Risk management and patient safety are closely related, following this premise some industries have adopted measures to omit number 13. Healthcare is not left behind, in some hospital the day of surgery's or bed numbering avoid number 13. The objective was to assess whether it is necessary to redesign the safety policies implemented in hospitals based on avoiding 13 in the numbering of rooms/beds.
MethodsA retrospective cohort study was conducted. Mortality and the number of adverse events suffered by patients admitted to rooms/beds numbering 13 (bad chance) or 7 (fair chance) over a two-year period to Intensive Care Unit, Medicine, Gastroenterology, Surgery, and Paediatric service were registered and compared.
ResultsA total of 8553 admissions were included. They had similar length-of-stay and Charlson Index scores (p-value=0.435). Mortality of bed 13 was 268 (6.2%, 95% CI 5.5–6.9) and 282 in bed 7 (6.7%, 95% CI 5.9–7.5) (p-value=0.3). A total of 422 adverse events from 4342 admissions (9.7%, 95% CI 8.9–10.6) occurred in bed 13, while in bed 7 the count of adverse events was 398 in 4211 admissions (9.4%, 95% CI 8.6–10.4) (p-value=0.6). Odds Ratio for mortality was equal to 0.9 (95% CI 0.8–1.1) and suffering adverse events when admitted to bed 13 versus bed 7 was 1.03 (95% CI 0.9–1.2).
ConclusionsBed 13 is not a risk factor for patient safety. Hospitals should pay attention to causes and interventions to avoid adverse events based on evidence rather than beliefs or myths.
La gestión de riesgos y la seguridad del paciente están estrechamente relacionadas, siguiendo esta premisa, algunas industrias han adoptado medidas para omitir el número 13. La atención médica no se queda atrás, en algunas cirugías o la numeración de camas, evitan el número 13. El objetivo fue evaluar si es necesario rediseñar las políticas de seguridad implementadas en los hospitales para evitar el 13 en la numeración de habitaciones/camas.
MétodoEstudio de cohortes retrospectivo. La mortalidad y el número de eventos adversos de pacientes ingresados en las camas 13 (mala suerte) o 7 (buena suerte) fueron registrados y comparados.
ResultadosSe incluyeron 8.553 admisiones. El índice de Charlson fue similar en ambos grupos (p=0,435). Doscientos sesenta y ocho (6,2%, IC del 95%: 5,5-6,9) ingresos en cama 13 fallecieron a diferencia de 282 en cama 7 (6,7%, IC del 95%: 5,9-7,5) (p=0,3). Se produjeron 422 eventos adversos en 4.342 admisiones (9,7%, IC del 95% 8,9-10,6) en cama la 13 a diferencia de 398 eventos adversos en 4.211 admisiones (9,4%, IC del 95%: 8,6-10,4) en cama 7 (p=0,6). La odds ratio para la mortalidad de 0,9 (IC del 95%: 0,8-1,1) y para evento adverso de 1,03 (IC del 95%: 0,9-1,2).
ConclusionesLa cama 13 no es un factor de riesgo para la seguridad de los pacientes. Los hospitales deben prestar atención a las causas e intervenciones para evitar eventos adversos basados en la evidencia y no en creencias o mitos.
There is little doubt that safe practices prevent safety incidents. The impact of hand hygiene, the correct identification of patients, Bacteremia Zero or safe surgery has been established and they reduce the number of adverse events (AEs). However, although there have been crucial advances in patient safety, there is still a long way to go and AEs are still ‘easy to count, complicated to understand, and complex to prevent’.1 There are no simple recipes but applying what we know works and stopping what doesn’t work remains the best way for achieve optimal quality of care.
In spite of all this, we find in different countries and in different hospitals curious and sometimes probably counterproductive measures. For example, avoiding be admitted to hospital, nor undergo surgery,2 on Friday the 13th, or omitting 13 in the numbering of wards (and beds).3 This is because in our cultural environment, travelling, getting married or making a financial decision on the 13th is expected to go wrong.
The number 13, as a risk factor, has an uncertain origin related, in the Christian era, with the number of diners at the Last Supper and on the date chosen, by King Philip IV of France, to end the Order of the Knights Templar.4 Avoiding the number 13 is framed within risk management and are part of the decisions that are taken daily to avoid bad results (illusion of control),5 such as avoiding crossing the path of a black cat or walking under a ladder. These decisions have an indispensable adaptive component so that things do not go wrong,6 and do not require having their effect checked in the first person to consider them plausible.7 However, its potential positive effect has not been adequately investigated in the context of safe practices, unlike the risk factors associated with mortality,8 complications,9 readmission,10 or AEs.11
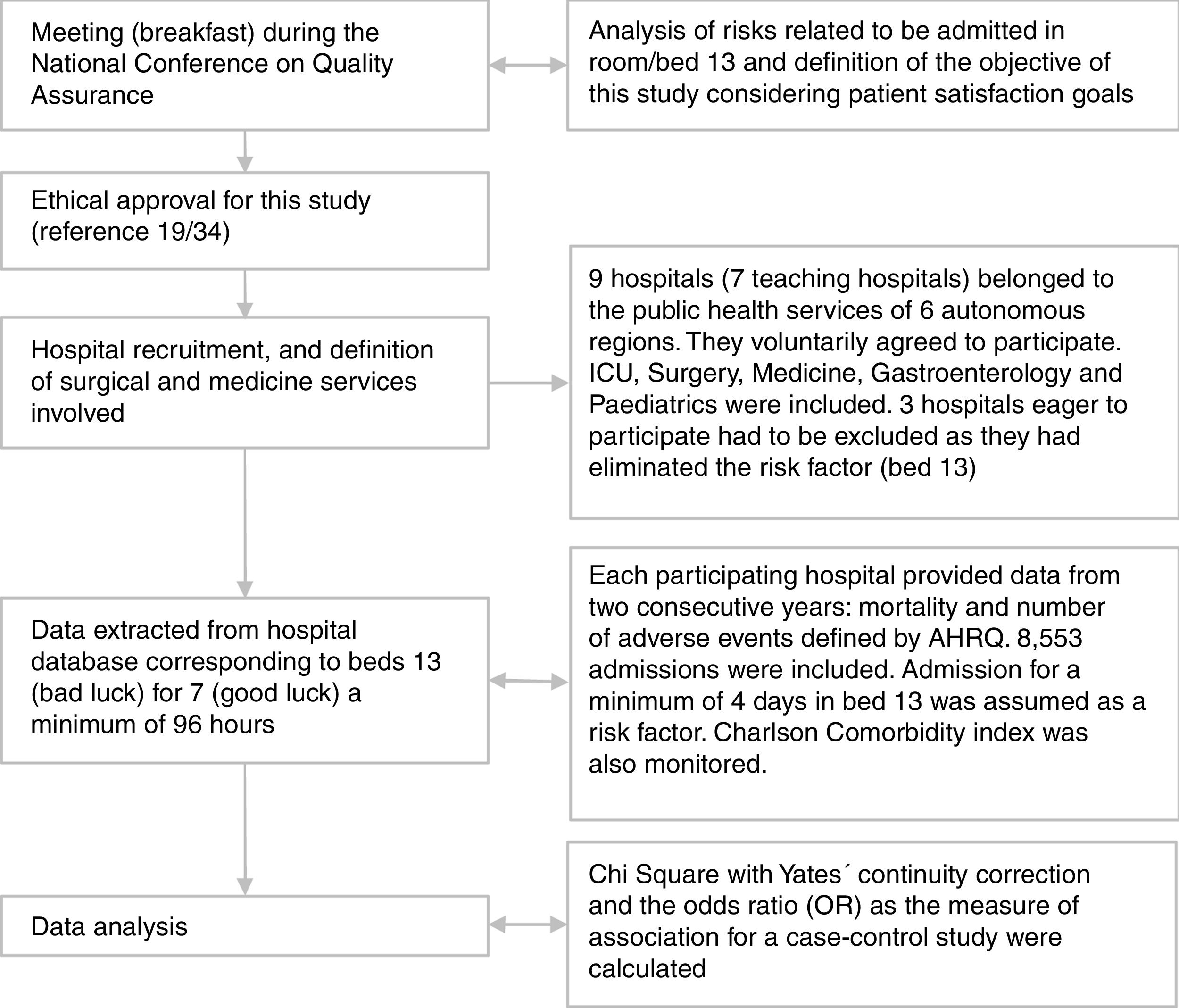
During the celebration of the annual Conference of the Spanish Society for Quality in Healthcare, in 2018, a group of patient safety directors from different Spanish regional health services debated on the evidence around other potential risk factors such as those derived from the bad luck of the patients when admitted to room/bed 13. They found out that some centres had already implemented preventive actions by eliminating beds with number 13, as part of their risk management programme in patient safety. The participants agreed on the importance of analysing this risk factor in the light of hospital safety policies to establish the most appropriate measures in the safety plans of the centres.
In this study, mortality and the number of patient safety incidents due to admission in bed 13 were analysed in a set of hospitals of the Spanish public Health Service in order to assess whether it was necessary to redesign the safety policies implemented.
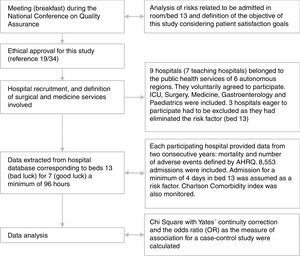
Material and methodsA retrospective cohort study was conducted on nine Spanish public hospitals. Each participating hospital provided data from two consecutive years of activity comprising the 2016–2018 period (all 2017 and 2018, except for two hospitals for years 2016 and 2017).
This study was conducted according to the ethical guidelines and the Spanish rules concerning the implementation of epidemiological and biomedical research. Ethical approval for this study (reference 19/34) was provided by the Research Ethics Committee of the Sant Joan d’Alacant Hospital, Sant Joan d’Alacant, on 27 March 2019.
Inclusion criteriaCases were defined as those patients admitted to any of the beds of the rooms identified with the number 13 and usually letters A and B. Patients admitted to rooms that corresponded to number 7 were included as control group, regardless of which floor they were on, for example beds numbered 213, 313, 413 or 207, 307 or 407.
Rooms 7 were chosen considering that our Western culture has a popular consensus that the number 7 is associated with good luck, basing its effectiveness on its coincidence with the colour spectrum of the rainbow, the days of the week, the estimated lives of a cat, or the human capacity for processing information.12
Data were extracted from the hospital database by qualified personnel for both beds in each of rooms 13 and 7. Databases include annual unweighted hospitalisations of patients covered by each hospital within the Spanish National Health System (Fig. 1).
STROBE criteria for observational studies was considered during this study's design and planning to strengthen the reporting and analytics.13
Participating hospitalsThe participating hospitals belonged to the public health services of six regions: Andalusia, Aragon, Valencia, Madrid, Murcia and Navarre. Seven were classified as teaching-hospitals; they had between 330 and 1166 beds. The hospitals were included on the basis that they had beds numbered 13 and their willingness to share the relevance and objectives of this study.
Study populationPatients were assigned to beds 13 and 7 by each center's Hospital Admission service. The assignment only considers the gender of the patient who is occupying a room bed and follows a random pattern. All patients recorded in the hospital database admitted to beds 13 for 7 a minimum of 96h and requiring the services of the ICU, Surgery, Medicine, Gastroenterology or Paediatrics were included. These services were chosen by consensus considering services with high and low incidence of AEs. No patient profile was excluded because of their beliefs about bad or good luck.
Admission for a minimum of 4 days in bed 13 was assumed as a risk factor, and when this risk factor was maintained throughout the admission regardless of whether another bed was occupied during the whole admission period.
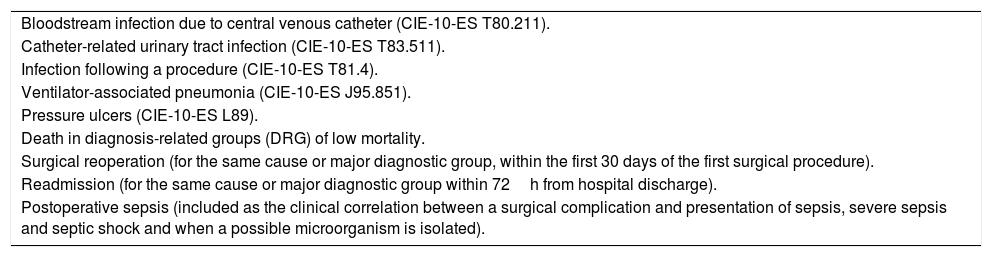
Study variablesThrough a consensus conference among experts, mortality (as in other studies) and a set of patient safety indicators were identified as dependent variables, based on safety metrics proposed by the Agency for Healthcare Research and Quality (AHRQ).14Table 1 shows the number of AEs included.
Adverse events included.a
| Bloodstream infection due to central venous catheter (CIE-10-ES T80.211). |
| Catheter-related urinary tract infection (CIE-10-ES T83.511). |
| Infection following a procedure (CIE-10-ES T81.4). |
| Ventilator-associated pneumonia (CIE-10-ES J95.851). |
| Pressure ulcers (CIE-10-ES L89). |
| Death in diagnosis-related groups (DRG) of low mortality. |
| Surgical reoperation (for the same cause or major diagnostic group, within the first 30 days of the first surgical procedure). |
| Readmission (for the same cause or major diagnostic group within 72h from hospital discharge). |
| Postoperative sepsis (included as the clinical correlation between a surgical complication and presentation of sepsis, severe sepsis and septic shock and when a possible microorganism is isolated). |
Agency for Healthcare Research and Quality. Quality Indicator Empirical Methods. November 2014. Available at: https://www.qualityindicators.ahrq.gov/Modules/psi_resources.aspx [accessed 2019/01/15]. CIE-10-ES is the Spanish version of the International Statistical Classification of Diseases and Related Health Problems (ICD-10).
The number of beds in each service, the number of days of stay (number of days of patient admission) and the Charlson Comorbidity index were also monitored controlling potential biases in the patient admission to beds numbered 13 or 7.
Statistical analysisWe compared, first, the Charlson Index of patients admitted to bed 13 and bed 7 of five participating hospitals, to control its potential effect and establish whether this variable should be considered a confounding factor.
For each service, the total sum of deaths and AEs for beds 13 and 7 were calculated as the simple sum of events. The differences in the incidence of mortality and AEs between beds 13 and 7 were analysed by the Fisher's exact test. We calculated the odds ratio (OR) as the measure of association for relative risk.
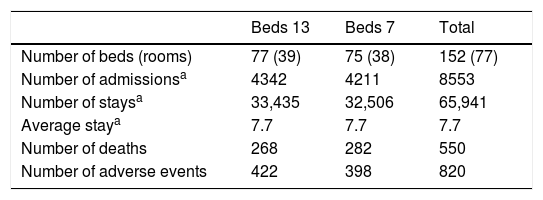
ResultsThe nine hospitals that contributed data had a total of 340,309 admissions in all the medical services and performed 117,251 admission surgical procedures.
Sample characteristicsThere were a total of 8553 admissions in all of the hospital services included in this study that resulted in 65,941 stays, with a total of 567 rooms and 1134 beds (142 in ICU, 287 in Surgery, 414 in Medicine, 184 in Gastroenterology and 107 in Paediatrics (Table 2). One hospital only had 12 rooms in the ICU. Unfortunately, three other hospitals that were eager to participate were excluded from the study because they had eliminated the risk factor and did not have beds numbered 13 in their medical or surgical services.
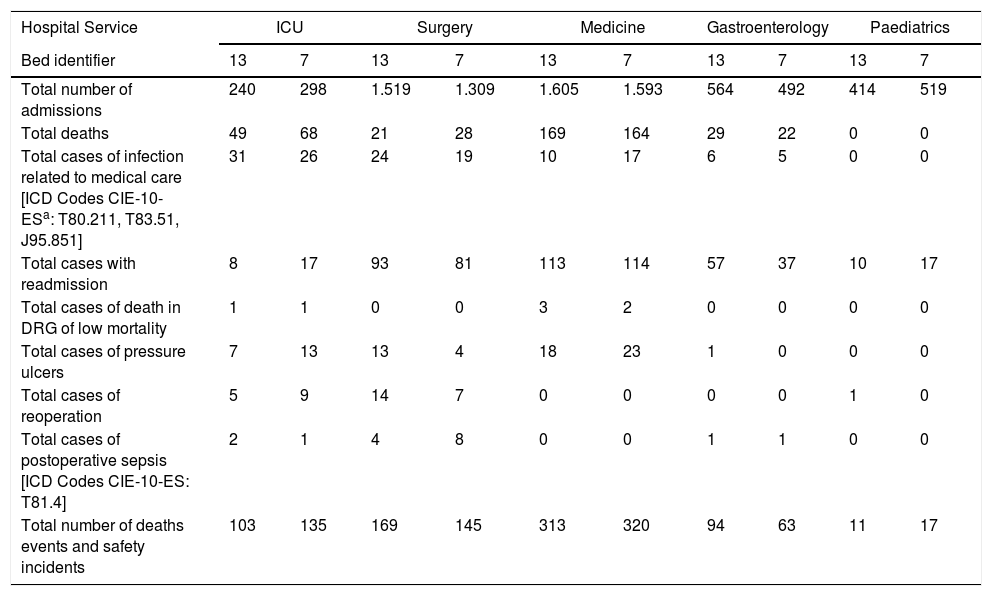
Total number of admissions, stays, deaths and adverse events occurring over a two-year period in bed 13 and 7.
The average length-of-stay in both beds 13 to 7 was identical over the two-year period. Patients admitted to beds 13 and 7 had similar Charlson Index scores (Chi Square 0.6, p-value=0.4). There was a total of 550 deaths and 820 AEs occurred over a two-year period (Table 2). The frequency of deaths and type of AEs per hospital service is detailed in Table 3.
Frequencies of mortality and adverse events in each hospital service in relation to beds 13 and 7.
| Hospital Service | ICU | Surgery | Medicine | Gastroenterology | Paediatrics | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Bed identifier | 13 | 7 | 13 | 7 | 13 | 7 | 13 | 7 | 13 | 7 |
| Total number of admissions | 240 | 298 | 1.519 | 1.309 | 1.605 | 1.593 | 564 | 492 | 414 | 519 |
| Total deaths | 49 | 68 | 21 | 28 | 169 | 164 | 29 | 22 | 0 | 0 |
| Total cases of infection related to medical care [ICD Codes CIE-10-ESa: T80.211, T83.51, J95.851] | 31 | 26 | 24 | 19 | 10 | 17 | 6 | 5 | 0 | 0 |
| Total cases with readmission | 8 | 17 | 93 | 81 | 113 | 114 | 57 | 37 | 10 | 17 |
| Total cases of death in DRG of low mortality | 1 | 1 | 0 | 0 | 3 | 2 | 0 | 0 | 0 | 0 |
| Total cases of pressure ulcers | 7 | 13 | 13 | 4 | 18 | 23 | 1 | 0 | 0 | 0 |
| Total cases of reoperation | 5 | 9 | 14 | 7 | 0 | 0 | 0 | 0 | 1 | 0 |
| Total cases of postoperative sepsis [ICD Codes CIE-10-ES: T81.4] | 2 | 1 | 4 | 8 | 0 | 0 | 1 | 1 | 0 | 0 |
| Total number of deaths events and safety incidents | 103 | 135 | 169 | 145 | 313 | 320 | 94 | 63 | 11 | 17 |
Mortality of patients admitted to bed 13 as a whole consisted of 268 cases (6.2% of total admissions, 95%CI 5.5–6.9) and 282 to bed 7 (6.7% of total admissions, 95%CI 5.9–7.5) (p-value=0.3). Considering the number of admissions, the Odds Ratio of death event when admitted to bed 13 versus bed 7 was equal to 0.9 (95% CI 0.8–1.1). The percentage of patients exposed to risk was 0.5.
Frequency of adverse eventsOver the two-year study, 422 AEs occurred in a total of 4342 admissions to bed 13 (9.7% incidence of AEs originating in the hospital, 95%CI 8.9–10.6), while 398 AEs occurred in a total of 4211 admissions to bed 7 (9.4%, 95%CI 8.6–10.4) (p-value=0.6). Considering the number of admissions, the OR of suffering an AE when admitted to bed 13 versus bed 7 was equal to 1.03 (95% CI 0.9–1.2). The percentage of patients exposed to risk was 0.5.
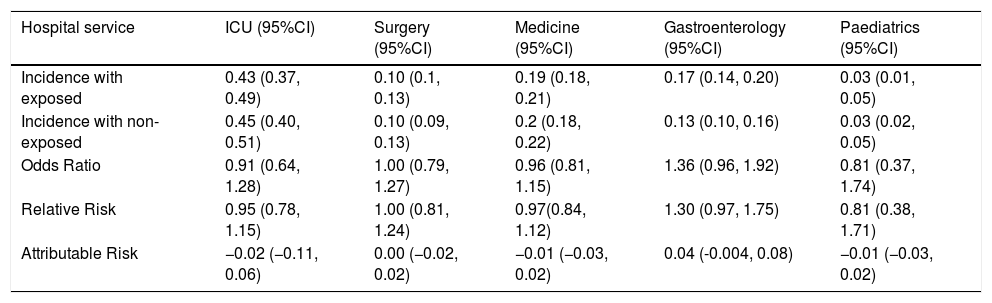
When considering the frequencies, the sum of deaths and AEs produced in each of the hospital services, OR values of around 1 were observed, except in the case of Paediatrics which was 0.8 (95% CI 0.4–1.7) and Gastroenterology 1.4 (95% CI 0.9–1.9) (Table 4).
Risk related to admission in bed 13 as opposed to bed 7.
| Hospital service | ICU (95%CI) | Surgery (95%CI) | Medicine (95%CI) | Gastroenterology (95%CI) | Paediatrics (95%CI) |
|---|---|---|---|---|---|
| Incidence with exposed | 0.43 (0.37, 0.49) | 0.10 (0.1, 0.13) | 0.19 (0.18, 0.21) | 0.17 (0.14, 0.20) | 0.03 (0.01, 0.05) |
| Incidence with non-exposed | 0.45 (0.40, 0.51) | 0.10 (0.09, 0.13) | 0.2 (0.18, 0.22) | 0.13 (0.10, 0.16) | 0.03 (0.02, 0.05) |
| Odds Ratio | 0.91 (0.64, 1.28) | 1.00 (0.79, 1.27) | 0.96 (0.81, 1.15) | 1.36 (0.96, 1.92) | 0.81 (0.37, 1.74) |
| Relative Risk | 0.95 (0.78, 1.15) | 1.00 (0.81, 1.24) | 0.97(0.84, 1.12) | 1.30 (0.97, 1.75) | 0.81 (0.38, 1.71) |
| Attributable Risk | −0.02 (−0.11, 0.06) | 0.00 (−0.02, 0.02) | −0.01 (−0.03, 0.02) | 0.04 (-0.004, 0.08) | −0.01 (−0.03, 0.02) |
Patients admitted to bed 13 (‘bad luck’).
Patients admitted to bed 7 (‘good luck’).
The likelihood of a patient suffering avoidable AEs in the course of health care is not a matter of bad luck; it has to do with how the (known) risks inherent in health care are managed. Based on these data, it can be affirmed that the interventions carried out by some hospitals to reduce the risk factor for the safety of patients consisting of avoiding bed 13 in medical and surgical services, are unnecessary. The incidence of AEs in hospitals included in this study follows a pattern similar to that which has been highlighted in other studies15–17 indicating that other factors other than bad luck should be explored as determinants of these incidents. These results confirm the fallacy already demonstrated of other works for example analysing urgent care activity, surgery outcomes, on Friday the 13th,17 the mortality rate in the seventh lunar month18 (phantom month), or the combine effect of the Friday the 13th and the full moon (known as “worst case scenario”) on the risk of injury, hospital admission or disease.19
Therefore, to increase patient safety, it is necessary to focus attention on other strategies, such as those based on strengthening the culture of positive safety in hospitals20–22 and carrying out the set of safe practices recommended by international organisations and scientific societies.23
Patient pressure, or the professionals’ own beliefs (which should not be ruled out), can alter medical decisions and affect healthcare spending.24–26 This study should serve to draw attention to some organisational and clinical decisions (such as delay interventions or discharges to perform them on a given day) that do nothing but contribute to extend the belief in these superstition.7 Admissions showed a similar mortality and a similar number of AEs and, according to the data, similar to that found in studies on incidence of AEs in Spanish hospitals27 or in other countries.15 There were no statistical neither clinically relevant differences.
These results can be taken into consideration from a one-size fits all approach. Since the participation of patients in decisions regarding their care and attitude are basic requirements to achieve patient-centred care, centres should not avoid bed-numbering 13 since, as we know, superstitions are acquired, among other means, by vicarious learning,28 through the testimony or acts of third parties.
Strengths and limitations of this studyA large number of hospitals participated in this study. When controlling the number of admissions over two years, the period of analysis of potential effects associated with bad luck is appropriate. Before comparison between beds patient complexity was evaluated. The methodology used with blind data extraction and comparing with bed 7 (good luck) avoids potential selection biases.
Whether the same patient suffered more than one AE was not taken into consideration. This study was not designed to analyse the fact that a jinxed patient or a professional was a causal factor of the incidents.
The 13th is simply the one that follows the 12nd. AEs are not due to bad or good luck, so actions aimed at improving safety should focus on those factors on which there is proven evidence.
ImplicationsAs a consequence of this study, the Spanish Strategy for Patient Safety, and probably in the strategy of no other country, does not require modifications and the safe practices recommended by WHO and the Spanish Ministry of Health do not need to be modified. On the contrary, they need to be rigorously implanted. The best available evidence, rather than the application of unfounded beliefs, is the best strategy to guarantee and improve patient safety.
FundingThis study has been carried out without requiring funds from any of the participating centres. Researchers have dedicated their free time to carry out this research in an altruistic way and with a good strict, and funny disposition.
Conflict of interestNo author is superstitious. No other conflict of interest.
Our thanks to the Health Services of Andalusia, Aragon, Madrid, Murcia, Navarre and Valencia. The work would not have been possible without the collaboration of the professionals in charge of the information systems of these health services. José Morant contributed to organise data. José Vicente Segura advised us in the statistical analysis.