Determine the effect of an intervention to reduce the length of stay (LOS) in appendectomies.
MethodsA four-quarter quality improvement initiative was developed after approval by the facility Quality Management Department, including educational sessions about the best practices regarding the hospital care for patients with appendicitis and recommendations to limit the LOS for no complicated appendicitis unless associated conditions were present, monitoring of the LOS and feedback to the staff and leaders.
Results692 appendectomies were performed, 365 (52.7%)) of them during the intervention. The mean LOS was 3.94 days with a decreasing trend during the study period. The complicated appendicitis had a mean LOS of 6.42 days (SD, 3.85) during the baseline and 5.27 days (SD 2.50) during the intervention (p=0.03), representing a 17.9% reduction. The not complicated appendicitis during baseline had LOS of 3.82 days (SD 4.17) with a subsequent reduction to 2.95 days (SD 1.53) in the intervention. The total saving bed days during the intervention were 338.04 days, which 254.04 days (75.2%) were in non complicated appendectomies. One patient required readmission during the intervention because of an organ space surgical site infection, with proper recovery after antibiotic treatment.
ConclusionOur study provides evidence about the possibility to optimize the bed use with a simple educational intervention, and should be considered a step to achieve additional reductions in the hospital stay of patients who undergo laparoscopic appendectomies.
Determinar el efecto de una intervención para reducir la estancia hospitalaria (LOS) en las apendicectomías.
MétodosPrevia aprobación por el comité de calidad se desarrolló una intervención que incluyó sesiones educativas sobre las mejores prácticas en la atención hospitalaria para pacientes con apendicitis y recomendaciones para limitar la estadía hospitalaria, monitoreo de la estadía y retroalimentación al personal y a los líderes.
ResultadosSe realizaron 692 apendicectomías, 365 (52,7%) de ellas durante la intervención. La estancia hospitalaria fue de 3,94 días con una tendencia decreciente durante el período de estudio. La apendicitis complicada tuvo una estancia de 6,42 días (desviación estándar [DE] 3,85) durante el periodo pre-intervención y de 5,27 días (DE 2,50) durante la intervención (p=0,03), lo que representa una reducción del 17,9%. En la apendicitis no complicada durante la pre-intervención la estancia fue de 3.82 días (DE, 4.17) con una reducción a 2,95 días (DE 1,53) durante la intervención. El ahorro total de días de cama durante la intervención fue de 338,04 días, de los cuales 254,04 días (75,2%) fueron en apendicectomías no complicadas. Un paciente requirió reingreso durante la intervención debido a una infección en el sitio quirúrgico órgano y espacios, con una recuperación adecuada después del tratamiento con antibióticos.
ConclusiónNuestro estudio proporciona evidencias sobre la posibilidad de optimizar el uso de la cama con una intervención educativa simple, siendo posible lograr reducciones adicionales en la estancia hospitalaria de los pacientes que se someten a apendicectomías laparoscópicas.
Bed utilization is a critical component for the efficiency of hospital services, especially in an environment of limited resources and increasing population. The reduction of the length of stay (LOS) in elective and emergency surgeries has become a standard practice in a wide range of procedures, once the advances in technology and improved patient care algorithm have been introduced. It should be considered the pre and post-procedure components of the LOS in these patients, which the stay after surgical procedure could be minimize in laparoscopic surgeries.
In laparoscopic appendectomies for non-complicated or non-perforated appendicitis, the studies conducted in adults and pediatric populations have shown benefits of outpatients or same day discharge in terms of reduced LOS, morbidity and readmission rate.1–4 Oyentunji et al identified in a national sample of American hospitals a significant variability of same day discharge (SDD) in pediatric patients and its increased use for children with nonperforated appendectomies5 and Frazee et al in adult patients in a single center experience reports the benefit of outpatient procedure.1
We identified a longer LOS in patients with appendectomies in a 75-beds facility, which was related to frequent bed crisis and not well supported by clinical or other evidence that support prolonged hospital stay. The aim of this study was to determine the effect of an educational intervention to reduce the LOS in appendectomies.
MethodsThis quality improvement study was performed in a community hospital during a four-quarter period (January–December, 2016). All adult patients who underwent appendectomies during the study period were included.
The following information was collected from the electronic medical record: age, sex, comorbidities, appendicitis according clinical findings (flemonous, suppurative, gangrenous, perforated),the procedure technique (laparoscopic, open), the physical status classification according eht American Society of Anesthesiologists and diagnosis of surgical site infections. The noncomplicated appendicitis was considered the flemonous and suppurative appendicitis according to operative findings and complicated the gangrenous and perforated. All patients received a single dose of cefuroxime plus metronidazole, but for the complicated appendicitis it was recommended a full therapeutic antibiotic schedule (corporate policy CL 7197 Antimicrobial Prescribing). The standardized surveillance criteria for defining surgical site infection as developed by the Centers for Disease Control (CDC) were used6 and performed by an infection control practitioner during the admission and 30-days after the procedures using postdischarge surveillance methods.
Quality improvement interventionThe intervention was approved as a quality improvement project by the facility Quality and Safety Committee with the primary goals of reducing the LOS in appendectomies, mainly focused on complicated appendicitis. It included: educational sessions, daily monitoring of the LOS of admitted patients and a monthly summary report and feedback to the staff and leaders. The educational sessions were conducted with the surgical staff (10 surgeons) and includes an initial session about the best practices regarding the requirement of hospital care for patients with appendicitis, with recommendations to limit the LOS for no complicated appendicitis unless associated conditions were present. After that a monthly session was conducted for the analysis of bed utilization and strategies for improvement. By consensus with the surgical staff, the recommended LOS for no-complicated appendicitis was two days, without specific LOS for complicated cases. For comparison, it was considered as baseline period the four-quarters previous to the intervention.
The majority of the patients who underwent appendectomies were transferred from others corporate facilities, reason why the LOS was considered the time from the admission to discharge in our facility, excluding the time spent in other facilities.
Statistical analysisStatistical analysis was performed using JMP 5.1 (SAS Institute, http://www.jmp.com/). Descriptive statistical methods were used. The incidence of SSI was calculated, by dividing the number of infections by the number of operations performed and multiplying it by 100. The mean LOS and standard deviation (SD) were calculated according to appendicitis type. Comparison of the variables was performed using student's t-test or chi-square test as required. Significance was set at p<.05.
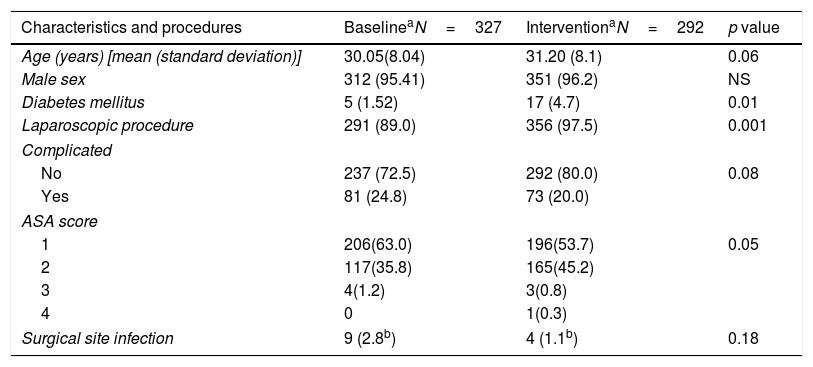
ResultsDuring the study period 692 appendectomies, of which 365 (52.7%) were performed during the intervention. No differences in demographics and the surgical site infection rate were observed among the periods, while during the intervention period more laparoscopic appendectomies were performed (97.5%) (p<0.001). During the intervention, the 80.0% of the appendicitis were considered non-complicated, while during the baseline the 72.5% fall in this category (p=0.08) (Table 1). Also, the majority of patients had ASA score 1 and 2 with an increased frequency of patients with mild systemic disease (ASA 2) during the intervention (45.2%).
Patients characteristics and procedures before and after intervention.
| Characteristics and procedures | BaselineaN=327 | InterventionaN=292 | p value |
|---|---|---|---|
| Age (years) [mean (standard deviation)] | 30.05(8.04) | 31.20 (8.1) | 0.06 |
| Male sex | 312 (95.41) | 351 (96.2) | NS |
| Diabetes mellitus | 5 (1.52) | 17 (4.7) | 0.01 |
| Laparoscopic procedure | 291 (89.0) | 356 (97.5) | 0.001 |
| Complicated | |||
| No | 237 (72.5) | 292 (80.0) | 0.08 |
| Yes | 81 (24.8) | 73 (20.0) | |
| ASA score | |||
| 1 | 206(63.0) | 196(53.7) | 0.05 |
| 2 | 117(35.8) | 165(45.2) | |
| 3 | 4(1.2) | 3(0.8) | |
| 4 | 0 | 1(0.3) | |
| Surgical site infection | 9 (2.8b) | 4 (1.1b) | 0.18 |
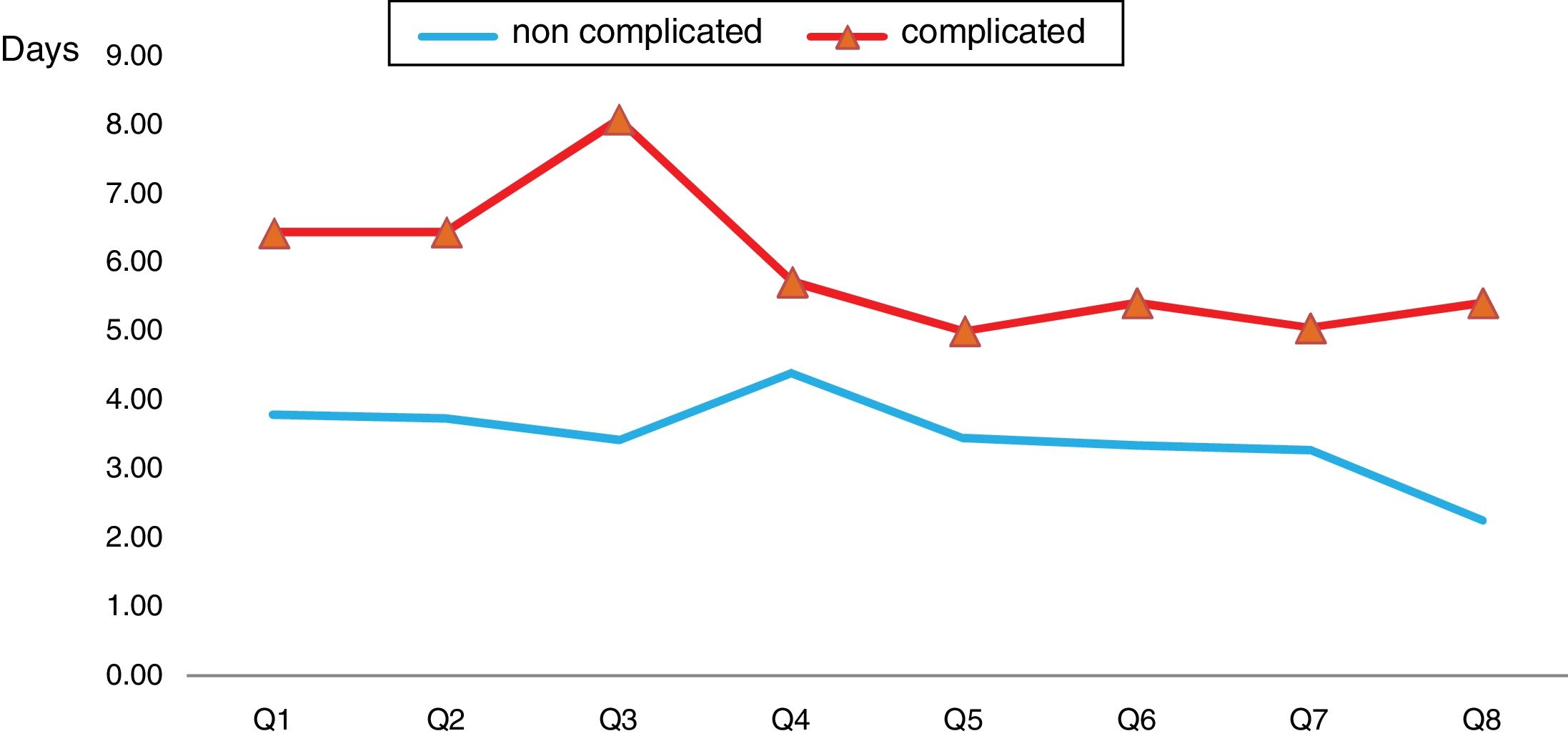
The mean LOS was 3.94 days (median 3 days), with a decreasing trend during the study period, especially during the last two-quarters of the intervention (Fig. 1). The complicated appendicitis had a mean LOS of 6.42 days (SD, 3.85) during the baseline and 5.27 days (SD, 2.50) during the intervention (p=0.03), representing a 17.9% reduction in LOS. The not complicated appendicitis during baseline had LOS of 3.82 days (SD, 4.17) with a subsequent reduction to 2.95 days (SD, 1.53) in the intervention (p=0.001), with the lowest figure in the last quarter (2.24 days (SD, 0.55)) (Fig. 2). The total saving bed days during the intervention were 338.04 days, which 254.04 days (75.2%) were in non complicated appendectomies.
During the intervention period, one patient required readmission because of an organ space surgical site infection, with proper recovery after antibiotic treatment.
DiscussionIn this quality improvement intervention, we found a reduction of length of stay in appendectomies as a result of the staff education, monitoring outcomes including LOS and feedback to staff. These measures will be considered basic in many quality improvement interventions, and should be implemented as a “bundle” to provide, in our study, the best evidence about the benefits of reducing the LOS with minimal risk for the patients. During the last quarter of the intervention was achieved the minimun length of stay probably related with the effectiveness of the measures implemented.
The LOS in patients who underwent appendectomies is variable according to different studies and settings; nevertheless, in general, is longer for complicated appendicitis, performed by open procedures or when antibiotics treatment is required.7–9 Sutton et al described a mean LOS of 5.32 days and 2.18 days for complicated and non-complicated appendectomies,7 while Kim et al described longer LOS in patients who received postoperative antibiotics.10
In our study the hospital stay for non-complicated appendectomies was considered more than the required for standard care, taking into consideration that the majority of these patients after the laparoscopic procedure did not require additional antibiotics or IV fluids. Regularly, analgesic medications could be provided by parenteral route during and immediately after the procedure, it could be but switched to oral route as soon as possible. No clear reasons explain the long stay of non complicated appendicitis after the surgical procedures. Nevertheless, previous physician behaviours could be a factor related with this results, because all the surgeons are new hired from other countries with differents practices.
In complicated appendectomies, the possibility to minimize the LOS is less compared with the non-complicated. However, in specific patients, the proper duration of postoperative antibiotics or the switch from IV to oral could be considered to limit the hospital stay, without adverse consequences for the patients.8
There are few reports about the outpatient laparoscopic appendectomy or same day discharge in adult patients. In the study of Frazee et al in 484 patients managed as outpatients, they achieved an overall success of 85%, without mortality or reoperations.1 In pediatric patients, a reduction of 37% of the LOS was achieved with the use of a discharge pathway, that included clinical criteria.4
The principal limitation of the study is its single center design. Nevertheless, the number of cases and the caracteristic of the improvement actions constituted strenghts related with the reproducibility of the intervention in other settings.
Our study provides evidence about the possibility to optimize the bed use with a simple educational intervention, and should be considered a step to achieve additional reductions in the hospital stay of patients who undergo laparoscopic appendectomies.
FundingNo funding received to conduct this study.
Ethical approval and informed consentNot required for this paper because was considered a quality improvement project, but approval from Quality Management Department was obtained to conduct and publish it.
Conflicts of interestNo conflict of interest to declare for all the authors.
I would like to thank the assistance of Mr. Carlos L. Crespo Palacios for reviewing this paper.