The Public Health System of the Balearic Islands (IB-Salut) implemented between 2016 and 2019 the Chronic Patient Care Plan to properly manage complex chronicity and provide quality care attention. The goal of this study is assessing the use of healthcare services and their associated costs before and after the implementation of the programme.
MethodsDescriptive analyses of resources destined to complex and advanced chronic patients (CCP and ACP).
ResultsAfter entering the programme: the frequency of CCP admissions to acute hospitals reduced by 6.9%, the frequency of CCP visits to emergency departments reduced by 8.4%, while the frequency of ACP admitted to intermediate care hospitals increased. Both the frequencies of ACP admitted to acute hospitals and emergency visits decreased to 16.7% and to 27.3%, respectively. Total cost before and after the implementation of the programme was €60,884,241 and €46,889,693, respectively. Taking into account the 1011 admissions avoided, the result is a negative incremental cost-effectiveness ratio (€-396.57) per acute hospital admission that was avoided.
ConclusionThe Chronic Patient Care Plan might be interpreted as a cost-effective intervention. This first assessment would benefit from further research including control groups.
El Servicio de Salud de las Islas Baleares (IB-Salut) implementó entre 2016-2019 un Plan de Atención a Personas con Enfermedades Crónicas para gestionar la cronicidad compleja de manera eficiente y asegurar una atención sanitaria de calidad. El objetivo de este estudio es evaluar el uso de recursos sanitarios y los costes asociados, antes y después de la implementación del programa.
MétodoAnálisis descriptivo de recursos destinados a pacientes crónicos complejos y avanzados (PCC y PCA).
ResultadosLa frecuencia de PCC que ingresaron en hospitales de agudos y que visitaron las urgencias hospitalarias disminuyó un 6,9 y un 8,4%, respectivamente. Se observó un incremento de la frecuencia de PCA que ingresaron en los hospitales de atención intermedia. La frecuencia de PCA que ingresaron en hospitales de agudos y que visitaron urgencias se redujo un 16,7 y un 27,3%, respectivamente. El coste total antes de la implementación del programa fue de 60.884.241 € y después de 46.889.693 €. Al relacionarlo con los 1.011 ingresos evitados supone una ratio coste-efectividad incremental negativa (–396,57 €) por ingreso en hospital de agudos evitado.
ConclusiónEl Plan de Atención a Personas con Enfermedades Crónicas se interpreta como una intervención coste-efectiva si bien se considera necesario ampliar el análisis de datos incluyendo grupos de control.
About 5% of the adult population shows at least one chronic condition, which requires a large amount of resources.1,2 Some authors define this type of patients as “complex chronic patients” due to their medical management being complicated for healthcare providers.2 One percent of this adult population suffers from one, or more, advanced chronic condition.3
Being aware of the high-cost care of these patients, different countries and organisations are implementing organisational and management models focused on primary care with proactive actions and collaborative practices.4,5
The Public Health System of the Balearic Islands (IB-Salut) implemented between 2016 and 2019 the Chronic Patient Care Plan for complex chronic patients (CCP) and advanced chronic patients (ACP) to properly manage complex chronicity and provide quality care attention. This programme was designed as an organisational and care model based on primary healthcare services coordinated with other different care levels. Two of the main goals of the programme were to identify both complex and advanced chronic patients and reduce the number of hospital admissions and emergency visits.6,7
The lack of experience on this new way of providing care services at both medium and long term, along with the absence of conceptual evaluation frameworks, accounts for the few experiences of systematic assessment. The evaluation of care programmes for chronic patients presents a challenge in which professionals must deal with the assessment of heterogeneous and complex interventions. As the care of complex chronic patients is a high resource-consuming action, its sustainability requires promoting cost-effective programmes that impact the overall system.8
The goal of the study is to evaluate the use of health care services and their associated costs before and after the implementation of the programme. We expect to confirm the hypothesis that the implementation of the care programme for people with chronic conditions results in a reduction of both visits to the emergency departments and acute care hospitals admissions, along with an increase of the use of the community health services.
Research methodsDesignPre-post comparison of the use of resources and healthcare services in a group of CCP and ACP, from a year previous to admission in the programme (pre intervention measurement) to the end of the first year after admission (post intervention measurement). The programme began in 2016 and the quantitative assessment was carried out in 2019.
ScopeThe scope of the study was the Public Health System of the Balearic Islands (IB-Salut), which reaches to a population of approximately 1,060,964 inhabitants and covers seven health sectors. Each of these sectors has one acute referral hospital (AH) and, additionally, there are three intermediate care hospitals (ICH).
PopulationWe included in our study all CCP and ACP older than 18 years old that were registered in the analytic data system in November 2019. All individuals were part of the programme for at least 12 months.
InterventionThe intervention carried out within the framework of the programme, the effect of which is the object of the present study, consisted in:
- 1.
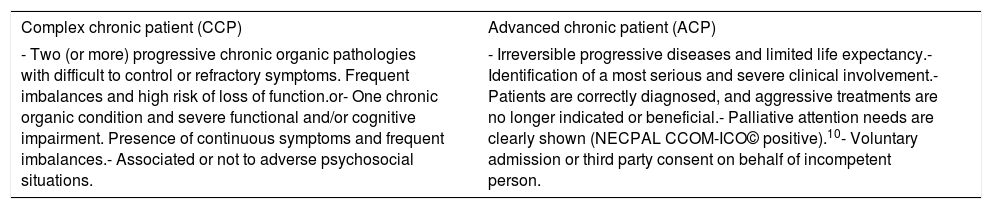
Identifying the population according to their complexity levels and developing a marking system in the medical record with CCP and ACP alerts. Once the referral professional activates the alerts, in accordance with their clinical judgement and the criteria defined in the programme (Table 1), these patients become noticeable in all levels of care. Then, a proactive, planned and individualised professional attention may be provided.
Table 1.Criteria for the identification of complex chronic patients and advanced chronic patients.
Complex chronic patient (CCP) Advanced chronic patient (ACP) - Two (or more) progressive chronic organic pathologies with difficult to control or refractory symptoms. Frequent imbalances and high risk of loss of function.or- One chronic organic condition and severe functional and/or cognitive impairment. Presence of continuous symptoms and frequent imbalances.- Associated or not to adverse psychosocial situations. - Irreversible progressive diseases and limited life expectancy.- Identification of a most serious and severe clinical involvement.- Patients are correctly diagnosed, and aggressive treatments are no longer indicated or beneficial.- Palliative attention needs are clearly shown (NECPAL CCOM-ICO© positive).10- Voluntary admission or third party consent on behalf of incompetent person. - 2.
Creating specific inpatient units for CCP in AH and specific routes of care in close coordination with these units through case management.
- 3.
Creating specific units in ICH so ACP may have instant access from their own home once they have been referred by their primary care professional. The professionals of these units, specially trained in palliative care, use an interdisciplinary perspective to provide a comprehensive approach so as to guarantee the maximum comfort and living standards.6
- 4.
Implementing the case management nursing programme in all health care areas with the main goal of guaranteeing the integral care plan, which is addressed to the patient, their family and their caregiver, through the coordination of different professionals and case managers, thus ensuring the continuity of healthcare services.9
Sociodemographic variables (age and gender) and the average duration in the programme have been considered. As far as the use of resources and services is concerned, the data from both CCP and ACP were recorded as follows:
- -
Acute hospitals (AH): percentage of admitted patients; percentage of patients who visited the emergency department; total number of admissions; total number of emergency visits; average of admissions; average of emergency visits; average duration of hospital admissions.
- -
Intermediate care hospitals (ICH): percentage of admitted patients; total number of admissions; average of admissions; average duration of hospital admissions.
- -
Primary care (PC): percentage of patients visited (total, at centre consultation and at domiciliary consultation) by general practitioner (GP) and nurse practitioner (NP); number of GP and NP visits (total, at centre and domiciliary); average of GP and nurse practitioner visits (total, at centre and domiciliary).
The costs associated with the use of resources in primary care and hospitals have also been considered.
Statistical analysisWe performed a descriptive analysis. Measures of central tendency and dispersion have been calculated (means and standard deviation) for continuous variables, while frequencies and percentages have been calculated for categorical variables. The comparison between qualitative variables was performed by applying Pearson's chi-squared test. The paired-sample's Student's t test was also calculated. The statistical analysis has been conducted using SPSS (Statistical Package for the Social Sciences) v. 17.0. The conversion from use of resources and services to costs was calculated using the public prices of the Public Health Network of the Balearic Islands as published in the Official Gazette of the Balearic Islands (Boletín Oficial de las Illes Balears, BOIB).11
Acute hospital admission costs were calculated as a total cost of 917€ (regulated cost) per day and patient during the length of hospital stay. Intermediate care hospital admission costs were calculated as a total cost of 230€ per day and patient during the length of stay in the health care facility. Furthermore, emergency admission cost is reported as 294€ per visit and patient. The cost of medical and nursing visits in healthcare facilities are reported as 33€ and 25€ per visit, respectively. Home-based medical and nursing care are reported as 46€ and 43€ per visit, respectively. Primary care consultations were considered as successive visits, since first visits and successive visits cannot be differentiated.
The incremental cost-effectiveness ratio (ICER) was calculated by dividing the difference of costs by the difference of income, both before and after the programme implementation.
ResultsA total of 8280 patients were included in the study (7910 CCP and 370 ACP). The average age was 80.74 (± 11.13) for CCP and 86.35 (± 10.67) for ACP. As far as gender is concerned, 60.3% of CCP and 68.9% of ACP were female. The average duration in the programme was 659.56 (± 193.40) days for the CCP, and 674.75 (± 228.77) days for the ACP.
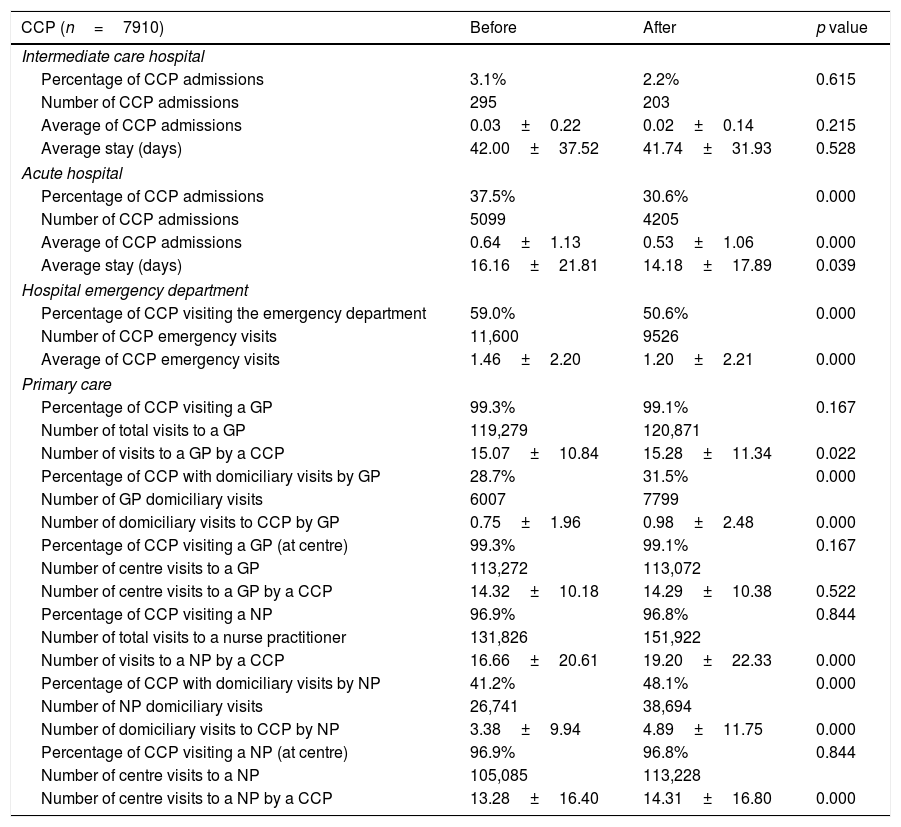
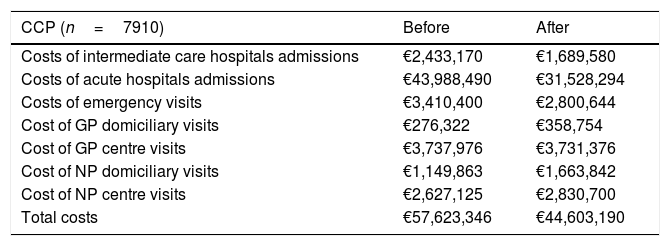
As for intermediate care hospitals, the frequency of CCP admissions was reduced by 0.9% while the total number of admissions dropped from 295 to 203. Regarding acute hospitals, the frequency of CCP admissions was reduced by 6.9% (p<0.001), while the number of admissions dropped from 5099 to 4205. Similarly, the frequency of CPP visits to emergency departments was reduced by 8.4% (p<0.001), while the number of visits dropped from 11,600 to 9526. Lastly, the use of medical consultations was similar to the data previous to entering the programme, as we did not find a significant increase in medical consultation per patient; however, nurse consultations did increase on average by 1.03 (p<0.001) (Table 2). As for the averages of CCP's annual admissions and visits, these were: 0.53 for acute hospital admissions, 1.20 for emergency visits and 34.48 for primary care visits. The cost of resources used by CCP dropped from €7284.87 to €5638.83 per year, representing a decrease from €19.95 to €15.44 daily per capita (Table 3).
Use of resources by CCP, 12 months before and after entering the programme.
| CCP (n=7910) | Before | After | p value |
|---|---|---|---|
| Intermediate care hospital | |||
| Percentage of CCP admissions | 3.1% | 2.2% | 0.615 |
| Number of CCP admissions | 295 | 203 | |
| Average of CCP admissions | 0.03±0.22 | 0.02±0.14 | 0.215 |
| Average stay (days) | 42.00±37.52 | 41.74±31.93 | 0.528 |
| Acute hospital | |||
| Percentage of CCP admissions | 37.5% | 30.6% | 0.000 |
| Number of CCP admissions | 5099 | 4205 | |
| Average of CCP admissions | 0.64±1.13 | 0.53±1.06 | 0.000 |
| Average stay (days) | 16.16±21.81 | 14.18±17.89 | 0.039 |
| Hospital emergency department | |||
| Percentage of CCP visiting the emergency department | 59.0% | 50.6% | 0.000 |
| Number of CCP emergency visits | 11,600 | 9526 | |
| Average of CCP emergency visits | 1.46±2.20 | 1.20±2.21 | 0.000 |
| Primary care | |||
| Percentage of CCP visiting a GP | 99.3% | 99.1% | 0.167 |
| Number of total visits to a GP | 119,279 | 120,871 | |
| Number of visits to a GP by a CCP | 15.07±10.84 | 15.28±11.34 | 0.022 |
| Percentage of CCP with domiciliary visits by GP | 28.7% | 31.5% | 0.000 |
| Number of GP domiciliary visits | 6007 | 7799 | |
| Number of domiciliary visits to CCP by GP | 0.75±1.96 | 0.98±2.48 | 0.000 |
| Percentage of CCP visiting a GP (at centre) | 99.3% | 99.1% | 0.167 |
| Number of centre visits to a GP | 113,272 | 113,072 | |
| Number of centre visits to a GP by a CCP | 14.32±10.18 | 14.29±10.38 | 0.522 |
| Percentage of CCP visiting a NP | 96.9% | 96.8% | 0.844 |
| Number of total visits to a nurse practitioner | 131,826 | 151,922 | |
| Number of visits to a NP by a CCP | 16.66±20.61 | 19.20±22.33 | 0.000 |
| Percentage of CCP with domiciliary visits by NP | 41.2% | 48.1% | 0.000 |
| Number of NP domiciliary visits | 26,741 | 38,694 | |
| Number of domiciliary visits to CCP by NP | 3.38±9.94 | 4.89±11.75 | 0.000 |
| Percentage of CCP visiting a NP (at centre) | 96.9% | 96.8% | 0.844 |
| Number of centre visits to a NP | 105,085 | 113,228 | |
| Number of centre visits to a NP by a CCP | 13.28±16.40 | 14.31±16.80 | 0.000 |
CCP, complex chronic patient; GP, general practitioner; NP, nurse practitioner.
Costs associated with the use of resources by CCP, 12 months before and after entering the programme.
| CCP (n=7910) | Before | After |
|---|---|---|
| Costs of intermediate care hospitals admissions | €2,433,170 | €1,689,580 |
| Costs of acute hospitals admissions | €43,988,490 | €31,528,294 |
| Costs of emergency visits | €3,410,400 | €2,800,644 |
| Cost of GP domiciliary visits | €276,322 | €358,754 |
| Cost of GP centre visits | €3,737,976 | €3,731,376 |
| Cost of NP domiciliary visits | €1,149,863 | €1,663,842 |
| Cost of NP centre visits | €2,627,125 | €2,830,700 |
| Total costs | €57,623,346 | €44,603,190 |
CCP, complex chronic patient; GP, general practitioner; NP, nurse practitioner.
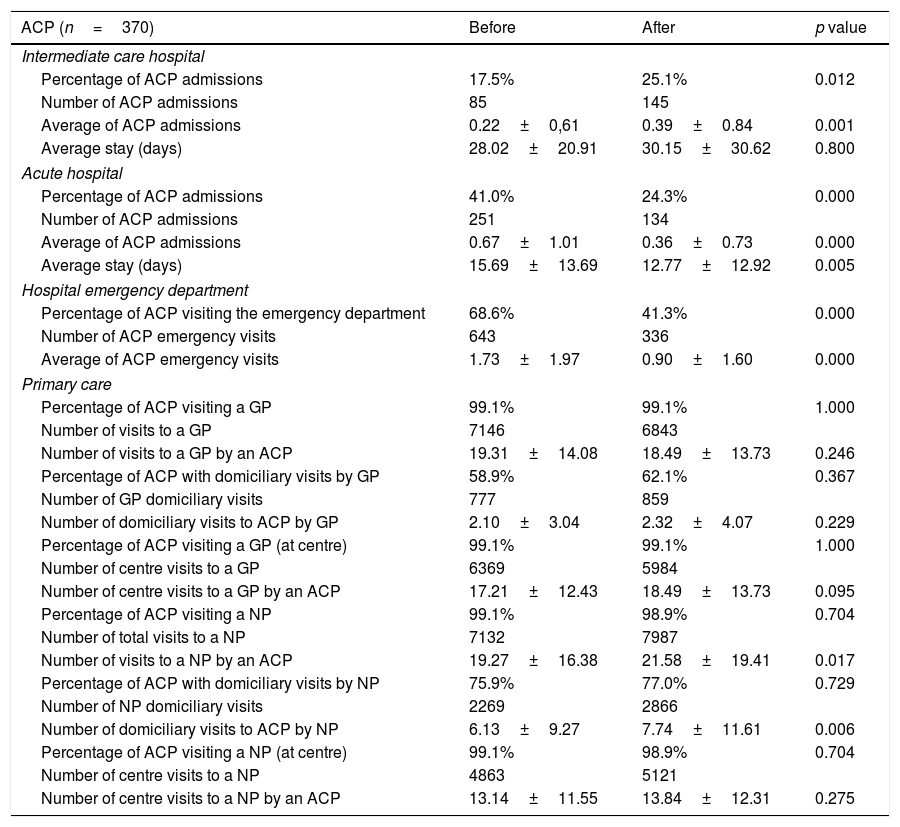
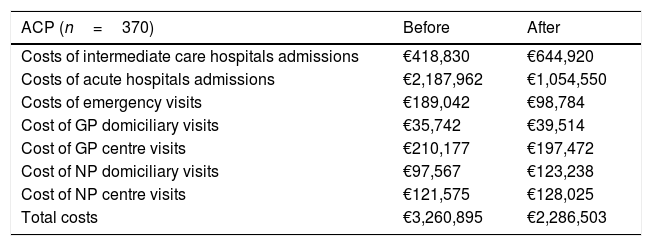
After entering the programme, the frequency of ACP admitted to intermediate care hospitals increased. On the other hand, both the frequencies of ACP admitted to acute hospitals and emergency visits decreased to 16.7% (p<0.001) and to 27.3% (p<0.001), respectively, while the number of hospital admissions and emergency visits decreased from 251 to 134, and from 643 to 336, respectively. The frequency of ACP visiting the nurse practitioner (total and domiciliary consultation) also increased after entering the programme (Table 4). Likewise, the average of annual emergency visits and admissions to acute hospitals was 0.90 and 0.36, respectively. Also, the average of annual visits to primary care was 40.08, that is, approximately, once every nine days. Furthermore, the costs associated with the use of resources by ACP fell from €8813.22 to €6179.73 yearly, which represents a daily cost reduction from €22.14 to €16.93 per capita (Table 5).
Use of resources by ACP, 12 months before and after entering the programme.
| ACP (n=370) | Before | After | p value |
|---|---|---|---|
| Intermediate care hospital | |||
| Percentage of ACP admissions | 17.5% | 25.1% | 0.012 |
| Number of ACP admissions | 85 | 145 | |
| Average of ACP admissions | 0.22±0,61 | 0.39±0.84 | 0.001 |
| Average stay (days) | 28.02±20.91 | 30.15±30.62 | 0.800 |
| Acute hospital | |||
| Percentage of ACP admissions | 41.0% | 24.3% | 0.000 |
| Number of ACP admissions | 251 | 134 | |
| Average of ACP admissions | 0.67±1.01 | 0.36±0.73 | 0.000 |
| Average stay (days) | 15.69±13.69 | 12.77±12.92 | 0.005 |
| Hospital emergency department | |||
| Percentage of ACP visiting the emergency department | 68.6% | 41.3% | 0.000 |
| Number of ACP emergency visits | 643 | 336 | |
| Average of ACP emergency visits | 1.73±1.97 | 0.90±1.60 | 0.000 |
| Primary care | |||
| Percentage of ACP visiting a GP | 99.1% | 99.1% | 1.000 |
| Number of visits to a GP | 7146 | 6843 | |
| Number of visits to a GP by an ACP | 19.31±14.08 | 18.49±13.73 | 0.246 |
| Percentage of ACP with domiciliary visits by GP | 58.9% | 62.1% | 0.367 |
| Number of GP domiciliary visits | 777 | 859 | |
| Number of domiciliary visits to ACP by GP | 2.10±3.04 | 2.32±4.07 | 0.229 |
| Percentage of ACP visiting a GP (at centre) | 99.1% | 99.1% | 1.000 |
| Number of centre visits to a GP | 6369 | 5984 | |
| Number of centre visits to a GP by an ACP | 17.21±12.43 | 18.49±13.73 | 0.095 |
| Percentage of ACP visiting a NP | 99.1% | 98.9% | 0.704 |
| Number of total visits to a NP | 7132 | 7987 | |
| Number of visits to a NP by an ACP | 19.27±16.38 | 21.58±19.41 | 0.017 |
| Percentage of ACP with domiciliary visits by NP | 75.9% | 77.0% | 0.729 |
| Number of NP domiciliary visits | 2269 | 2866 | |
| Number of domiciliary visits to ACP by NP | 6.13±9.27 | 7.74±11.61 | 0.006 |
| Percentage of ACP visiting a NP (at centre) | 99.1% | 98.9% | 0.704 |
| Number of centre visits to a NP | 4863 | 5121 | |
| Number of centre visits to a NP by an ACP | 13.14±11.55 | 13.84±12.31 | 0.275 |
ACP, advanced chronic patient; GP, general practitioner; NP, nurse practitioner.
Costs associated with the use of resources by ACP, 12 months before and after entering the programme.
| ACP (n=370) | Before | After |
|---|---|---|
| Costs of intermediate care hospitals admissions | €418,830 | €644,920 |
| Costs of acute hospitals admissions | €2,187,962 | €1,054,550 |
| Costs of emergency visits | €189,042 | €98,784 |
| Cost of GP domiciliary visits | €35,742 | €39,514 |
| Cost of GP centre visits | €210,177 | €197,472 |
| Cost of NP domiciliary visits | €97,567 | €123,238 |
| Cost of NP centre visits | €121,575 | €128,025 |
| Total costs | €3,260,895 | €2,286,503 |
ACP, advanced chronic patient; GP, general practitioner; NP nurse practitioner.
Total costs before and after the implementation of the programme was €60,884,241 and €46,889,693, respectively, thus saving a total of €13,994,548. If we do not consider the income-related savings in the statistical treatment, the total result is €400,940. Taking into account the 1011 admissions avoided, the result is a negative incremental cost-effectiveness ratio (ICER=€−396.57) per acute hospital admission that was avoided.
DiscussionThe main goal of the present study was to evaluate the use of health services and their related costs before and after the implementation of the Chronic Patient Care Plan in the Balearic Islands. The results so far show a significant reduction in hospitalisations and emergency visits for both CCP and ACP. On the other hand, the number of visits to the GP and NP in primary care increased. These results concur with other studies carried out on similar programmes of chronic care,12–14 and also follow the recommendations of the Spanish National Strategic Framework for Chronic Conditions15 about the promotion of primary care attention as a reference for patients with chronic conditions. The use of resources and the associated costs decreased in both cases after the identification of patients. According to these preliminary results, the implementation of the Chronic Patient Care Plan might be interpreted as a cost-effective intervention. Anyhow more research is needed using control groups.
The change in the expenditure distribution is quite interesting, as the costs associated with both emergency visits and acute hospital admissions decreased for both types of patients, while those associated with intermediate attention decreased for CCP but increased for ACP. As for the expense of primary care, this increased after the patients entering the programme. These results are in line with those of Blay et al., 16 who previously studied a community cohort of individuals with advanced chronic conditions, suggesting a better cost-effective approach while providing appropriate care.
The results of Allepuz et al.14 over a CCP sample after the implementation of a similar programme show the same pattern in the distribution of costs, which resulted in savings in hospital costs while primary care costs increased.
The frequency of healthcare resources used among ACP in the Balearic Islands was lower compared to other cases. Also, as far as the ACP are concerned, the annual visits to the emergency department as well as the intermediate care hospitals admissions were about half of those observed by Bullich et al.,17 who studied the data of morbidity and health services use in Catalonia. The annual visits made by primary care professionals are similar to those found by Blay et al.16 and almost double than those reported by Bullich et al.17 The cost associated with the use of resources per capita for ACP was also lower than those observed by Bullich et al.17 and Blay et al.16 (€16.93 daily vs. €20.14 and €19.4).
Nevertheless, it must be clarified that the lower costs that have been pointed out could be explained by the non-inclusion of neither the pharmacy expenses nor the cost of the external consultations in our study. Currently, these data are not available in our analytic data system.
Since beginning this programme, the number of interventions in primary care has increased. This may be due to the identification of patients with greater complexity, which the nurse case managers specially promoted by means of proactive recruitment, along with the increased number of health assessments and individualised plans devised, in a first step, by primary care. These two reasons, along with a better coordination between different care levels and the insurance of the continuity of care provided, may have contributed to the redistribution of the use of resources identified.
Concerning the limitations of our study, we need to point out again the lack of control groups, thus hindering the establishment of a correlation between the intervention and the reduction in the use of resources. Also, we assumed the same pattern of admissions for before and after entering the programme. Lastly, given the specific nature of the public prices,11 the risks of bias in the calculation of costs should be taken into account.
As most of the chronic care plans stress out,18 primary care should be the main axis of chronic patients care. Paradoxically enough, the total budget allocated to primary care level is stuck lower than 15% in relation to the total healthcare expenditure, while the annual growth is always lower than those of the hospitals.19 The results shown in our study reflect not only the key role that primary care plays in the attention of chronic patients but also a more efficient redistribution of healthcare resources.
Nowadays, primary healthcare is being the object of a transformation by national policies. This scenario poses a great opportunity to redesign, from this very primary level, the attention to patients with chronic conditions or palliative care needs, and thus, provide a much better service according to their needs, values and expectations.
This study represents a first approach to a quantitative model for the assessment of the chronicity care programme in the Balearic Islands. In this regard, the exploration and study of other variables concerning the integrated attention and the perceived quality of care would be of special interest.
Further development of the model is needed in parallel with an evaluation system that should allow the identification of more valuable strategies and of those patients who might benefit the most.
FundingThis research has received no funding from any public agencies, private companies or nonprofit organizations.
Conflict of interestsThe authors have no competing interests to declare.
The Technical Cabinet of the Public Health System of the Balearic Islands collaborated in the exploitation of data.