A measure of Behavioral Activation (BA) is highly recommended when evaluating BA treatment effects for smokers with depression. Recently, a short version of the Behavioral Activation for Depression scale (BADS-SF) has been developed as a means of assessing changes in activation and avoidance patterns. To date there is no validated version of this questionnaire in Spanish. This study sought to adapt the BADS-SF to a Spanish population of depressed smokers. Method A sample of 169 smokers (72.2% female) with elevated depressive symptomatology completed the BADS-SF. Results A bi-factorial structure was obtained: Activation and Avoidance. Results indicated an acceptable internal consistency for both the Activation (ω = .85) and the Avoidance subscales (ω =.70). Overall, convergent validity was obtained with Activation and Avoidance subscales being related to other depression-related measures such as depressive symptomatology (Activation r = −.29; Avoidance r = .35), environmental reward (Activation r = .40; Avoidance r = −.41) and, nicotine dependence (Avoidance r = .23). This latter variable was the only one not showing a statistically significant association with the Activation factor (r = −.12). Conclusions The Spanish BADS-SF can be considered as a reliable and valid instrument when assessing behavioral activation among clinically depressed smokers.
Las medidas de Activación Conductual (AC) resultan necesarias en la evaluación de los tratamientos dirigidos a fumadores con depresión. Recientemente, una versión corta de la escala de AC (BADS-SF) ha sido desarrollada para evaluar los cambios en la activación y evitación. El objetivo de este trabajo fue adaptar la versión corta de la escala de AC (BADS-SF) a la población española de fumadores deprimidos. Método Una muestra de 169 fumadores (72,2% mujeres) con síntomas elevados de depresión completó el BADS-SF. Resultados Se obtuvo una estructura bifactorial: Activación y Evitación. Los resultados indicaron una consistencia interna aceptable para las subescalas Activación (ω = 0,85) y Evitación (ω = 0,70). Se obtuvo evidencia de validez convergente mediante correlaciones significativas entre las subescalas del BADS-SF, la depresión (Activación r = −0,29; Evitación r = 0,35), el nivel de recompensa obtenido del entorno (Activación r = 0,40; Evitación r = −0,41) y la dependencia a la nicotina (Evitación r = 0,23). La última variable fue la única que no mostró una relación estadísticamente significativa con el factor Activación (r = −0,12). Conclusiones La versión española del BADS-SF puede ser considerada como una medida fiable y un instrumento válido para evaluar AC en pacientes fumadores con depresión.
Smoking produces a heavy economic burden worldwide, especially in Europe and North America where the tobacco epidemic accounts for 5.7% of global health expenditures (Goodchild, Nargis, & Tursan d’Espaignet, 2018). In Spain, despite there having been a slight decrease in the percentage of daily smokers over the last decade (from 32.5% in 2005 to 30.8% in 2015) (National Plan of Drugs, 2017), depression seems to have increased in this population (Becoña, López-Durán, Fernández del Río, & Martínez, 2014). This comorbidity leads not only to poor cessation outcomes (Weinberger et al., 2016), but also causes poor quality of life as evidenced by a high number of hospitalizations (Baker, 2017).
Against this background, research into smoking and depression is currently focused on the development of effective strategies to promote abstinence (López-Núñez, Martínez-Loredo, Weidberg, Pericot-Valverde, & Secades-Villa, 2016; Secades-Villa et al., 2015). In particular, behavioral activation (BA) as an adjunct to smoking cessation treatments has been recently recognized as a promising intervention in terms of mood improvement and cessation rates (MacPherson, Collado, Lejuez, Brown, & Tull, 2016; MacPherson et al., 2010; Pérez-Álvarez, 2012; Ross et al., 2016; van der Meer, Willemsen, Smit, Cuijpers, & Schippers, 2010). Treatments based on BA emphasize the importance of reengaging individuals with pleasant and adaptive activities while overcoming avoidance patterns as the main therapy component (Barraca, 2012; Chan, Sun, Tam, Tsoi, & Wong, 2017). Consequently, evaluating changes in activation and avoidance patterns is of great interest.
Accordingly, the Behavioral Activation Scale (BADS) has been developed as an instrument to assess frequency of activation, escape and avoidance behaviors throughout BA therapy (Kanter, Mulick, Busch, Berlin, & Martell, 2006). Although this scale originally consisted of 29 items, a 9-item short version has been recently cross-culturally validated (Manos, Kanter, & Busch, 2010; Manos, Kanter, & Luo, 2011; Wagener, Van der Linden, & Blairy, 2015). The abbreviated version of BADS (BADS-SF) allows health providers to swiftly and effectively monitor BA changes in-treatment; especially when added to other smoking-related and sociodemographic measurements. Research has reported that BADS-SF possesses adequate psychometric properties across both non-clinical (Raes, Hoes, Van Gucht, Kanter, & Hermans, 2010; Wagener et al., 2015) and clinically depressed individuals (Fuhr, Hautzinger, Krisch, Berking, & Ebert, 2016). Interestingly, it has shown good construct validity through high correlations with measures of depression and predictive validity over a one-week period (Manos et al., 2011).
Notwithstanding this, the BADS-SF has not yet been validated in the context of Spanish-speaking depressed smokers. Given that Spanish is the third most widely spoken language worldwide, and because of the increasing migratory movements of this population to the US, having adequate assessment tools for BA monitoring becomes essential in order to yield evidence on treatment efficacy for this particular group. Despite the existence of a validated version of the 25-item BADS scale in Spanish (Barraca, Pérez-Álvarez, & Lozano Bleda, 2011), the adaptation of BADS to a shorter format offers health providers a more efficient tool for monitoring activation levels in each therapy session.
This study sought to adapt the BADS-SF to a sample of Spanish depressed smokers and examine whether support for its psychometric properties is achieved in this population. We examined for reliability and validity evidence based on its internal structure and relation to other variables.
MethodParticipantsThe data set comprised 169 smokers (72.2% female) with moderate to severe depressive symptoms (BDI = 28.70, SD = 9.31). Most participants had a current depression diagnosis (73.8%). Mean age was 53 years old (SD = 9.62). Most of the sample (52.7%) reported having secondary studies. Mean number of cigarettes per day was 23 (SD = 9.26), mean score on Fagerström Test for Nicotine Dependence (Becoña & Vázquez, 1998) was 6.45 (SD = 1.85), mean expired air carbon monoxide (CO) was 22.96 (SD = 12.79) and mean urine cotinine levels were 2396.88 (SD = 1193.60).
ProcedureThe study sample was recruited from the community for a randomized controlled trial investigating the effects of three depression-focused smoking cessation treatments. Participants were recruited by means of flyers, radio and newspaper advertisements posted around the region of Asturias, Spain. Interested individuals were referred to contact the Clinical Unit of Addictive Behaviors by either phone or e-mail and scheduled for an in-person interview. None of the participants who initially contacted the research staff refused to participate in the intake assessment. Data for this study were collected prior to the intervention at the baseline assessment following the Code of Ethics of the World Medical Association (Declaration of Helsinki). Written informed consent was obtained prior to initiation and this study was approved by the Research ethics committee of the Principality of Asturias (n°124/15).
InstrumentsIndividuals completed an ad hoc questionnaire which collected data on sociodemographic variables (e.g., age, sex, and educational level) and smoking-related characteristics (e.g., number of daily cigarettes, nicotine dependence). All participants were asked to provide a urine and CO sample.
Behavioral Activation for Depression Scale Short-form (BADS-SF). The short form of the Behavioral Activation for Depression Scale (The BADS-SF; Manos et al., 2011) was used to assess experienced pleasure from daily activities over the past week. This scale contains 9 items and demonstrated good internal consistency (α = .82) and validity evidence based on relations to other depression-related variables (Manos et al., 2010; Manos et al., 2011). This instrument yields a total score and two subscales: Activation (items 2, 3, 4, 5, 9) and Avoidance (items 1, 6, 7, 8). In this study sample, the internal consistency examined by McDonald's coefficient omega (ω) was .85 and .63 for the Activation and Avoidance subscales, respectively. Respondents are provided a seven-point scale that ranges from 0 (not at all) to 6 (completely). The Spanish version of the BADS-SF was developed following the guidelines for translating and adapting tests posed by the International Test Commission (Hambleton, Merenda, & Spielberger, 2005; International Test Commision, 2017; Muñiz, Elosua, & Hambleton, 2013). Items in the Spanish version of BADS-SF were presented in the same order as the original.
Environmental Reward Observation Scale (EROS). The Spanish adapted version of the Environmental Reward Observation Scale (EROS; Barraca & Pérez-Álvarez, 2010) was used as a measure of response-contingent positive reward. Internal consistency for the study sample was (ω = .68). This instrument comprises 10 items and has shown high internal consistency (α = .86) and high correlations with the Beck Depression Inventory (BDI-II), and BADS (Barraca & Pérez-Álvarez, 2010).
Beck Depression Inventory (BDI-II). Depressive symptomatology was assessed using the Spanish version of the Beck Depression Inventory (Sanz, Perdigón, & Vázquez, 2003). BDI-II good internal consistency in our study sample was (ω = .88). The Spanish adaptation of BDI-II has shown internal consistency (α = .87). Total scores range between 0 and 63. A score between 0 and 13 represents normal to minimal depression, 14 to 19 indicates mild depression, 20 to 28 moderate depression, and scores above 29 suggest severe depression.
The Structured Clinical Interview SCID-CV. The structured clinical interview for DSM-IV Disorders (SCID-CV; First, Spitzer, Williams, & Gibbon, 1999) was used to detect a current depression diagnosis based on the DSM-IV-TR diagnostic guidelines. This instrument is one of the most widely used instruments for diagnosis purposes and presents acceptable reliability coefficients (.61-.80) (Zanarini & Frankenburg, 2001; Zanarini et al., 2000).
Nicotine Dependence. Nicotine dependence severity was assessed by the Fagerström Test for Nicotine Dependence (FTND) (α = .66) (Becoña, Gómez-Durán, Álvarez-Soto, & García, 1992). Scores range from 0 (very low) to 10 (high severity). Internal consistency in the sample of smokers with depression was ω = .60. This instrument was reported as a useful measure to predict craving severity, and smoking relapse.
Biochemical assessment. All participants provided CO and urinalysis samples to confirm smoking status. These measures were collected in the clinic using a piCO Smokerlyzer monitor (Bedfont Scientific Ltd., Rochester, UK) and the BS-120 chemistry analyzer (Shenzhen Mindray Bio-medical Electronics Co. Ltd., Shenzhen, P. R. China). Readings of ≥4 parts per million (ppm) on CO samples and ≥80 nanograms per milliliter (ng/ml) indicated smoking status.
Data analysisExploratory factor analysis (EFA) with Unweighted Least Squares (ULS) as the extraction method and Promin rotation was carried out to explore the factorial structure of the BADS-SF. The polychoric correlation matrix was used in the EFA. The procedure to ascertain the number of recommended extracted factors was the optimal implementation of Parallel Analysis, using 500 random correlation matrices (Timmerman & Lorenzo-Seva, 2011). As this represents the first attempt to examine the internal structure of the BADS-SF among depressed smokers, the EFA was deemed eligible over other methods due to it being regarded as adequate when exploring factorial solutions in an unstudied sample, such as the one included in this study (Fabrigar & Wegener, 2012; Ferrando & Lorenzo-Seva, 2017). For the factorial solution, the following fit indices were examined: the comparative fit index (CFI) the root mean square of the residuals (RMSR), the root mean square error of approximation (RMSEA), and the goodness of fit index (GFI). Acceptable fits are considered when a GFI, CFI of ≥ .95 (Ruiz, Pardo, & San Martín, 2010), and a RMSR of ≤ .08 are obtained (Hu & Bentler, 1999). Following the recommendations of Ferrando and Anguiano-Carrasco (2010) RMSEA values between .05 and .08 were considered adequate. Cutoff points of ≥ .40 were considered for factor loading (Brown, 2015).
Analyses of reliability were also performed for each of the BADS-SF subscales through Cronbach¿s alpha. Due to its adequacy for Likert-type responses, analyses of reliability were also performed for both Activation and Avoidance subscales through McDonald's Omega (McDonald, 1999). BADS-SF items were examined through the discrimination indices and the alpha if the item is removed. These latter analyses were performed separately for each subscale, as the two BADS-SF factors have been shown to be uncorrelated and thus reflect different BA constructs.
For examining convergent validity evidence, we carried out two-tailed Pearson correlations between the Spanish version of BADS (Activation and Avoidance sub-scores), other depression-related measures (BDI-II, EROS), and FTND. A multiple analysis of variance (MANOVA) was also conducted to examine inter-group differences for smokers with mild-to-moderate and severe depression on the Activation and Avoidance patterns. Following the recommendations posed by Sanz (2013), individuals with mild-to-moderate depression were those scoring between 14 and 28 in the BDI-II. Patients scoring ≥ 29 were classified as severely depressed.
Effect size was calculated using eta square (η2). Values of .01, .06, and .14 indicate small, medium, and large effects (Cohen, 1988).
IBM SPSS Statistics for Windows (version 22.0, IBM Corp, Armonk, NY, 2011) and FACTOR (version 9.20, Tarragona, Spain, 2006) for EFA analysis were used.
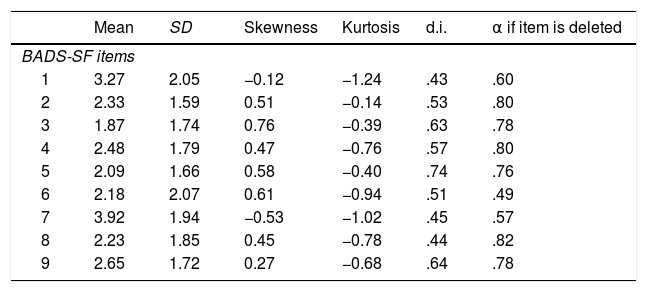
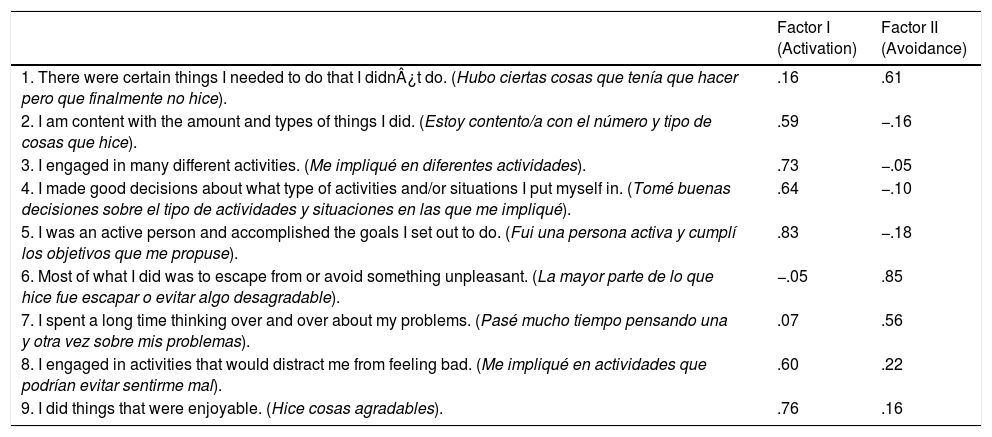
ResultsValidity evidence based on internal structureAnalysis of univariate normality of the BADS-SF items indicated no deviation from normality. Skewness ranged from −.53 to .76 and kurtosis ranged between −1.244 to −.140 (see Table 1). The Kaiser-Meyer-Olkin index value was .77 and the Bartlett Sphericity test was statistically significant (χ2 = (471.6, 36), p < .001). EFA analysis recommended the extraction of two factors “Activation” (items 2, 3, 4, 5, 8, 9) and “Avoidance” (items 1, 6, 7) (See Table 2). An explained variance of 54.9% and 26.2% was obtained for Activation and Avoidance, respectively. Correlation analysis between Activation and Avoidance did not reach statistical significance (r = −.075). Overall, the factor structure of BADS-SF showed a good fit (GFI = .99; CFI = .98; RMSR = .06; RMSEA = .07).
Descriptive statistics for BADS-SF items.
| Mean | SD | Skewness | Kurtosis | d.i. | α if item is deleted | |
|---|---|---|---|---|---|---|
| BADS-SF items | ||||||
| 1 | 3.27 | 2.05 | −0.12 | −1.24 | .43 | .60 |
| 2 | 2.33 | 1.59 | 0.51 | −0.14 | .53 | .80 |
| 3 | 1.87 | 1.74 | 0.76 | −0.39 | .63 | .78 |
| 4 | 2.48 | 1.79 | 0.47 | −0.76 | .57 | .80 |
| 5 | 2.09 | 1.66 | 0.58 | −0.40 | .74 | .76 |
| 6 | 2.18 | 2.07 | 0.61 | −0.94 | .51 | .49 |
| 7 | 3.92 | 1.94 | −0.53 | −1.02 | .45 | .57 |
| 8 | 2.23 | 1.85 | 0.45 | −0.78 | .44 | .82 |
| 9 | 2.65 | 1.72 | 0.27 | −0.68 | .64 | .78 |
Note. Both discrimination indices and α if item is deleted were calculated in relation to its respective BADS-SF subscale. SD: standard deviation; d.i.: discrimination index.
Factor loadings of the Spanish BADS-SF items.
| Factor I (Activation) | Factor II (Avoidance) | |
|---|---|---|
| 1. There were certain things I needed to do that I didn¿t do. (Hubo ciertas cosas que tenía que hacer pero que finalmente no hice). | .16 | .61 |
| 2. I am content with the amount and types of things I did. (Estoy contento/a con el número y tipo de cosas que hice). | .59 | −.16 |
| 3. I engaged in many different activities. (Me impliqué en diferentes actividades). | .73 | −.05 |
| 4. I made good decisions about what type of activities and/or situations I put myself in. (Tomé buenas decisiones sobre el tipo de actividades y situaciones en las que me impliqué). | .64 | −.10 |
| 5. I was an active person and accomplished the goals I set out to do. (Fui una persona activa y cumplí los objetivos que me propuse). | .83 | −.18 |
| 6. Most of what I did was to escape from or avoid something unpleasant. (La mayor parte de lo que hice fue escapar o evitar algo desagradable). | −.05 | .85 |
| 7. I spent a long time thinking over and over about my problems. (Pasé mucho tiempo pensando una y otra vez sobre mis problemas). | .07 | .56 |
| 8. I engaged in activities that would distract me from feeling bad. (Me impliqué en actividades que podrían evitar sentirme mal). | .60 | .22 |
| 9. I did things that were enjoyable. (Hice cosas agradables). | .76 | .16 |
Note. Factor loadings ≥.40 are indicated in bold.
Reliability analyses showed acceptable internal consistency for the Spanish version of the BADS-SF. McDonald's Omega was .85 and .70 for Activation and Avoidance, respectively. Cronbach¿s alpha was .82 and .66 for Activation and Avoidance, respectively. All items showed discrimination indices higher than .40 (see Table 1). Analysis of reliability for the Activation subscale showed that deleting item 1 slightly increased the internal consistency from .82 to .83. Nonetheless, the internal consistency of the Avoidance subscale did not improve with the deletion of any item.
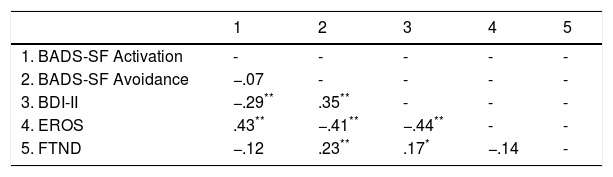
Validity evidence based on relations to other variablesTable 3 shows Pearson¿s correlations between the BADS-SF subscales, BDI-II, EROS, and FTND scores. Results showed that the BADS-SF Activation subscale was positively correlated with EROS and negatively correlated with depression; as activation increased, scores in EROS increased, but depression decreased. Avoidance subscale was positively correlated with depression and FTND scores but negatively correlated with EROS.
Pearson's correlations between the Spanish BADS-SF, BDI-II, EROS and, FTND.
| 1 | 2 | 3 | 4 | 5 | |
|---|---|---|---|---|---|
| 1. BADS-SF Activation | - | - | - | - | - |
| 2. BADS-SF Avoidance | −.07 | - | - | - | - |
| 3. BDI-II | −.29** | .35** | - | - | - |
| 4. EROS | .43** | −.41** | −.44** | - | - |
| 5. FTND | −.12 | .23** | .17* | −.14 | - |
Note. BADS-SF = Behavioral Activation for Depression scale-short-form; BDI-II = Beck Depression Inventory II; EROS = the Environmental Reward Observation scale; FTND = The Fagerström Test for Nicotine Dependence.
Further convergent validity was obtained with the MANOVA analysis. Statistically significant differences emerged as a function of depression severity, [F (2, 166) = 14.24, p < .001, η2 = .15]. Patients presenting severe depressive symptoms presented lower Activation (M = 11.55, SD = 7.10) and higher Avoidance (M = 10.84, SD = 4.76) relative to those presenting mild to moderate depression (Activation: M = 15.57, SD = 7.50, Avoidance: M = 8.09, SD = 4.22).
DiscussionThis study sought to adapt the BADS-SF to a Spanish sample of smokers with depression and examine its psychometric properties. Due to the high prevalence of depression among smokers, the availability of the BADS-SF has relevance for both research and clinical purposes. Even though many research efforts have been conducted on depression etiology and treatment (MacPherson et al., 2016; Mathew, Hogarth, Leventhal, Cook, & Hitsman, 2017; Miret et al., 2015), few studies have been focused on developing treatment strategies that simultaneously target comorbid tobacco use and depression. Consequently, it is expected that this validation will enable the proliferation of research on smoking cessation treatments for depressed individuals. Results showed that the BADS-SF is a valid and reliable tool for assessing behavioral activation levels among clinically depressed smokers.
Consistent with previous validation studies of the BADS-SF (Fuhr et al., 2016; Manos et al., 2011; Wagener et al., 2015), results yielded support for the originally proposed bi-factorial structure; Activation and Avoidance. Nonetheless, both factors were composed of different items. Activation included items 2, 3, 4, 5, 8 and, 9 whereas Avoidance included items 1, 6 and 7. The factorial solution obtained herein is also consistent with the theoretical basis of BA (Dimidjian, Barrera, Martell, Muñoz, & Lewinsohn, 2011). Therapists using this treatment approach pay close attention to the function of behavior and the aversive stimulation. BA is aimed at both mitigating avoidance behaviors (e.g., smoking) and increasing positive and rewarding activities (e.g., engaging in sport activities), thus offering congruency with both the two-factorial solution and the content of their BADS-SF items.
The factor structure showed a better fit than the originally proposed two factor model. Acceptable reliability was observed for the Activation subscale (ω = .85) which is higher than the one previously reported by Fuhr et al. (2016) among individuals with elevated depressive symptoms. However, internal consistency for the Avoidance subscale (ω = .65) was lower compared to a prior validation study on BADS-SF (α = .75) (Wagener et al., 2015) but slightly higher than the one reported by Fuhr et al. (2016) (α = .62). Consequently, it might be that an adjustment of this scale (e.g., adding a few items) would improve (Danner et al., 2016) its internal consistency, but not necessarily. In this context, future efforts aimed at improving the psychometric properties of BADS-SF should not add ineffective items such as item 1. As previously shown, the inclusion of negative items adds a different dimension to the outcome and invalidates the reliability and validity of the proposed model (Solis Salazar, 2015; Suárez-Álvarez et al., in press). In this study Activation and Avoidance subscales were not significantly correlated one another, suggesting that these two subscales are orthogonal or measuring two different constructs. These results suggest the need to use the Activation subscale rather than use the Avoidance subscale, mainly due to it including only three items.
The BADS-SF construct validity was demonstrated as evidenced by moderate to large correlations between the BADS-SF subscales and other depression-related measures (BDI-II, EROS, and FTND). This is an important finding that confirms the strong association between high activation levels and high positive reinforcement obtained from pleasant activities (Collado, Calderón, MacPherson, & Lejuez, 2016; Gawrysiak, Nicholas, & Hopko, 2009). These findings also support previous validation studies and are in line with research indicating that depressed individuals present Avoidance patterns while being involved in barely pleasant activities (Ichikura et al., 2017; Nasrin, Rimes, Reinecke, Rinck, & Barnhofer, 2017; Wu et al., 2017). The fact that FTND scores were positively associated with depression and negatively with EROS, aligns with existing research stressing the role of tobacco cigarettes as a coping strategy for relieving emotional discomfort (Leventhal & Zvolensky, 2015).
This study is subject to at least three limitations. First, a relatively small sample size was included in this study and thus results obtained herein represent preliminary data. Nevertheless, the number of respondents was more fifteen times the number of items contained in the BADS-SF which overcomes the minimum required for validation studies (Price, 2016). Second, individuals with other substance abuse disorders (e.g., alcohol) and severe psychiatric disorders such as schizophrenia were discarded, thus results can be only generalized to the population of cigarette smokers with depression. Third, we did not evaluate the capacity of the BADS-SF to predict Activation/Avoidance changes to BA treatment.
Despite these limitations, results show that the BADS-SF is a reliable, valid and useful questionnaire for examining behavioral activation levels in smokers with depression. Due to its brevity, this scale offers health providers and researchers an efficient way of evaluating behavioral activation. Although the EFA identified 2 subscales (Activation and Avoidance), we highly encourage the use of the Activation sub-score instead of using each of them in isolation. Given that the Avoidance subscale comprises only three items, we recommend using other reliable and valid avoidance measures (e.g., CBAS; Hernández-Guzmán et al., 2009). Further confirmatory studies on BADS-SF among depressed smokers are warranted.
FundingThis research was supported by the Spanish Ministry of Economy and Competitiveness, the European Regional Development Fund (Grant PSI2015-64371-P. MINECO/FEDER; Grant PSI-2014-56114-P), and by the Predoctoral FPI Grant (Ref. BES-2016-076663). This institution had no role in the study design, collection, analysis or interpretation of the data, writing the manuscript, or the decision to submit the paper for publication.