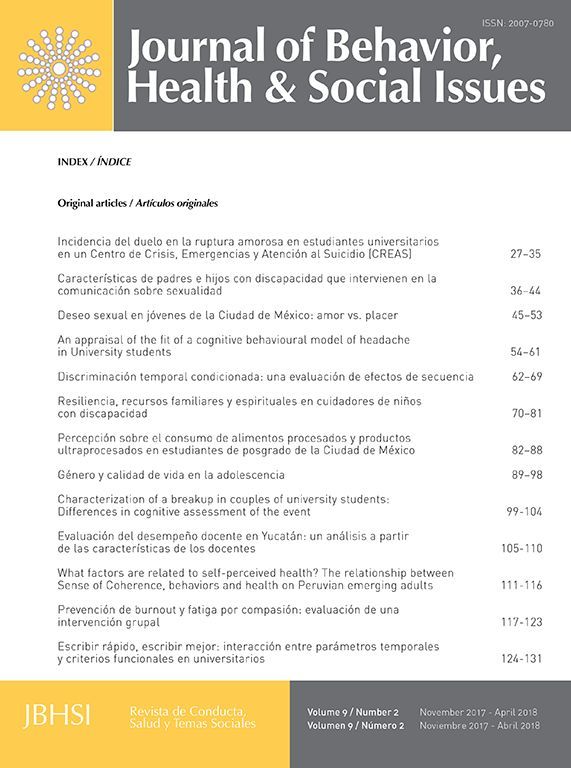
The aim of this study was to evaluate the fit of a cognitive behavioural model of headache in the population of University students, from Córdoba, Argentina. The direct and indirect contributions to pain intensity of control beliefs, beliefs and thoughts about pain and coping strategies were determined, as were the direct contributions of pain behaviours and disability. The sample was comprised of 382 students of both genders from several Universities. Multiple instruments were administered to measure the variables proposed in the cognitive behavioural model of headache followed by a descriptive and exploratory analysis of the data. Structural equation modelling was used and revealed an acceptable fit of the model but with lower levels than the criteria proposed. The model was therefore redefined by eliminating two indicators and was then found to achieve a better fit (CFI=.91; GFI=.95) and an optimal RMSEA index of .05. The new model explained 47% of the variance of headache intensity. All the variables of the model predicted pain intensity directly, with beliefs and thoughts about pain having the greatest predictive value (β=0.68).
El objetivo de este estudio fue el de evaluar el ajuste de un modelo cognitivo conductual de cefaleas en estudiantes universitarios de Córdoba, Argentina. Se examinaron las contribuciones directas e indirectas a la intensidad del dolor de las creencias de control, creencias y pensamientos sobre el dolor y las estrategias de afrontamiento, así como las contribuciones directas de las conductas del dolor y la discapacidad. La muestra estuvo compuesta por 382 estudiantes de ambos sexos de diferentes universidades. Se administraron múltiples instrumentos para medir las variables propuestas en el modelo cognitivo-conductual de cefalea, seguido de un análisis descriptivo y exploratorio de los datos. Los análisis mediante ecuaciones estructurales indicaron un ajuste aceptable del modelo, pero con niveles inferiores a los criterios propuestos. El modelo se redefinió eliminando 2 indicadores y se observó un mejor ajuste (CFI=.91; GFI=.95) y un índice RMSEA óptimo de .05. El nuevo modelo explicó el 47% de la varianza de la cefalea. Todas las variables del modelo predijeron la intensidad del dolor, siendo las creencias y los pensamientos sobre el dolor las de mayor valor predictivo (β=.68).
Task force on taxonomy of the International Association for the Study of Pain (IASP) says that pain is an unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage (Kumar & Elavarasi, 2016). Pain experience is a result of the interaction between sensory, behavioural and affective components; it can be caused by nociception, psychological factors and learning-based behavioural phenomena. It is one of the most common causes of disability and is associated with high levels of both economical costs as well as human suffering – particularly in cases of chronic pain. For these and other reasons the study of pain is a central topic of the contemporary health sciences (Miró, 2006).
Chronic pain is a type of pain which is present throughout long periods, is persistent, does not respond to common medical treatments and which does not have an adaptive value for the individual but instead is associated with a range of disorders which incapacitate the person (Miró, 2006). This pain causes the individual to face a continuous cascade of stressors which impact through all aspects of the person's life. Bearing in mind the complexity of chronic pain, it should be studied from a multidimensional perspective (van-der Hofstadt & Quiles, 2001).
Independently of the aetiology, pain is the main symptom which compels people to seek medical attention and is the principal reason for consulting within medical practices (Pueyrredón & Salvat, 2007). Within chronic pain the most frequent types include chronic lumbalgia, myofascial pain, fibromyalgia, neuropathic pain, phantom limb pain, central pain and headache (Bonica, 1990; Goldenberg, 1987; Pueyrredón & Salvat, 2007), with the last being the most common. Headache is defined as the sensation of pain or discomfort in the head and particularly the cranium (Rodríguez-Franco, Cano-García, & Blanco-Picabia, 2004).
In the city of Córdoba, Argentina, a study examining a range of lesser health disorders in University students was carried out which found that within the sample of 315 students 72.2% reported discomfort due to headaches. Given that headaches can potentially hinder academic performance and/or be symptomatic of a range of illnesses, and given the currently high prevalence of headache in the young adults sampled in this investigation, the need to study headache further and to benefit from explicative models of this complaint is evident (Moretti, 2010a).
Fear-avoidance modelOver the years some cognitive behavioural models have been developed in which the variables fear and avoidance are presented as crucial mechanisms to explain the progression of acute pain into chronic pain (Severeijns, Vlaeyen, van den Hout, & Picavet, 2004). In 1995, Vlaeyen, Kolen-Snijders, Boeren, and van Eek (1995) proposed a refined version of Lethem's cognitive behavioural model of chronic pain (Lethem, Slade, Troup, & Bentley, 1983). This model (see Fig. 1) states that after a pain-producing lesion appears, two different responses can be generated: in the first response the pain felt is interpreted as non-threatening and is faced in an adaptive way; the person does not catastrophise but confronts the pain experience and achieves an earlier recovery. The second possibility is that the pain experience is perceived as a threat whose consequences are catastrophised by the individual (Vlaeyen & Linton, 2000). When the latter occurs feelings of fear are linked to the pain experience (Leeuw et al., 2007). Catastrophisation – understood as an exaggerated negative orientation towards pain – leads to avoidance behaviours (e.g. avoiding movement) and hypervigilance of bodily sensations and is subsequently followed by disability, disuse and depression. Consequently, the pain experience is maintained, feeding into and reinforcing the vicious cycle and increasing the fear and avoidance responses (Vlaeyen & Linton, 2000). Catastrophisation therefore is established as a precursor to pain-related fear – more specifically to the fear of moving or gaining new lesions – and is affected by negative affectivity and by threatening information regarding the illness (Sullivan, Bishop, & Pivik, 1995). From the perspective of this model, pain-related fear or fear based in the belief that a new lesion will be caused explains why some individuals recover relatively quickly from pain while other develop chronic pain. It should be noted that in the case of people with chronic pain it is not possible to avoid the pain but it is possible to avoid that the pain be perceived as threatening (Leeuw et al., 2007).
Cognitive behavioural model of fear-avoidance in chronic pain (taken from Vlaeyen et al., 2007).
Despite the wide acceptance of the fear-avoidance model in the scientific community it also possesses some limitations. Firstly, Vlaeyen and Morley (2009) state that although the model has been successfully tested in cases of back and neck pain this has not occurred in cases of fibromyalgia or headache as there have only been a limited number of studies which apply the model to these conditions. Additionally, the model does not place importance on the intensity of pain despite various studies finding that intense pain is in itself an experience which produces fear and which leads to escape and avoidance. Finally, the model places fear of pain in a central position despite the existence of other factors which can determine the development of back pain, such as pain catastrophising and negative affect (see Fig. 1) (Leeuw et al., 2007).
Further to the above, this model only analyses coping mechanisms in terms of catastrophisation despite individuals possessing various ways in which they can face pain (Soriano & Monsalve, 2004). Furthermore, the conceptualisation of catastrophisation as a coping strategy has in itself been questioned given that it is also considered a cognition or negative thought (González-Rivera, Amador-Salinas, Fernández-López, & Tinajero-Estrada, 2011). Additionally, the only pain behaviour addressed in this model is avoidance despite other behaviours being possible, including verbal and non-verbal complaining, resting, etc. (Rodríguez-Franco, Cano-García, & Blanco-Picabia, 2000).
Finally, the above model does not address the role of cognitive and behavioural mediator and modulator variables which have been demonstrated to have strong predictive values of pain and the experience associated with it. Variables such as locus of control in pain, perceptions and beliefs about pain, negative thoughts regarding pain, pain behaviours, disability, self-efficacy in the control of pain and coping strategies possess a considerable weight in the determination of the pain experience (Anarte, Esteve, López, Ramírez, & Camacho, 2001; Camacho-Martel & Anarte-Ortiz, 2003; Vlaeyen & Linton, 2000; Rodríguez-Franco et al., 2000; Moix-Queraltó, 2005).
Cognitive behavioural model of headacheThe new cognitive behavioural model of pain in cases of headache proposed here (see Fig. 2) maintains that the variables control beliefs (which includes self-efficacy in the control of pain and locus of control in pain) and beliefs and thoughts about pain (which includes negative thoughts in response to pain and perceptions and beliefs about pain) are correlated (Cabanach, Valle, Rodríguez, Piñeiro, & González, 2015; Vinaccia et al., 2005). Additionally, both control beliefs and beliefs and thoughts about pain directly affect pain-related coping strategies (Cano-García & Rodríguez-Franco, 2002; Casey, Greenberg, Nicassio, Harpin, & Hubbard, 2008; González-Gutierrez et al., 2009) and indirectly affect pain behaviours (Anarte et al., 2001; Burns, Elfant, & Quartana, 2010; Camacho-Martel & Anarte-Ortiz, 2001; Cano-García, Rodríguez-Franco, García-Martínez, & Bellerín, 2005; González-Gutierrez et al., 2009; González-Ramírez & Landero-Hernández, 2010; González-Rivera et al., 2011; Nijs, van de Putte, Louckx, Truijen, & De Meirleir, 2008).
With respect to disability levels of students who suffer headache, control beliefs are indirectly related to these (mediated by the variable coping strategies) (Anarte et al., 2001; Rodríguez-Franco et al., 2004), while beliefs and thoughts about pain are directly related to them (Camacho-Martel & Anarte-Ortiz, 2003; Douglas, Graham, Anderson, & Rogerson, 2004; González-Gutierrez et al., 2009; Pérez-Pareja, Borrás, Sesé, & Palmer, 2005; Vranceanu, Barsky, & Ring, 2009). At the same time, both variables (control beliefs and beliefs and thoughts about pain) have a direct effect on the intensity of pain reported (Anarte et al., 2001; Cano-García & Rodríguez-Franco, 2002; Camacho-Martel & Anarte-Ortiz, 2003; Douglas et al., 2004; González-Gutierrez et al., 2009; González-Ramírez & Landero-Hernández, 2010; Moretti, 2010b).
Finally, the variables coping strategies, pain behaviours and disability directly affect the intensity of pain perceived by students with headache (Camacho-Martel & Anarte-Ortiz, 2003; Ferrando-García, 2009; Justo, Mañas, & Martínez 2010; Miró, 2006; Truyols-Taberner, Pérez-Pareja, Medinas-Amorós, Palmer-Pol, & Sesé Abad, 2008). Coping strategies also directly affect pain behaviours and disability as well as – together with disability – mediating the effects of control beliefs and beliefs and thoughts about pain on pain behaviours and pain intensity.
Purpose of present studyThe current work evaluates a new explicative model of pain in a population of University students with the aim to observe the direct and indirect contributions of different variables in the prediction of headache intensity (see Fig. 2). This new model is based on the model proposed by Vlaeyen (1995), but adding variables considered pertinent in the explanation and prediction of pain intensity such as pain behaviours, negative thoughts, self-efficacy, perceptions and beliefs about pain, locus of control, coping strategies and disability.
MethodParticipantsThe study sample consisted of 382 University students selected through a nonprobability judgemental sampling method. Before administering the tests each participant underwent a brief structured interview to evaluate their suitability for the study. An inclusion criterion employed was that participants should have experienced headache in the previous six months, regardless the type of headache, pain intensity and number of pain episodes. The sample size was sufficient to carry out the planned statistical analysis given that the literature (Coenders-Gallart, Batista-Foguet, & Saris, 2005) states that more than 5 participants per estimated parameter (of which this study includes 45) are needed.
The age range of the students in the sample was 18–49 years and the mean and standard deviation was 22.49 and 4.03 years respectively, with a higher proportion of females to males (77.7% and 22.3% respectively). 90% were students of state Universities and 10% were of private Universities. Of the 382 participants, 38% reported experiencing headaches once or twice per month, 26.7% several times per month, 17.2% several times per week, 16% a few times a year and 2.1% reported experiencing headaches on a daily basis.
With regards to pain intensity, 49% of the sample reported experiencing headaches of a predominantly moderate intensity and 38% a high intensity, the remaining 13% reported pain low intensity. When considering headache triggers 71.7% reported that triggers to their headache existed and 40.3% said that they could anticipate the onset of headache.
InstrumentsHeadache questionnaireAn ad hoc questionnaire which includes questions designed to determine whether the participant experiences headache as well as the duration and frequency of headache.
Socio-demographic and moderator variable questionnaireAn ad hoc questionnaire which includes socio-demographic questions (gender, age, University course) and other questions related to variables which could produce bias in the study; it asks whether the participant has a health condition and whether the participant consumes analgesic medication for relief of headache pain.
Pain behaviour questionnaireDeveloped by Philips and Hunter (1981; in Rodríguez-Franco et al., 2000), this examines behaviours shown by people who experience pain (“speak to several people about the pain”, “moan, cry, sigh”, “avoid contact with other people”). In the present study the locally adapted version of this questionnaire was used (Moretti, 2016), which has 10 items distributed in 2 subjacent factors: 1) non-verbal complaint and avoidance behaviours, and 2) verbal complaints – these factors possess acceptable (α=0.76) and optimal (α=0.85) levels of internal consistency respectively. Individuals respond to this questionnaire on a 5-point scale which ranges from “never” to “always”.
Headache specific locus of control scaleThis questionnaire was developed by Martin, Holroyd and Penzien (1990, in Cano-García, Blanco-Picabia, & Rodríguez-Franco, 2000), and translated into Spanish by Cano-García et al. (2000). For the present work the version adapted to the local context (Moretti, 2016) was used, which has 24 items distributed in three underlying factors: 1) external locus of control in medical professionals (α=0.86), which represents the belief that pain will be relieved by medical professionals; 2) internal locus of control (α=0.80), which refers to beliefs that pain can be modified by personal actions, and 3) aleatory external locus of control (α=0.78), which represents the belief that pain is caused by chance. The responses to the instrument are carried out on a 5-point scale which ranges from “strongly disagree” to “strongly agree”.
Pain self-efficacy questionnaireThis evaluates patients’ beliefs regarding their abilities to manage their pain in specific situations (“when they argue with somebody”, “when things do not turn out as planned”, “when there is a sudden stressful situation in their life”). For the current work, the locally adapted version (Moretti, 2016) was used, whose factorial analysis (following the elimination of 16 items due to multifactorial load and theoretical criteria) demonstrated theoretical coherence and suggested the existence of two subjacent factors: 1) stress and social pressure, and 2) pain triggering stimuli. These factors have optimal (α=0.96) and acceptable (α=0.79) levels of internal consistency respectively.
Pain beliefs and perceptions inventoryThis inventory was developed by Williams and Thorn (1989) to evaluate the beliefs and perceptions which people have regarding their pain (“I blame myself if I have pain”, “I don’t know enough about my pain”, “my pain is confusing to me”). For the present work the locally adapted version (Moretti, 2016) was used which has twelve items distributed across three factors: 1) pain as a mystery (α=0.79); 2) chronicity of pain (α=0.80), and 3) self-blame (α=0.83). The subjects respond on a scale of four points according to their level of agreement/disagreement with the statements presented to them.
Pain coping skills questionnaireThis instrument was created by Rosenstiel and Keefe (1983, in Rodríguez-Franco et al., 2004) and evaluates the coping skills used by people with chronic pain (“I see the pain as a challenge and don’t let it bother me”, “I do that things that I enjoy such as watch television or listen to the radio”, “the pain is terrible and I feel I’m never going to get better”). The responses to the questionnaire are based on the frequency with which people carry out a determined action when faced with pain, from “never” to “always”. For this work the locally adapted version (Moretti, 2016) was used which consists of 16 items distributed across three subjacent factors: 1) positive self-instructions and distancing from pain (α=0.84); 2) distracting activities (α=0.81), and 3) faith and praying (α=0.95).
Negative thoughts in response to pain inventoryThis instrument was developed to evaluate negative thoughts related to pain (“I will become disabled”, “I’m a burden to my family”, “I can’t control this pain”). Individuals respond to the questionnaire according to the frequency with which the thoughts in each item occur to them on a scale of five points which ranges from “never” to “always”. For the current work, the locally adapted version of this instrument was used (Moretti, 2016) which has twenty items distributed in four subjacent factors: 1) general negative thoughts and of disability (α=0.79), 2) social negative thoughts (α=0.81), 3) thoughts of self-blame (α=0.74), and 4) thoughts of loss of control (α=0.68).
Visual analogue scaleThis instrument measures the intensity of pain in headache as perceived by University students and consists of a 10 centimetre line which goes from 0 (no pain) to 10 (the worst pain imaginable) and along whose length the individual places a mark to represent the intensity of the pain perceived (Chapman & Syrjala, 2001).
ProcedureThe participants were selected from several different Universities in Argentina and varying University courses including Law, Psychology, Architecture, Nutrition, Medicine, Public Relations, Physical Education, Microbiology, amongst others. When selecting the sample and administering the questionnaires priority was placed on accessing classrooms where lectures are given to enable the inclusion of the greatest number of participants in the least time – there were few cases in which students absent from classes were included in the sample. The sample was made only of people who had experienced headache in the previous six months.
Structural equations modelling was used to analyse the relationships between the variables presented in the new cognitive behavioural model of headache (see Fig. 2); the AMOS 20 program was used for these analyses. Multiple indices were examined to determine model fit: (a) The chi-squared statistic (χ2); (b) the comparative fit index (CFI); (c) the Tucker–Lewis index (TLI); and (d) the root mean square error of approximation (RMSEA). To interpret these indices, we used the critical values previously recommended. Specifically, values >.90 and .95 for the CFI and TLI were considered benchmarks for acceptable and good fit, respectively; and RMSEA values of <.08 and .06 were benchmarks for acceptable and good fit, respectively
ResultsStructural equations modelling was performed following the steps proposed by Batista-Foguet and Coenders-Gallart (2000). Firstly, the cognitive behavioural model was specified in the program AMOS (Model 1; see Fig. 2). Second, the model was examined for over identification by examining the degrees of freedom, of which there were 145. Next, to estimate the parameters the maximum verisimilitude method was used as the sample presented with a normal distribution. As presented in Table 1, the model showed an acceptable fit but with values below the criteria proposed by Hu and Bentler (1998). Given these results and following an examination of the residual errors and modification indices it was decided the model should be respecified (Model 2). Indicators which did not correlate significantly with their corresponding factor were eliminated; the indicators “Faith and Praying” and “Internal Locus of Control” were eliminated from the factors “Coping Skills” and “Control Beliefs” respectively. Additionally, Control Beliefs was divided in two factors, “Self-efficacy in pain control” and “External Control Beliefs”. Finally, the errors of the indicators of the factor “Beliefs and Thoughts about Pain” were correlated and, given the modifications carried out, there was a considerable increase in the fit indices examined (see Table 1).
Given the observed levels of fit, Model 2 (the respecified model) was chosen for the interpretation of the estimated parameters. The standardised regression coefficients obtained are presented in Fig. 3. The model has considerable explicative value, explaining 47% of the variance in headache intensity.
The re-specified model contains modifications made with the aim to achieve a greater fit. Firstly, the variable “control beliefs” was divided into two representative variables: external control beliefs (which include aleatory external locus of control and external locus of control in medical professionals, with internal locus of control being eliminated) and self-efficacy in pain control (whose indicators are self-efficacy in stress and social pressure and self-efficacy in pain triggers). The latter variable correlates negatively with the variable beliefs and thoughts about pain (β=−0.72), external control beliefs (β=−0.29) and intensity of pain in headache (β=−0.42) and correlates positively with coping strategies (β=0.62). Coping strategies influence pain intensity indirectly via its relations with disability (β=−0.03) and pain behaviours (β=0.09). Additionally, the variable beliefs and thoughts about pain presents a negative correlation with coping strategies (β=−0.53) and positive correlations with intensity of pain in headache (β=0.68), disability (β=0.23) and external control beliefs (β=0.27). Beliefs and thoughts about pain are indirectly related to pain behaviours (β=0.12), pain intensity (β=0.13) and disability (β=0.13) via coping strategies.
Also of note are the correlations found between external control beliefs and coping strategies (β=−0.28) and external control beliefs and disability (β=0.16). Additionally, external control beliefs have a direct, positive relation with intensity of pain in headache (0.24) and with pain behaviours (β=0.30). Furthermore, the variable “coping strategies” negatively correlates with intensity of pain in headache (β=−0.26), disability (β=−0.28) and pain behaviours (β=−0.22). Finally, both disability (β=0.10) and pain behaviours (β=0.41) correlate positively with pain intensity in headache.
DiscussionThe aim of this study was to evaluate the fit of new explicative model of pain in a population of University students with the aim to observe the direct and indirect contributions of different variables in the prediction of headache intensity. The cognitive behavioural model of chronic pain proposed by Vlaeyen (1995; in Vlaeyen, Crombez, & Goubert, 2007) was used as a template to which new variables were incorporated with the aim to make it more comprehensive and explicative and to increase its power of prediction. A first model (Fig. 2) synthesising the results of previous works and proposing new relationships was created. This model was then modified in order that it achieve greater fit, following the measurement of the direct and indirect contributions of the proposed variables. The final, new cognitive behavioural model of headache (Fig. 3) includes the variables pain behaviours, self-efficacy in pain control, beliefs and thoughts about pain, coping strategies, external control beliefs and disability.
This cognitive behavioural model of headache is of considerable explicative value; the proportion of variance in headache intensity explained is 47%. Specific changes to the originally proposed model are that the indicators “faith and praying” and “internal locus of control” are eliminated due to their low predictive power in pain intensity in headache, demonstrating that the majority of University students – as observed in the study sample – do not use this type of coping strategy nor have this type of control belief. All the variables were found to possess a direct relationship with pain intensity, with beliefs and thoughts about pain having the greatest predictive value (β=0.68). The new theoretical model proposed includes various variables – and their relationships – which are not considered in other studies and for this reason sets a precedent for future investigations aiming to research this topic more deeply.
The importance of having a cognitive behavioural model of headache is evident given the high occurrence of this common disorder in clinical practice. Given that it is vital that psychological input in pain is based on an adequate understanding of the dynamics which exist between psychological, social, behavioural and physiological factors (Ruvalcaba-Palacios & Domínguez-Trejo, 2009), this model can contribute to the improvement of the processes of evaluation and intervention in headache as it aids the development of shorter evaluative protocols with greater discriminative power and it also allows the creation of shorter and more effective intervention protocols (Pérez-Pareja et al., 2005). This model demonstrates the way in which different variables in headache are related, as well as the grade of correlation and prediction of the intensity of pain. These relationships are fundamental to interventions aiming to address the variables which best predict pain intensity. For work in clinical settings, this model suggests that interventions addressing beliefs and thoughts about pain (with the aim to make them more adaptive), increasing self-efficacy in pain control and reducing external control beliefs, a reduction in pain intensity can be achieved. Additionally, by increasing self-efficacy in pain control a decrease in beliefs and thoughts about pain can be achieved, and vice versa. Increasing self-efficacy in pain control can also cause an increase in adaptive coping strategies, with the latter also resulting in a decrease in pain behaviours which, in turn, will reduce pain intensity.
To finalise, limitations to this study can be highlighted in terms of its methodology; nonprobability accidental sampling could have been used with the inclusion of equal numbers of participants from public and private Universities with no differentiation of whether the person has suffered headache in the previous six months. Future studies should consider this limitation with the aim to achieve greater sample representativeness, with the incorporation of participants who do not suffer headaches allowing for group comparisons between a study and control group. Additionally, it would be ideal that the number of female participants be equal to that of male participants – this would also allow for new research to be carried out to analyse whether a gender difference in pain intensity in chronic headache exists. Lastly, in the present study the inventory of negative thoughts regarding pain contains an indicator (“thoughts of loss of control”) with a level of internal consistency lower than the acceptable levels (α=0.68); future lines of research should consider this point and also use evaluative methods other than the self-administered questionnaire in measuring the variables to gain greater objectivity and response corroboration.
Peer review under the responsibility of Asociación Mexicana de Comportamiento y Salud.