Insufficient education and training in nursing programs has led to nurses in the field knowing very little in order to assist a breastfeeding mother. Several studies recommend implementation of effective breastfeeding training in all undergraduate curricula that lead to nursing and other healthcare degrees.
ObjectiveTo analyze the development of an objective structured clinical examination (OSCE) to measure breastfeeding clinical skills and the preliminary outcomes of its implementation.
MethodParticipants for this pilot study were 23 undergraduate nursing students. The breastfeeding OSCE consisted of 10 stations where students performed different clinical skills under a simulated environment. The clinical skills being assessed in each station ranged from performing proper manual milk expression to correctly using a breast pump on a mannequin's breast. Observers in each station completed a checklist which assessed each student's clinical ability to complete that task correctly. Students conducted an evaluation of the training immediately after completing the OSCE using a structured online questionnaire.
ResultsThe stations with the highest score were: interventions for sore, leaking, and inverted nipples (station 4, M=2.57, SD=.843, range 1–3) and indicators of adequate latching (station 6; M=7.09, SD=1.443, range 4–8). The stations with the lowest scores were: pump set up to breast and how to remove the infant from the breast (station 1, M=7.96, SD=1.745, range 4–10), and breastfeeding positions (station 5, M=1.65, SD=.714, range 0–2).
ConclusionThe OSCE has been positively evaluated for objectivity in student assessment and provides a ‘hands on’ approach to assessing clinical competence. Scores and student feedback suggests that the OSCE can be a valuable tool to be used in courses of any nursing or health-related undergraduate curriculum.
Insuficiente educación y entrenamiento clínico de las enfermeras recién graduadas ha llevado a que estas no se sientan capacitadas para asistir a la madre lactante. Varios estudios recomiendan la implementación de entrenamiento de lactancia en todos los planes de estudio de pregrado que conlleven a enfermería y otros títulos en el área del cuidado de la salud.
ObjetivoAnalizar el desarrollo de un examen clínico objetivo estructurado (ECOE) para medir las habilidades clínicas de lactancia materna y los resultados preliminares de su aplicación.
MétodoLos participantes para este estudio piloto fueron 23 estudiantes de enfermería de pregrado. El ECOE de lactancia consistió en 10 estaciones donde los estudiantes implementaron diferentes habilidades clínicas bajo un ambiente simulado. Las habilidades clínicas examinadas en cada estación variaron desde extracción manual de leche materna hasta el correcto uso de la bomba extractora en el seno de un maniquí. Observadores en cada estación completaron una lista que juzgaba la habilidad clínica de cada estudiante para completar la tarea correctamente. Estudiantes condujeron una evaluación del entrenamiento inmediatamente después de completar el ECOE usando una encuesta estructurada en línea.
ResultadosLas estaciones con las puntuaciones más altas fueron: intervención en pezones adoloridos, goteo de leche materna de los pezones invertidos (estación 4, promedio=2.57, desviación estándar=.843, rango 1-3) e indicadores de agarre adecuado del niño al pecho materno (estación 6, promedio=7.09, desviación estándar=1.443, rango 4-8). Las estaciones con las puntuaciones más bajas fueron: cómo manejar la bomba de extracción de leche y cómo destetar al niño del pecho materno (estación 1, promedio=7.96, desviación estándar=1.745, rango 4-10) y las posiciones para la lactancia (estación 5, promedio=1.65, desviación estándar=.714, rango 0–2).
ConclusiónEl ECOE ha sido evaluado positivamente por su objetividad en la evaluación de estudiantes y porque funciona adecuadamente para medir las competencias clínicas. Los puntajes y las evaluaciones de los estudiantes sugieren que el ECOE puede ser una herramienta valiosa para ser utilizada en otros cursos de enfermería o planes de estudio de pregrado relacionados con el área de salud.
Supporting, promoting, and protecting lactation and breastfeeding has emerged as a contemporary public health initiative.1 Breastfeeding combines two crucial elements of infant survival: nurturing and nourishment.2 Over 40 years of strong evidence acknowledges that breast milk is the ideal form of infant nutrition.3,4 According to the Lancet Child Survival Series, breastfeeding is ranked first among the top 15 preventative child survival interventions and it is recommended exclusively for the first 6 months.5
The World Health Organization (WHO)/United Nations Children's Fund (UNICEF) developed a Global Strategy in 2002, which serves as a framework of actions necessary to protect, support, and promote adequate feeding of all infants and children worldwide.6 The Baby-Friendly Hospital Initiative (BFHI) is one out of nine targets of the Global Strategy for Infant and Child Feeding and consists of 20h of breastfeeding training based on The Ten Steps to Successful Breastfeeding.6,7 These 20h of breastfeeding training are considered by the WHO/UNICEF as the minimum time of instruction that health care workers caring for a lactating mother should receive.8 Maternity facilities that successfully implemented the Ten Steps and the International Code of Marketing of Breast-milk Substitutes are rewarded and recognized as a “Baby-Friendly” facility.9 Whether maternity hospitals and birthing centers decide to earn the Baby-Friendly designation, the ultimate goal is to implement the Ten Steps and to train the maternal–child staff to effectively practice the steps.10 In the US alone, there are 182 hospitals and birthing centers that hold the Baby Friendly designation in which 6.9% of births occur.9 Globally, there are about 152 countries that have baby-friendly facilities; unfortunately, according to the WHO11 no more than 40% of infants fewer than 6 months of age are breastfed exclusively.
Breastfeeding has become a prevalent topic due to recent studies that have found a deficit in the knowledge of healthcare workers in this area.12 Nurses are the largest group of maternal–child staff that support mothers and babies to meet their lactation and breastfeeding needs.13 However, insufficient training in nursing programs has led to nurses in the field knowing very little in order to assist a mother. A recent study showed that lack of breastfeeding education has resulted in nursing students not knowing essential information needed to assist a breastfeeding mother.14 Several studies recommend implementation of effective training on breastfeeding support in all undergraduate curricula that lead to nursing and other healthcare degrees.14,15
Besides acquiring new knowledge, nurses need to practice and develop clinical skills in order for them to gain confidence and assist a mother breastfeed in the real world.14 One methodology described in the literature that facilitates the development of skills among health care workers is the Objective Structured Clinical Examination (OSCE). The OSCE was first introduced by Harden in the 1970s as a way to assess clinical skills of medical students objectively, and has then been considered a strategy to assess clinical skills among an array of healthcare fields.16 The students in the OSCE progress through a number of timed stations as they perform the skills required of them from each station in which they are also scored based on their performance.16 An examiner is present at each station to assess students as they demonstrate specific sets of skills and behaviors in a simulated environment.17 This methodology is flexible and can be used in different settings (e.g. clinical, simulation, classroom).16,17
The OSCEs, according to Smith et al.,17 have been favorably appraised in the literature and provide the potential for a holistic approach to assess clinical competence if they are well planned, achieve content validity, and are then properly executed. OSCE's are a meaningful assessment experience and opportunity for learning clinical skills.16
The OSCE methodology can increase the knowledge and skills of healthcare students who provide support to breastfeeding mothers. Healer18 implemented the OSCE methodology with midwifery students from United Kingdom. In that study, the OSCE consisted of 5 scenarios of 15min each where the students needed to listen, observe, and evaluate a given situation (e.g. milk supply, breast engorgement, sore nipples, supplementation with formula, and support with breastfeeding). Each student participated in role playing of one scenario and the scenarios were video recorded. The author concluded that the students’ knowledge increased and were more capable of providing breastfeeding support to women. In addition, Smith et al.17 used a two-station, 20-min duration OSCE (10min each station) to assess breastfeeding competences among midwifery students. The scenarios included role playing about lactation and infant feeding with a client (e.g. usual/standard such as first feed post birth and other scenario with mastitis or engorgement). The results showed that the OSCE was an appropriate and valuable form of assessment for this topic and that the students increased their levels of breastfeeding skills and knowledge. The studies found in the literature evaluated the OSCE as an educational experience for the students and there was not a consensus about the most effective ways to implement the OSCE methodology among students. After an extensive literature search, the research team did not find studies that implemented the OSCE methodology for breastfeeding with nursing students. The purpose of this study is to analyze the development of an OSCE to increase breastfeeding clinical skills and the preliminary outcomes of its implementation.
MethodThis is a quantitative descriptive study with a sample of twenty three undergraduate nursing students who participated in a breastfeeding OSCE. The students were enrolled in a maternal health nursing course at the School of Nursing and Health Studies, University of Miami. Prior to the completion of the OSCE, the students completed an online Breastfeeding Training (BT) course, which consisted of five online modules using the UNICEF/WHO/BFI 20-hours breastfeeding curriculum.19 These modules provided the conceptual breastfeeding knowledge that was assessed in the OSCE. In this article, only the OSCE results will be reported. The inclusion criteria were (a) being a University of Miami undergraduate nursing student, and (b) completing the online BT modules. This study was approved by the Institutional Review Board of the University of Miami.
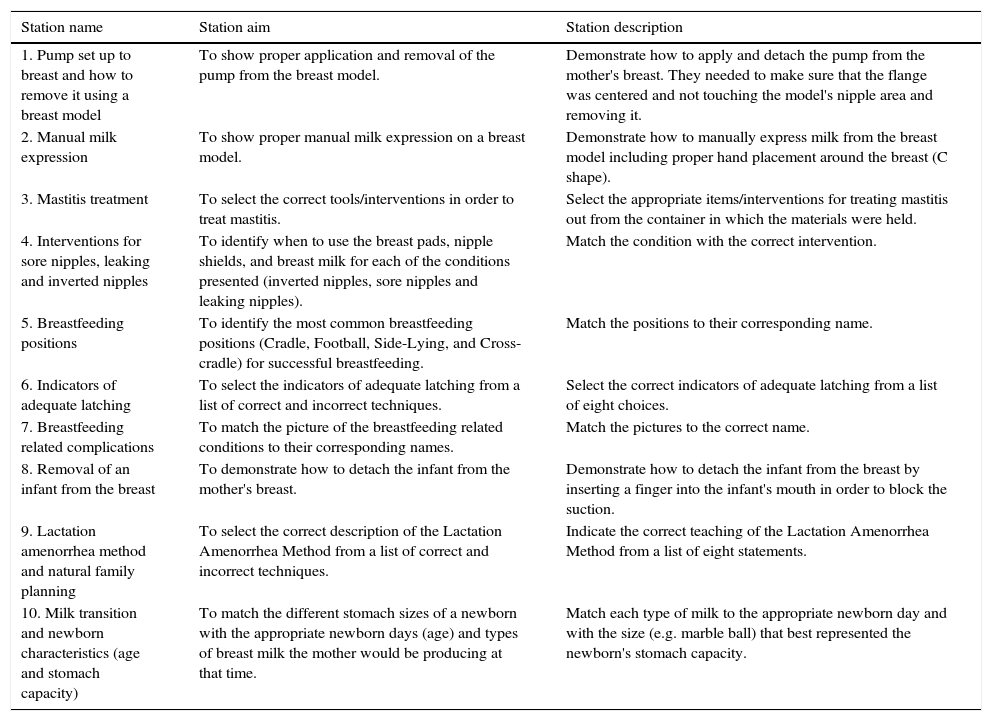
The breastfeeding OSCE consisted of 10 stations where the students performed different clinical skills (see Table 1). Each station lasted 2min, for a total of 20min. Instructions for the OSCE were given at the beginning. There was a timekeeper who indicated that the students needed to move to the next station. In addition, there was a table in each station with the instructions, required materials, and a trained observer with a checklist. The observers were responsible for completing the checklist that assessed the student's clinical skills and organizing the station after each student completed the activity (30s were assigned for this purpose). No interaction was allowed between the observer and the students.
Breastfeeding OSCE stations.
| Station name | Station aim | Station description |
|---|---|---|
| 1. Pump set up to breast and how to remove it using a breast model | To show proper application and removal of the pump from the breast model. | Demonstrate how to apply and detach the pump from the mother's breast. They needed to make sure that the flange was centered and not touching the model's nipple area and removing it. |
| 2. Manual milk expression | To show proper manual milk expression on a breast model. | Demonstrate how to manually express milk from the breast model including proper hand placement around the breast (C shape). |
| 3. Mastitis treatment | To select the correct tools/interventions in order to treat mastitis. | Select the appropriate items/interventions for treating mastitis out from the container in which the materials were held. |
| 4. Interventions for sore nipples, leaking and inverted nipples | To identify when to use the breast pads, nipple shields, and breast milk for each of the conditions presented (inverted nipples, sore nipples and leaking nipples). | Match the condition with the correct intervention. |
| 5. Breastfeeding positions | To identify the most common breastfeeding positions (Cradle, Football, Side-Lying, and Cross-cradle) for successful breastfeeding. | Match the positions to their corresponding name. |
| 6. Indicators of adequate latching | To select the indicators of adequate latching from a list of correct and incorrect techniques. | Select the correct indicators of adequate latching from a list of eight choices. |
| 7. Breastfeeding related complications | To match the picture of the breastfeeding related conditions to their corresponding names. | Match the pictures to the correct name. |
| 8. Removal of an infant from the breast | To demonstrate how to detach the infant from the mother's breast. | Demonstrate how to detach the infant from the breast by inserting a finger into the infant's mouth in order to block the suction. |
| 9. Lactation amenorrhea method and natural family planning | To select the correct description of the Lactation Amenorrhea Method from a list of correct and incorrect techniques. | Indicate the correct teaching of the Lactation Amenorrhea Method from a list of eight statements. |
| 10. Milk transition and newborn characteristics (age and stomach capacity) | To match the different stomach sizes of a newborn with the appropriate newborn days (age) and types of breast milk the mother would be producing at that time. | Match each type of milk to the appropriate newborn day and with the size (e.g. marble ball) that best represented the newborn's stomach capacity. |
The instructions at each station contained a description of a scenario that required them to perform a skill (e.g. match items, demonstrate proper milk let down, select correct interventions, etc.). The clinical skills being assessed in the stations ranged anywhere from selecting appropriate interventions for breast conditions such as mastitis to using a breast pump correctly and showing proper removal. In four of the stations the students were required to match items, in two stations they needed to mark the correct interventions and procedures on a sheet of paper that offered multiple answer choices, in three stations the students required skill demonstrations (e.g. hand milk expression, proper attachment and detachment of breast pump, and proper removal of the infant from mothers breast), and lastly one station required that the students pull out appropriate intervention items out of a container which had extra items that were distractors. Dummies (women and newborn) were used for the stations to facilitate the students demonstration when was needed (e.g. removal of the newborn from the mother breast).
Ethical ConsiderationsThe University of Miami Institutional Review Board approved the study.
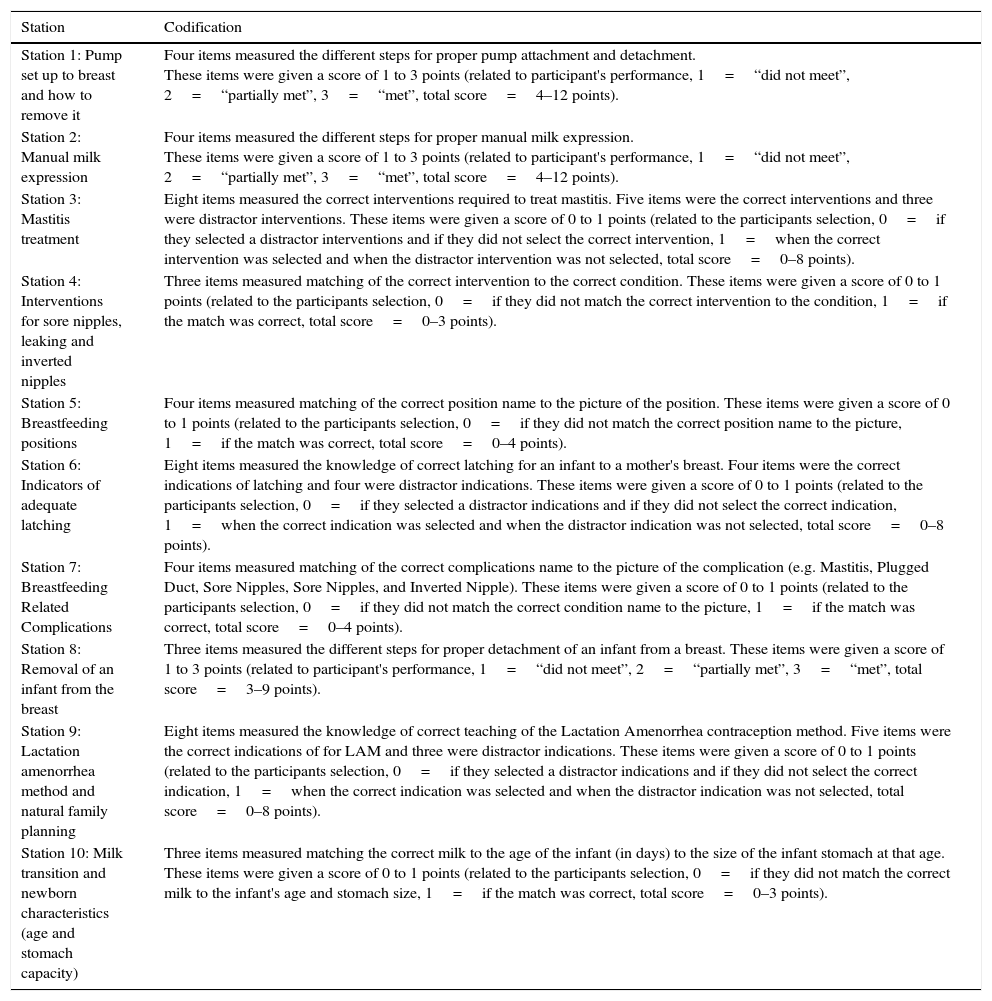
MeasuresBreastfeeding OSCE stations scoresAfter the checklists were completed, all of the observations were analyzed and codified using a standardized evaluation form which allowed for assessments to be consistent and objective when each student's performance was scored. A higher score represented higher levels of correct breastfeeding clinical skills (see Table 2).
Checklist codification measure.
| Station | Codification |
|---|---|
| Station 1: Pump set up to breast and how to remove it | Four items measured the different steps for proper pump attachment and detachment. These items were given a score of 1 to 3 points (related to participant's performance, 1=“did not meet”, 2=“partially met”, 3=“met”, total score=4–12 points). |
| Station 2: Manual milk expression | Four items measured the different steps for proper manual milk expression. These items were given a score of 1 to 3 points (related to participant's performance, 1=“did not meet”, 2=“partially met”, 3=“met”, total score=4–12 points). |
| Station 3: Mastitis treatment | Eight items measured the correct interventions required to treat mastitis. Five items were the correct interventions and three were distractor interventions. These items were given a score of 0 to 1 points (related to the participants selection, 0=if they selected a distractor interventions and if they did not select the correct intervention, 1=when the correct intervention was selected and when the distractor intervention was not selected, total score=0–8 points). |
| Station 4: Interventions for sore nipples, leaking and inverted nipples | Three items measured matching of the correct intervention to the correct condition. These items were given a score of 0 to 1 points (related to the participants selection, 0=if they did not match the correct intervention to the condition, 1=if the match was correct, total score=0–3 points). |
| Station 5: Breastfeeding positions | Four items measured matching of the correct position name to the picture of the position. These items were given a score of 0 to 1 points (related to the participants selection, 0=if they did not match the correct position name to the picture, 1=if the match was correct, total score=0–4 points). |
| Station 6: Indicators of adequate latching | Eight items measured the knowledge of correct latching for an infant to a mother's breast. Four items were the correct indications of latching and four were distractor indications. These items were given a score of 0 to 1 points (related to the participants selection, 0=if they selected a distractor indications and if they did not select the correct indication, 1=when the correct indication was selected and when the distractor indication was not selected, total score=0–8 points). |
| Station 7: Breastfeeding Related Complications | Four items measured matching of the correct complications name to the picture of the complication (e.g. Mastitis, Plugged Duct, Sore Nipples, Sore Nipples, and Inverted Nipple). These items were given a score of 0 to 1 points (related to the participants selection, 0=if they did not match the correct condition name to the picture, 1=if the match was correct, total score=0–4 points). |
| Station 8: Removal of an infant from the breast | Three items measured the different steps for proper detachment of an infant from a breast. These items were given a score of 1 to 3 points (related to participant's performance, 1=“did not meet”, 2=“partially met”, 3=“met”, total score=3–9 points). |
| Station 9: Lactation amenorrhea method and natural family planning | Eight items measured the knowledge of correct teaching of the Lactation Amenorrhea contraception method. Five items were the correct indications of for LAM and three were distractor indications. These items were given a score of 0 to 1 points (related to the participants selection, 0=if they selected a distractor indications and if they did not select the correct indication, 1=when the correct indication was selected and when the distractor indication was not selected, total score=0–8 points). |
| Station 10: Milk transition and newborn characteristics (age and stomach capacity) | Three items measured matching the correct milk to the age of the infant (in days) to the size of the infant stomach at that age. These items were given a score of 0 to 1 points (related to the participants selection, 0=if they did not match the correct milk to the infant's age and stomach size, 1=if the match was correct, total score=0–3 points). |
The evaluation of the training was done immediately after the students completed the OSCE using an online structured measure with an estimated length of 20min. Students answered nine items reporting how confident they felt after the training to perform breastfeeding skills. Examples of these items include the following: to discuss with a pregnant women why breastfeeding is important for babies and mothers; assist a mother in positioning and attaching her infant for feeding; help mothers and babies to have skin to skin contact immediately after birth; and assist mothers to start early with breastfeeding. These items had 3 answers choices with a score ranging from 1 to 3 points (related to participant's agreement with the statement, 1=“I am not able to”, 2=“I am partially able to”, 3=“I am totally able to”, total score=9–27 points). A higher score represented a higher confidence in breastfeeding clinical skills after they received the online BT.
In addition, students answered 3 questions reporting the: (a) overall rate of this course (one question with 3 answers options excellent/good/poor), (b) what they learned from this course that would be most useful in their work with pregnant women, new mothers, and newborn infants? (one open-ended question), and (c) their feedback about how the intervention could be improved (one open-ended question).
Statistical analysisThe Predictive Analytics Software (SPSS), version 18.0, was used for data analysis. Descriptive statistics were used to analyze the breastfeeding OSCE scores. Quantitative content analysis was used to analyze the questions about the students’ learning from this course that would be most useful in their work with pregnant women, new mothers, and newborn infants, and their feedback about how the OSCE could be improved.
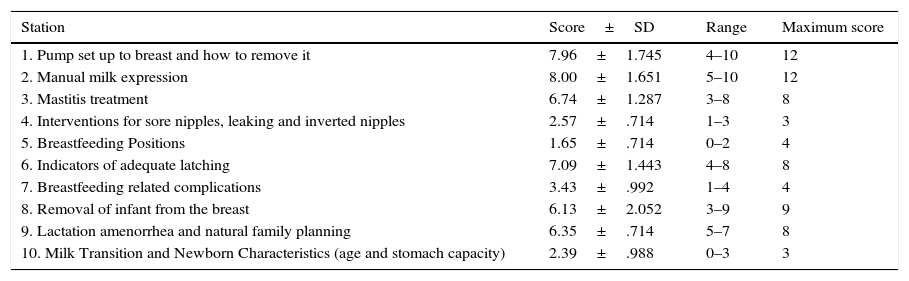
ResultsAfter the students completed the 10 breastfeeding OSCE stations, the observations were analyzed, codified, and the scores for each station were calculated (see Table 3). The stations with the highest score were: interventions for sore nipples, leaking and inverted nipples (station 4, M=2.57, SD=.843), indicators of adequate latching (station 6; M=7.09, SD=1.443), and breastfeeding complications (station 7; M=3.43, SD =.992). The stations where the students had the lowest scores were: pump set up to breast and how to remove it (station 1, M=7.96, SD=1.745), breastfeeding positions (station 5, M=1.65, SD=.714), and removal of infant from the breast (station 8, M=6.13, SD=2.052).
Breastfeeding OSCE scores (n=23).
| Station | Score±SD | Range | Maximum score |
|---|---|---|---|
| 1. Pump set up to breast and how to remove it | 7.96±1.745 | 4–10 | 12 |
| 2. Manual milk expression | 8.00±1.651 | 5–10 | 12 |
| 3. Mastitis treatment | 6.74±1.287 | 3–8 | 8 |
| 4. Interventions for sore nipples, leaking and inverted nipples | 2.57±.714 | 1–3 | 3 |
| 5. Breastfeeding Positions | 1.65±.714 | 0–2 | 4 |
| 6. Indicators of adequate latching | 7.09±1.443 | 4–8 | 8 |
| 7. Breastfeeding related complications | 3.43±.992 | 1–4 | 4 |
| 8. Removal of infant from the breast | 6.13±2.052 | 3–9 | 9 |
| 9. Lactation amenorrhea and natural family planning | 6.35±.714 | 5–7 | 8 |
| 10. Milk Transition and Newborn Characteristics (age and stomach capacity) | 2.39±.988 | 0–3 | 3 |
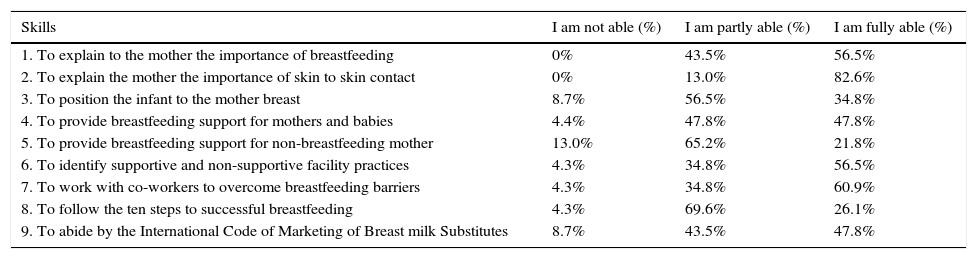
All the students completed the OSCE evaluation. The majority of the students felt that they were fully able or partly able to perform the nine clinical skills to support breastfeeding. The students reported the highest levels of confidence in their performance on the clinical skills needed helping mothers and babies have skin to skin contact immediately after birth (n=19, 82.6%); and work with coworkers to highlight barriers to breastfeeding and how to overcome those barriers (n=14, 60.9%). The students felt less confident with their ability to provide support for non-breastfeeding mothers (n=5, 21.8%), as well as following the ten steps to successful breastfeeding (n=6, 26.1%). Table 4 contains detailed information about the nine clinical skills to support breastfeeding that were assessed. All the students rated the OSCE as “excellent or good”.
Breastfeeding skills.
| Skills | I am not able (%) | I am partly able (%) | I am fully able (%) |
|---|---|---|---|
| 1. To explain to the mother the importance of breastfeeding | 0% | 43.5% | 56.5% |
| 2. To explain the mother the importance of skin to skin contact | 0% | 13.0% | 82.6% |
| 3. To position the infant to the mother breast | 8.7% | 56.5% | 34.8% |
| 4. To provide breastfeeding support for mothers and babies | 4.4% | 47.8% | 47.8% |
| 5. To provide breastfeeding support for non-breastfeeding mother | 13.0% | 65.2% | 21.8% |
| 6. To identify supportive and non-supportive facility practices | 4.3% | 34.8% | 56.5% |
| 7. To work with co-workers to overcome breastfeeding barriers | 4.3% | 34.8% | 60.9% |
| 8. To follow the ten steps to successful breastfeeding | 4.3% | 69.6% | 26.1% |
| 9. To abide by the International Code of Marketing of Breast milk Substitutes | 8.7% | 43.5% | 47.8% |
Note: N=80. The variation in the total % for skills 2 and 6 is due to missing data (1 student).
Two survey questions were presented to the students about the OSCE; one asking them what they learned and the other one asking for any suggestions to improve the OSCE. In regards to what they learned, twelve (27.91%) comments referred to learning the importance of breastfeeding and the benefits, seven (16.28%) comments referred to how the OSCE helped them learn breastfeeding techniques. For example, one student commented: “I learned the proper techniques to latching and unlatching a baby,…”. Six (13.95%) comments were about comfortably teaching and communicating with mothers in regards to breastfeeding. A student said: “I have learned to feel comfortable to speak with a mother concerning breastfeeding techniques…”. Five (11.63%) comments referred to the clinical skills that were acquired and can be used in the clinical setting. Lastly, two (4.65%) comments were made on learning how to support mothers and babies with difficulties.
In addition to comments about learning eleven (55%) comments addressed the OSCE methodology as a learning strategy, nine (20.93%) comments mentioned that it reinforced their previous knowledge, and two (4.65%) comments showed that the OSCE tested their knowledge and there were several suggestions from the students to improve the OSCE. Six (35.29%) comments were made suggesting more hands on practice either during the OSCE or in class. One student mentioned: “I would like there to be more hands on work to practice”, four (23.53%) comments showed the need for improve instructions clarity on some of the stations. Three (17.64%) comments were related to incorporating an immediate debriefing session after the OSCE. One student said: “I would maybe recommend a 20min after the station-training to discuss any questions or issues”, two (11.77%) comments suggested incorporating the OSCE stations as a permanent part of the maternity course and two (11.77%) comments indicated the need for educating students on available resources they can refer mothers to who may come across issue after discharge.
DiscussionIt is a consensus that breastfeeding provides major benefits for mothers and infants. Lactation and breastfeeding experts agree that healthcare professionals, especially nurses, have a major influence on a mother's decision to initiate and maintain breastfeeding.3,17,20,21 Nurses should be well-trained and equipped with the best evidence-based knowledge and skills techniques to promote, protect, and support breastfeeding mothers.13 The best evidence to date is the Ten Steps.4,22 To breastfeeding success, nurses should have the knowledge, attitude, and clinical skill in breastfeeding and lactation management to support mothers.18,23
One big obstacle to train nursing students in breastfeeding is that clinical sites do not provide sufficient opportunities to achieve the clinical skills needed to support breastfeeding.14,24,25 In this study, the OSCE showed to be a very good methodology to increase nursing student's clinical skills, allowing to avoid the challenges of busy clinical environments and client safety issues. This finding is congruent with other studies conducted with other healthcare providers.26–30 The OSCE experience in this study was enjoyed by the nursing students evidenced by their positive feedback, as a good learning, valuable and practical experience similar findings were reported in Awaisu et al.,31 Branch,32 and Pierre et al.33 studies.
The OSCE, in this study, provides a meaningful alternative strategy as it allows for individual assessments of a total group or class of students in a timely, controlled, and simulated environment. Consequently, students’ competence can be assessed in a non-threatening environment which minimizes risk and harm to an actual breastfeeding mother.17,34,35 Moreover, simulated environments supplement the need for clinical sites which are often hard to acquire for nursing students to practice breastfeeding skills.
The use of the OSCE, in this study, extends beyond students’ merely demonstrating skills, such as assisting women with position and infant feeding techniques; it involves students’ interactions to support breastfeeding women, communicate effectively, to respond to women's needs.17 In addition, in this study, students performed very well on identifying the indicators of proper latching, helping the breastfeeding mother when they have sore or leaking.36–39
There were some stations in this study in which students did not performed well. For example, they had problems setting up a breast pump or removing an infant from the breast. This may be in part due to the instructions not being clear enough or because some of the students may have experienced nervousness, stress, and/or anxiety. These emotional reactions were reported in other studies in which the OSCE was utilized. It will be interesting to study these emotional reactions to the OSCE to find strategies to minimize or to avoid them.29,33,39–42 In the future, to reinforce the learning in the stations where students underperformed, the following strategies may be incorporated: (a) more visual content (e.g. pictures, videos, games) in the training, (b) online videos demonstrating the proper technique after they complete the stations, (c) students can request appointments for more one-on-one demonstration, and (d) proper technique for all stations can be discussed and demonstrated for the whole class as a form of review after the OSCE.
LimitationsLimitations of this study include the limited sample size. Since this was the first time that the OSCE methodology was implemented and efforts were made to accommodate the maximum number of students based on the resources available. The methodology required the presence of several observers and additional personnel (e.g. timekeeper) which could jeopardize the replication of the OSCE in other settings where the personnel available is limited. Future studies can incorporate technology to reduce the burden of the personnel dedicated to the OSCE. In addition, the sample was collected from one location, which limits the generalizability of the results. Another limitation is the study's design which limits inferential analysis of the results to prove the benefit of the OSCE.
ConclusionThe OSCE is an excellent method for teaching and assess clinical skills in the area of breastfeeding including mother and infant. The OSCE has been positively evaluated for objectivity in student assessment and provides a ‘hands on’ approach to assessing clinical competence in situations where the ‘real world’ clinical environment is not feasible to develop breastfeeding clinical skills performance. Scores and student feedback suggested that the OSCE can be a valuable tool to be used in other courses of the nursing undergraduate and graduate curriculum and not only in this University but in others as well as for healthcare workers who would like to learn for continuing education purposes in order help out breastfeeding mothers at their workplace and/or within their community.
Future studies can consider the implementation of the OSCE with community leaders or women in the community. Community leaders and women in the community, can be trained about breastfeeding using the OSCE. Future implementation of the OSCE can include online teaching via programs such as Zoom or Skype where the instructor can meet online with the breastfeeding mothers or pregnant women. The incorporation of online activities can also facilitate the dissemination of the OSCE to other communities or states in the U.S. and outside the U.S.
ContributionNV: Study concept, design, data collection, analysis and interpretation of data, drafting and critical revision of the manuscript.
RC: Study concept, interpretation of data, and critical revision of the manuscript.
MF: Organization of the literature, background design and participated drafting the article.
SH: Study concept, data collection, revision of the manuscript.
SS, YA and CLJ: Literature review, data collection.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
FundingSchool of Nursing and Health Studies at the University of Miami, Coral Gables, Florida and the Center of Excellence for Health Disparities Research: El Centro, National Institute on Minority Health and Health Disparities grant 2P60MD002266.
Conflict of interest statementThe authors report no financial interests or potential conflicts of interest with grantors or other entities whose products or services are related to topics covered in this manuscript that could be construed as a conflict of interest.
Previous presentationsNone.
Support for this research was received from the Center of Excellence for Health Disparities Research: El Centro, National Center on Minority Health and Health Disparities grant P60MD002266.
Peer Review under the responsibility of Universidad Nacional Autónoma de México.