a serious illness | .36 | .69 | .25 | .49 |
| 16. The probability of a cure if I had a serious illness | .29 | .49 | .18 | .25 |
| 17. A serious illness could ruin many aspects of my life | .32 | .72 | .31 | .53 |
| 18. Loss of dignity due to having a serious illness | .29 | .52 | .28 | .27 |
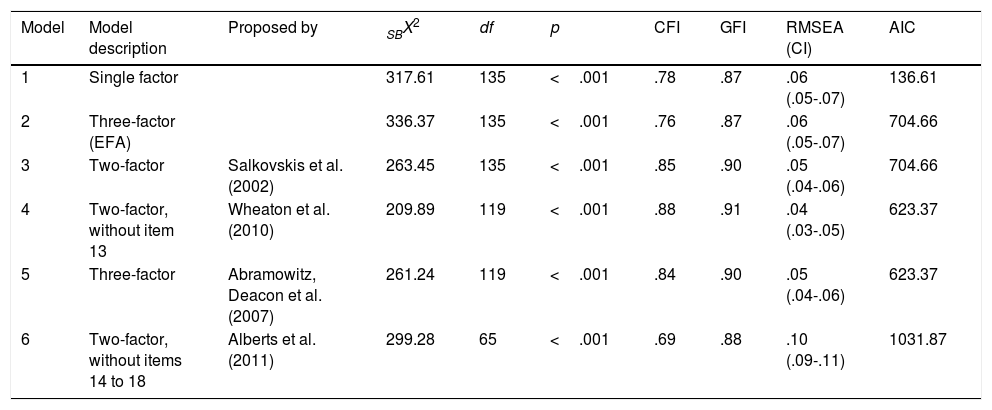
Following our previous exploratory analysis of the questionnaire, as well as the findings reported in the existing literature, we tested six CFA at the item level, using the data obtained from the community participants. Table 3 shows the fit indexes for the six tested models. Following Hu and Bentler's (1999) criteria, the models that most closely matched the criteria were models 3 (Salkovskis et al., 2002), 4 (Wheaton et al., 2010), and 5 (Abramowitz, Deacon et al., 2007) because the index rates of these models were slightly closer to the established criteria, CFI and GFI ≥.90 and RMSEA ≤06, and the chi-square and AIC values were smaller. Moreover, as proposed by Marsh et al. (2004), GFI values were acceptable, and RMSEA values were optimal. The fit indexes of the three models were fairly equivalent, but slightly higher for Model 4. However, because Model 3 and 4 are fairly similar (with model 4 deleting one item from the original scale), but Model 3 parallels the original factor solution of the Spanish adolescent version (Morales et al., 2015) and most validations of the SHAI (e.g., Kocjan, 2016; Morales et al., 2015; te Poel et al., 2017; Zhang et al., 2015), this structure was selected. Factor loadings for each item in its corresponding factor are shown in Table 4.
Goodness-of-fit indices of the SHAI factor models analyzed (n=342; community participants).
| Model | Model description | Proposed by | SBX2 | df | p | CFI | GFI | RMSEA (CI) | AIC |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Single factor | 317.61 | 135 | <.001 | .78 | .87 | .06 (.05-.07) | 136.61 | |
| 2 | Three-factor (EFA) | 336.37 | 135 | <.001 | .76 | .87 | .06 (.05-.07) | 704.66 | |
| 3 | Two-factor | Salkovskis et al. (2002) | 263.45 | 135 | <.001 | .85 | .90 | .05 (.04-.06) | 704.66 |
| 4 | Two-factor, without item 13 | Wheaton et al. (2010) | 209.89 | 119 | <.001 | .88 | .91 | .04 (.03-.05) | 623.37 |
| 5 | Three-factor | Abramowitz, Deacon et al. (2007) | 261.24 | 119 | <.001 | .84 | .90 | .05 (.04-.06) | 623.37 |
| 6 | Two-factor, without items 14 to 18 | Alberts et al. (2011) | 299.28 | 65 | <.001 | .69 | .88 | .10 (.09-.11) | 1031.87 |
Notes. SBX2=Satorra-Bentler Scaled Chi-Square; CFI=Comparative Fit Index; GFI=Goodness of Fit Index; RMSEA=Root Mean-Square Error of Approximation.
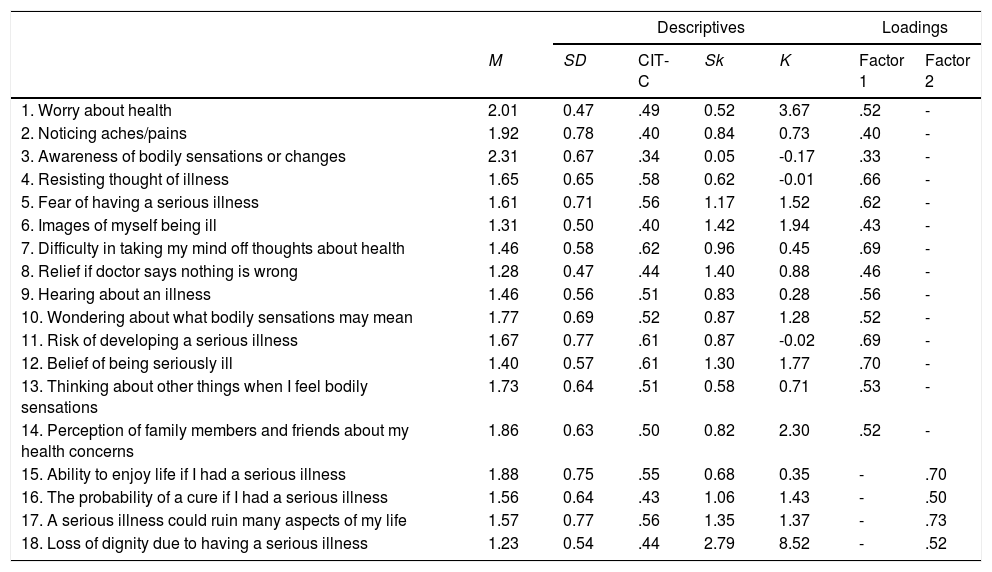
Item description and factor loadings of the Sort Health Anxiety Inventory (n=342; community participants).
| Descriptives | Loadings | ||||||
|---|---|---|---|---|---|---|---|
| M | SD | CIT-C | Sk | K | Factor 1 | Factor 2 | |
| 1. Worry about health | 2.01 | 0.47 | .49 | 0.52 | 3.67 | .52 | - |
| 2. Noticing aches/pains | 1.92 | 0.78 | .40 | 0.84 | 0.73 | .40 | - |
| 3. Awareness of bodily sensations or changes | 2.31 | 0.67 | .34 | 0.05 | -0.17 | .33 | - |
| 4. Resisting thought of illness | 1.65 | 0.65 | .58 | 0.62 | -0.01 | .66 | - |
| 5. Fear of having a serious illness | 1.61 | 0.71 | .56 | 1.17 | 1.52 | .62 | - |
| 6. Images of myself being ill | 1.31 | 0.50 | .40 | 1.42 | 1.94 | .43 | - |
| 7. Difficulty in taking my mind off thoughts about health | 1.46 | 0.58 | .62 | 0.96 | 0.45 | .69 | - |
| 8. Relief if doctor says nothing is wrong | 1.28 | 0.47 | .44 | 1.40 | 0.88 | .46 | - |
| 9. Hearing about an illness | 1.46 | 0.56 | .51 | 0.83 | 0.28 | .56 | - |
| 10. Wondering about what bodily sensations may mean | 1.77 | 0.69 | .52 | 0.87 | 1.28 | .52 | - |
| 11. Risk of developing a serious illness | 1.67 | 0.77 | .61 | 0.87 | -0.02 | .69 | - |
| 12. Belief of being seriously ill | 1.40 | 0.57 | .61 | 1.30 | 1.77 | .70 | - |
| 13. Thinking about other things when I feel bodily sensations | 1.73 | 0.64 | .51 | 0.58 | 0.71 | .53 | - |
| 14. Perception of family members and friends about my health concerns | 1.86 | 0.63 | .50 | 0.82 | 2.30 | .52 | - |
| 15. Ability to enjoy life if I had a serious illness | 1.88 | 0.75 | .55 | 0.68 | 0.35 | - | .70 |
| 16. The probability of a cure if I had a serious illness | 1.56 | 0.64 | .43 | 1.06 | 1.43 | - | .50 |
| 17. A serious illness could ruin many aspects of my life | 1.57 | 0.77 | .56 | 1.35 | 1.37 | - | .73 |
| 18. Loss of dignity due to having a serious illness | 1.23 | 0.54 | .44 | 2.79 | 8.52 | - | .52 |
Note. M=mean; SD=standard deviation; CIT-C: corrected item total correlations; Sk=skewness; K=kurtosis; Factor 1=Illness likelihood; Factor 2=Negative consequences of illness. Only saturations≥ .30 are included.
The descriptive data for the items are presented in Table 4. In general, the items showed low means (Mmean=1.65, range: 1.23-2.31) and low standard deviations (MSD=0.63, range: 0.47-0.77). Moreover, the items showed a trend toward positive skewness (MSk=1.01, range [0.05-2.79]) and kurtosis (MK=1.5, range [-0.17-8.52]).
The SHAI total score and subscales demonstrated adequate internal consistency for the total score (α= .86) and subscales (Illness likelihood: α=.85; Negative consequences of illness: α= .70). The items on the Illness likelihood subscale (1-14) obtained an acceptable corrected item-total correlation (range r=.34 to .62), as did the items on the Negative consequences subscale (15-18) (range r=.44 to .56).
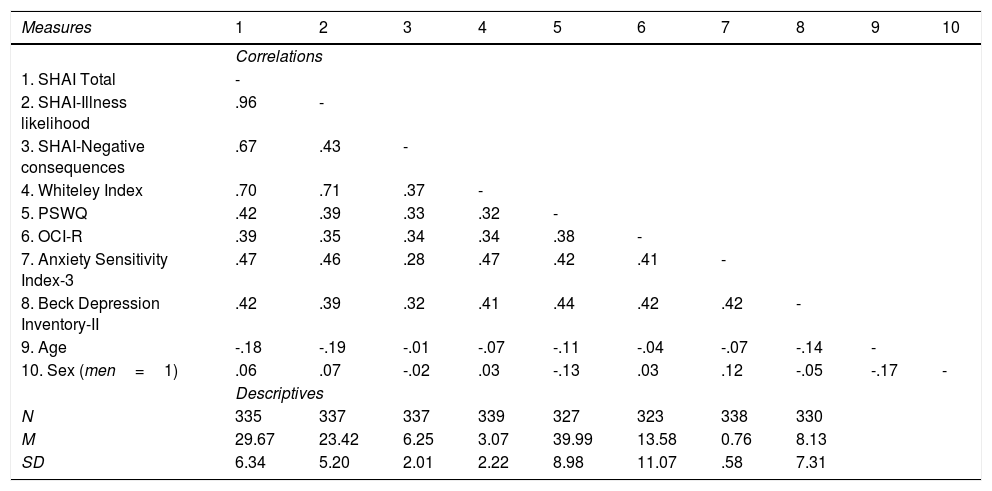
Correlations between the SHAI and the study measuresTable 5 presents the relationships among the SHAI, the other self-report measures, and the demographic data. Regarding the intercorrelations, high and significant correlations were obtained between the SHAI total score and its subscales with the other study measures, but only moderate relationships were found between the two SHAI-subscales, which indicates that they were assessing different but related aspects of health anxiety. The SHAI total score and the Illness likelihood subscale showed significant and high correlations with the Whiteley Index, which assesses hypochondriacal symptoms, and medium associations with the other psychopathological measures. The Negative consequences of illness subscale correlate moderately with the WI, as well as with the other measures, with the exception of the ASI-3, which showed a small association. The sizes of the correlations among the Illness likelihood subscale, hypochondriacal symptoms, and anxiety sensitivity were significantly higher than between the WI and ASI-3 and the Negative consequences of illness subscale (WI: z=6.45, p <.001; ASI-3: z=2.27, p=.01). Age was significantly and negatively correlated with the SHAI total scale and the Illness likelihood subscale, although the size of the coefficient was small. No significant correlations were found between the SHAI scores and gender.
Pearson correlations and descriptive statistics (community participants).
| Measures | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
|---|---|---|---|---|---|---|---|---|---|---|
| Correlations | ||||||||||
| 1. SHAI Total | - | |||||||||
| 2. SHAI-Illness likelihood | .96 | - | ||||||||
| 3. SHAI-Negative consequences | .67 | .43 | - | |||||||
| 4. Whiteley Index | .70 | .71 | .37 | - | ||||||
| 5. PSWQ | .42 | .39 | .33 | .32 | - | |||||
| 6. OCI-R | .39 | .35 | .34 | .34 | .38 | - | ||||
| 7. Anxiety Sensitivity Index-3 | .47 | .46 | .28 | .47 | .42 | .41 | - | |||
| 8. Beck Depression Inventory-II | .42 | .39 | .32 | .41 | .44 | .42 | .42 | - | ||
| 9. Age | -.18 | -.19 | -.01 | -.07 | -.11 | -.04 | -.07 | -.14 | - | |
| 10. Sex (men=1) | .06 | .07 | -.02 | .03 | -.13 | .03 | .12 | -.05 | -.17 | - |
| Descriptives | ||||||||||
| N | 335 | 337 | 337 | 339 | 327 | 323 | 338 | 330 | ||
| M | 29.67 | 23.42 | 6.25 | 3.07 | 39.99 | 13.58 | 0.76 | 8.13 | ||
| SD | 6.34 | 5.20 | 2.01 | 2.22 | 8.98 | 11.07 | .58 | 7.31 | ||
Note. Bold values correspond to statistically significant correlations (p≤ .05). Sex was coded with a dummy variable, where 0=women and 1=men. SHAI=Short Health Anxiety Inventory; PSWQ=Penn State Worry Questionnaire; OCI-R=Obsessive-Compulsive Inventory-Revised.
Community participants and patients with hypochondriasis obtained significantly different scores on the SHAI, with patients showing higher total scores (M=29.67, SD=6.35 vs. M=54.26, SD=5.51; t(366)=20.60, p <.001, Cohen’ d=4.13) and higher scores on the subscales: Likelihood of becoming il (M=23.42, SD=5.20 vs. M=43.45, SD=5.25; t(366)=20.49, p <.001, Cohen’ d=3.82) and Negative consequences of illness (M=6.25, SD=2.03 vs. M=10.81, SD=1.88; t(366)=12.12, p <.001, Cohen’ d=2.33).
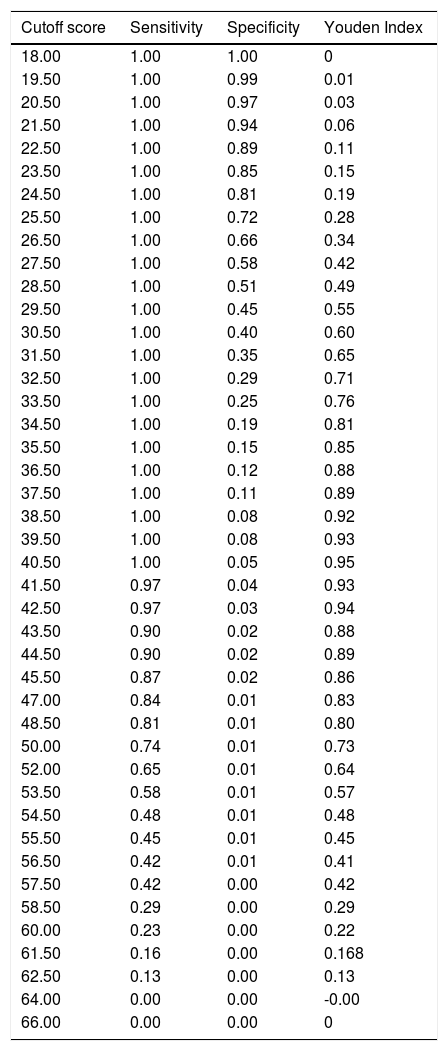
Diagnostic accuracy of the SHAIThe SHAI total score revealed a high AUC, indicating excellent discriminatory power (AUC=.99; 95% confidence interval=.98 to .99). As Table 6 shows, a SHAI total cutoff score of 40.5 resulted in the highest Youden index, with values of 100% and 95% for sensitivity and specificity, respectively. This score corresponded to the 95th percentile obtained in the non-clinical sample.
Sensitivity, specificity, and Youden Index for the Short Health Anxiety Inventory cutoff scores: Differentiating hypochondriacal concerns from normal concerns about health.
| Cutoff score | Sensitivity | Specificity | Youden Index |
|---|---|---|---|
| 18.00 | 1.00 | 1.00 | 0 |
| 19.50 | 1.00 | 0.99 | 0.01 |
| 20.50 | 1.00 | 0.97 | 0.03 |
| 21.50 | 1.00 | 0.94 | 0.06 |
| 22.50 | 1.00 | 0.89 | 0.11 |
| 23.50 | 1.00 | 0.85 | 0.15 |
| 24.50 | 1.00 | 0.81 | 0.19 |
| 25.50 | 1.00 | 0.72 | 0.28 |
| 26.50 | 1.00 | 0.66 | 0.34 |
| 27.50 | 1.00 | 0.58 | 0.42 |
| 28.50 | 1.00 | 0.51 | 0.49 |
| 29.50 | 1.00 | 0.45 | 0.55 |
| 30.50 | 1.00 | 0.40 | 0.60 |
| 31.50 | 1.00 | 0.35 | 0.65 |
| 32.50 | 1.00 | 0.29 | 0.71 |
| 33.50 | 1.00 | 0.25 | 0.76 |
| 34.50 | 1.00 | 0.19 | 0.81 |
| 35.50 | 1.00 | 0.15 | 0.85 |
| 36.50 | 1.00 | 0.12 | 0.88 |
| 37.50 | 1.00 | 0.11 | 0.89 |
| 38.50 | 1.00 | 0.08 | 0.92 |
| 39.50 | 1.00 | 0.08 | 0.93 |
| 40.50 | 1.00 | 0.05 | 0.95 |
| 41.50 | 0.97 | 0.04 | 0.93 |
| 42.50 | 0.97 | 0.03 | 0.94 |
| 43.50 | 0.90 | 0.02 | 0.88 |
| 44.50 | 0.90 | 0.02 | 0.89 |
| 45.50 | 0.87 | 0.02 | 0.86 |
| 47.00 | 0.84 | 0.01 | 0.83 |
| 48.50 | 0.81 | 0.01 | 0.80 |
| 50.00 | 0.74 | 0.01 | 0.73 |
| 52.00 | 0.65 | 0.01 | 0.64 |
| 53.50 | 0.58 | 0.01 | 0.57 |
| 54.50 | 0.48 | 0.01 | 0.48 |
| 55.50 | 0.45 | 0.01 | 0.45 |
| 56.50 | 0.42 | 0.01 | 0.41 |
| 57.50 | 0.42 | 0.00 | 0.42 |
| 58.50 | 0.29 | 0.00 | 0.29 |
| 60.00 | 0.23 | 0.00 | 0.22 |
| 61.50 | 0.16 | 0.00 | 0.168 |
| 62.50 | 0.13 | 0.00 | 0.13 |
| 64.00 | 0.00 | 0.00 | -0.00 |
| 66.00 | 0.00 | 0.00 | 0 |
The present study aimed to analyze the factor structure of the SHAI and its psychometric properties in a healthy adult Spanish sample and calculate the optimal cutoff point to identify clinically significant health anxiety symptoms. Confirmatory factor analysis indicated that the two-factor model described in the original version of the scale (Salkovskis et al., 2002), the two-factor model proposed by Wheaton et al. (2010), and the three-factor model suggested by Abramowitz, Deacon et al. (2007) provided an adequate data fit. In light of the results obtained, we decided to maintain the two-factor model proposed originally by Salkovskis et al. (2002), based on parsimony and the greater support found in the literature for this structure, as was indicated in the Introduction section. The two-factor model includes 14 items that evaluate the perceived likelihood of becoming ill (Illness likelihood) and 4 items that assess the perception of the negative consequences of an illness (Negative consequences of illness).
Overall, our findings suggest good internal consistency of the Spanish version of the SHAI. The internal consistency of the SHAI total scale was similar to what was found in other studies (Morales et al., 2016), although some studies have reported slightly higher internal consistency (α range: .91-.96) (Abramowitz, Olatunji et al., 2007; Kocjan, 2016). Furthermore, the Illness likelihood subscale demonstrated adequate internal consistency, whereas the Negative consequences of illness subscale only showed acceptable internal consistency. Overall, these results are congruent with those reported in the original study by Salkovskis et al. (2002) and other studies (e.g., Morales et al., 2015; te Poel et al., 2017; Zhang et al., 2015) that have consistently reported that the Negative consequences of illness subscale shows a lower internal consistency. This result might be due, at least in part, to the reduced number of items on the subscale. In addition, the SHAI subscales were relatively independent, which means that each of them assesses a related but distinct dimension of health anxiety.
Our findings support the convergent and divergent validity of the SHAI and its subscales. Specifically, the SHAI total score and the Illness likelihood subscale were strongly associated with a widely used measure of hypochondriacal symptoms, the Whiteley Index, but they were only moderately associated with other psychological constructs different from health anxiety (i.e., obsessive-compulsive symptoms, worry, anxiety sensitivity, and depression). Similarly, Abramowitz, Olatunji et al. (2007) found significant associations (strong to moderate) between the SHAI subscales and theoretically related constructs (e.g., body vigilance, worry), and low associations with other psychopathology measures. The Negative consequences of illness subscale was moderately associated with all the symptom measures. These results are also congruent with other studies that have shown moderate associations between the SHAI total score and Illness likelihood and Negative consequences of illness subscales and anxious and depressive symptoms (Kocjan, 2016; Zhang et al., 2015). The evidence of construct validity is more convincing for the SHAI-total score and the Illness likelihood subscale because the associations with hypochondriacal symptoms are clearly higher than with the other measures. However, the Negative consequences of illness subscale maintained similar correlations with all the other measures, which supports its discriminant validity, but not its convergent validity.
Regarding the demographic variables, our data indicate that younger people scored higher on the SHAI total scale and the Illness likelihood subscale, thus showing higher health anxiety symptoms. Nonetheless, it should be noted that the size of the association was weak, as in the Abramowitz, Deacon et al. (2007) study. By contrast, the Dutch study of the SHAI found a negative association between age and the Negative consequences of illness subscale (te Poel et al., 2017), and other studies in adult samples (Abramowitz, Olatunji et al., 2007; Wheaton et al., 2010) and adolescents (Morales et al., 2015, 2016) did not find differences between the SHAI scores and age. Overall, the results for the relationships between age and the SHAI scores are not consistent across studies. Something similar occurs in the case of gender, with some studies reporting higher scores in women, but with small effect sizes (Abramowitz, Deacon et al., 2007; Morales et al., 2015, 2016; te Poel et al., 2017), whereas other studies (Abramowitz, Olatunji et al., 2007; Wheaton et al., 2010), as in the current one, did not find gender differences.
An important aspect of the usefulness of a self-report that assesses clinical vs non-clinical symptoms is its potential ability to differentiate patients from non-patients. Our results showed that hypochondriacal patients obtained higher scores on the SHAI and its subscales than healthy participants, which indicates that the questionnaire has significant divergent and construct validity. Salkovskis et al. (2002) found a similar result when comparing the hypochondriacal patients’ scores in their study to the scores of a community sample.
As for the accuracy of the SHAI-total score in differentiating patients with hypochondriasis from non-patients, we found that a cutoff point of 40.5 differentiates between those who are strongly concerned about their health status and those with a normal concern for their health. This score was similar to the reported in the Abramowitz, Olatunji et al. (2007) study to differentiate patients with hypochondriasis from patients with anxiety disorders, but it is lower than the cutoff scores reported in other studies. For example, Kocjan (2016) suggested a total score of 45 to identify problematic health anxiety. Other authors reported lower cutoff scores, from 33 to 26 to identify people with excessive concerns about health (Zhang et al., 2015). Nonetheless, as different authors stated (Alberts et al., 2013; Hedman et al., 2015), although the aforementioned cutoff scores are widely used, there are not enough data supporting them. The different studies used diverse samples (e.g., from undergraduate students to cardiovascular patients), or they did not even specify the population in which the cutoff score was obtained or the rationale applied to calculate it. In our study, the cutoff score obtained is very similar to the one obtained by Abramowitz, Olatunji et al. (2007), which, as far as we know, is the only published study that used a sample of hypochondriacal patients in their analyses, as in the current study.
This study has some limitations. The retrospective and cross-sectional design could be influential in introducing some respondent biases when faced with a self-report, thus preventing us from drawing causal inferences about the relationships between health anxiety and other symptoms apart from hypochondriacal ones. The limited sample size of patients with hypochondriasis is another limitation, which means that caution should be used in generalizing the findings to broader and more representative samples. Moreover, the absence of a control group of patients with a disorder different from hypochondriasis keeps us from making suggestions about the specificity of health anxiety to patients with hypochondriasis.
Despite the aforementioned limitations, the present study provides support for the two-factor structure of the SHAI, as proposed by its original authors (Salkovskis et al., 2002). Moreover, the Spanish version of the SHAI has been shown to be sensitive in assessing the range of health concerns from normality to severity, and it offers a cutoff point to reliably differentiate between non-clinical and clinically significant health anxiety symptoms. This cutoff score can be used not only in clinical practice for screening purposes, but also in epidemiological studies. Taken together, our findings support the SHAI's adequacy for use in Spanish adult community samples.
FundingThe Ministry of Science, Innovation and Universities of Spain [Grant FPU 14/02795 & Grant RTI2018-098349-B-I00] supported this work. The Ministry of Science, Innovation and Universities of Spain played no role in the study design; data collection, analysis or interpretation; the writing of the report; or the decision to submit this paper for publication.