Administrative and medical processes of the healthcare organizations are rapidly changing because of the use of artificial intelligence (AI) systems. This change demonstrates the critical impact of AI at multiple activities, particularly in medical processes related to early detection and diagnosis. Previous studies suggest that AI can raise the quality of services in the healthcare industry. AI-based technologies have reported to improve human life quality, making life easier, safer and more productive. This study presents a systematic review of academic articles on the application of AI in the healthcare sector. The review initially considered 1,988 academic articles from major scholarly databases. After a careful review, the list was filtered down to 180 articles for full analysis to present a classification framework based on four dimensions: AI-enabled healthcare benefits, challenges, methodologies, and functionalities. It was identified that AI continues to significantly outperform humans in terms of accuracy, efficiency and timely execution of medical and related administrative processes. Benefits for patients’ map directly to the relevant AI functionalities in the categories of diagnosis, treatment, consultation and health monitoring for self-management of chronic conditions. Implications for future research directions are identified in the areas of value-added healthcare services for medical decision-making, security and privacy for patient data, health monitoring features, and creative IT service delivery models using AI.
Since the industrial revolution, there has been a tremendous and continuing advancement and prioritization of technology in production and growth (Li et al., 2017; Ali et al., 2022). Arduous and manual tasks have been replaced by technological advancements in machines that have progressed human development (Kaplan and Haenlein, 2020). Beyond the physical labor support offered by machines, artificial intelligence (AI) is a key technological advancement that has enabled humans to replace manual work with superior mental capacities and intellectual levels in a variety of industries (Chien et al., 2020; Kumar et al., 2023). AI is a discipline of science and technology that enables intelligent computers and computer programs to undertake activities traditionally requiring human intelligence (Aiken and Epstein, 2000). Consequently, a key attraction of AI is that it can perform a variety of human-like functions, learn from experience and adapt to new inputs and settings. To attain superior performance for specified tasks, AI makes use of relevant information sources such as Big Data (Kaplan and Haenlein, 2020).
AI has swiftly advanced in recent years and has been applied to offer many benefits across various industries, including the critical health-care industry (Minz and Mahobiya, 2017; Ribbens et al., 2014; Strachna and Asan, 2020). AI has already digitally transformed the manual health system into an automated version in many areas, whereby in some applications, humans are now only required to perform more fundamental duties in medical practice to manage patients and medical resources (Comito et al., 2020; Yu and Zhou, 2021; Bernardini et al., 2021), leaving complicated procedures to be handled by or dependent on AI components. AI-based healthcare systems are rapidly evolving, particularly for early detection and diagnostic applications (Chen, 2018; Dhieb et al., 2020; Yu and Zhou, 2021; Merhi, 2022). These developments enable AI to accomplish tasks that humans sometimes cannot perform with the pace, simplicity, reliability and diligence that AI can deliver at a lower cost (Sqalli and Al-Thani, 2019; Zhou et al., 2020). When Information Systems (IS) developers can effectively design AI systems to carry out specific tasks, the technological advancement from healthcare digitization can also overcome additional challenges (Tobore et al., 2019). For example, AI can significantly enhance patient care while simultaneously lowering healthcare expenses (Wahl et al., 2018; Dhieb et al., 2020; Kaur et al., 2021). The growing human population is likely to increase the need for healthcare services to be delivered at a rapid pace; therefore, innovative AI solutions are needed in the healthcare sector to improve effectiveness and efficiency without increasing costs (Pee et al., 2019). This is one area where AI continue to play a pioneer role in providing innovative solutions. Rapid technological advancements, particularly in the realm of AI, have already supported the management of the healthcare industry's growth (Maduri et al., 2020; Comito et al., 2020).
Recent AI technologies encompass Big Data, machine learning applications, and robots that are utilized to monitor, detect, and measure risks and benefits in the healthcare industry (Hossen and Armoker, 2020; Dharani & Krishnan, 2021; Duan et al., 2022). To enhance procedures and facilitate the administration of medical services, the healthcare business relies heavily on medical data and analytics. In recent years, the amount of gathered medical data and its dimensions have exponentially expanded. For example, medical professionals, researchers, and patients generate massive amounts of data, such as electronic health records (EHRs), medical imaging data, and other data from various monitoring devices, including health tracking devices and apps, that people are increasingly using in normal circumstances beyond the need for medical attention (Antoniou et al., 2018; Liu et al., 2020; Xie et al., 2020). In this environment, AI technology has the capacity to capture data, process it, perform dynamic analyses and produce results that can be effectively used for medical intervention (Comito et al., 2020). This function is typically executed using machine learning algorithms supported by data storage and processing power (Charan et al., 2018; Woo et al., 2021). For example, patient behavior patterns may be able to establish reliable predictions via daily observation of medical data. As a result, AI may offer suggestions toward diagnosis, medical intervention, therapeutic insights and strategies for mitigating health deterioration and supporting proactive strategies to prevent patient conditions from worsening, thereby enhancing patient outcomes at various phases of diagnosis and illness, as well as medication prescription and use. Technologically advanced hospitals are now exploring the use of AI technologies to help improve the accuracy of practice (Zhou et al., 2020; Mary et al., 2020) and lower the cost of operations (Sqalli and Al-Thani, 2019; Zhou et al., 2020). By presenting detailed information on a variety of treatment options, AI enables medical staff and patients to make informed decisions about treatment plans (Deng et al., 2019).
While a rosy picture of the future of AI can be imagined in terms of its capabilities and opportunities, it must be recognized that AI can also present a number of challenges and ongoing issues due to the complexity of the integration of healthcare environments with a purely machine learning-supported AI intervention. Some of the main risks and challenges that have emerged are patient injury from system errors (Aljaaf et al., 2015; Srivastava and Rossi, 2019; Madanan et al., 2021; Dwivedi et al., 2021), patient privacy concerns limiting data access, and the ethical, legal and medical challenges of making decisions about human lives and medical conditions using AI (Liu et al., 2020; Shaban-Nejad et al., 2021).
Regardless of the AI challenges, one of the most important benefits of AI is its support in preventative care in the healthcare system that promotes all humans to become and remain healthy. For example, apps have been used to give patients more control over their health (Antoniou et al., 2018; Jaiman and Urovi, 2020; Samuel et al., 2022), allowing them to make evidence-based decisions on the matters of preventative health issues, such as type 2 diabetes and high blood pressure. However, early detection and diagnostics of health information require many AI apps (Stamford et al., 2016; Siddiqui et al., 2018; Kumar and Suresh, 2019). These AI apps are used in a variety of settings to diagnose different types of illnesses for precise, rapid and reliable results (Ribbens et al., 2019; Sasubilli et al., 2020; Jahan and Tripathi, 2021). At the simplest level, AI performs a significant level of comparative analysis using Big Data so that information from a patient is compared with data and digital images from huge datasets compiled from other patients in relevant and related settings (Charan et al., 2018; Somasundaram et al., 2020). This type of self-learning mechanism recognizes patterns and provides information for medical practitioners to support their diagnosis and intervention strategies (Charan et al., 2018; Woo et al., 2021). While supporting these complex medical procedures, AI technologies can also improve the efficiency of medical care administration (Deng et al., 2019; Daltayanni et al., 2012).
This systematic review includes a discussion of the benefits, challenges, methodologies, and functionalities related to AI in the healthcare sector (Murphy et al., 2021). To fully understand these dimensions of AI, additional research is needed on both the practical and theoretical aspects of AI (Chen et al., 2020; Johnson et al., 2022). There are interesting evolving insights of AI, such as the power of AI to exercise doctors' rights and obligations (Yang, 2018; McGregor, 2020), AI issues regarding privacy protection (Wang et al., 2020; Zhou et al., 2021), and how AI can store, process, edit, and share health data in consideration of permission from patients and ethics committees? Governments could also establish legislative guidelines to secure healthcare data (Gomoi and Stoicu-Tivadar, 2010; Bhaduri et al., 2011). Furthermore, raw data acquired from patients and hospitals are used by machine learning and expert systems, however while collecting these data, ethical considerations should be considered (Liu et al., 2020; Shaban-Nejad et al., 2021). The norms of technology development and health applications must be established to optimally use AI technology in medical care. To meet this objective, this review study presents the state-of-the-art of the application of AI in the healthcare sector and proposes a classification framework to determine the benefits, challenges, methodologies, and functionalities of the use of AI in health services.
An overview on the current use of AI in the healthcare sector is presented next. Then, background information on AI and relevant applications are explained. This is followed by the research methodology detailing the SR mapping process and presenting research results based on a classification framework. Subsequently, discussion of current literature in terms of the four dimensions of benefits, challenges, methodologies, and functionalities of AI for the healthcare industry is presented. Finally, implications to future research and practice are highlighted.
Background on artificial intelligenceAI or machine intelligence is an area of computer science whereby machines are programmed with the ability to perform intelligent tasks that are usually undertaken by humans (Tsang et al., 2020). Computers and machines use AI techniques to understand, analyze, and learn from data through specifically designed algorithms (Sasubilli et al., 2020). For example, with today's AI technologies, cameras can automatically recognize faces, computers can translate from one language to another, it is easy to search and find products in e-commerce, computers can assist doctors in making decisions and so on (Sasubilli et al., 2020). In the 1930s, Alan Turing developed the first Turing machines for intelligent mathematical calculations that can be undertaken automatically, paving a way for the start of the AI technology. AI was founded as an academic discipline since 1950s and since then, it has been significantly researched in areas such as natural language processing, learning, reasoning and knowledge representation. More recently, AI has been transformed with the expansion of its research beyond computer science, with the recent developments drawing on broad areas such as psychology, linguistics, and philosophy. Consequently, AI has been applied in various areas, such as education, e-commerce, robotics, navigation, healthcare, agriculture, military, marketing and games. More specifically, widely adopted AI applications include search engines such as Google, recommender systems such as Netflix, self-driving cars such as Tesla, and human speech recognition systems such as Siri and Alexa. In general, AI methods can be broadly categorized in these areas: machine learning (Bernardini et al., 2021); robotics; natural language processing (Patii and Iyer, 2017; Murray et al., 2019); computer vision (Jahan and Tripathi, 2021); and big data (Hossen and Armoker, 2020).
Classification and clustering are two major techniques used in AI machine learning. Both algorithms use data, such as numbers, text, images and videos, as input (Jahan and Tripathi, 2021). Classification algorithms (such as neural networks, decision trees and Bayesian networks) use huge amounts of data as training datasets. There are two types of classification algorithms: supervised and unsupervised learning. Supervised learning uses labeled data vectors during training; by contrast, unsupervised learning algorithms do not use labels. Both methods use class labels during the testing phase. In machine learning, clustering algorithms are used for unsupervised learning and do not need any class label data. Prediction algorithms are trained using historical data to develop forecasting models. Several algorithms are used in classification, clustering and prediction, as given below (Elbasi et al., 2021):
- •
Classification: Decision tree, Naïve Bayes classifier, Bayesian network, Random Forest, Neural network, Deep learning, Support vector machines,
- •
Clustering: K-means, Mean shift, Expectation-Maximization, Gaussian mixture model,
- •
Prediction: Linear regression, Learning vector quantization, Logistic regression, K-nearest neighbors
Some researchers believe in “strong AI”, which means machines can be equally intelligent as humans. On the other hand, “weak AI” has limited functionalities (Gomoi and Stoicu-Tivadar, 2010). In weak AI, problems are solved using AI algorithms where machines are trained by AI system developers. E-commerce recommendation systems, medical assistant applications, and voice-based personal assistants such as Siri are examples of weak AI applications. In strong AI, machines can make independent decisions without human intervention. There are several applications of strong AI, such as in cybersecurity, the entertainment sector and behavioral recognition and prediction. Deep learning is also widely used for solving complex problems. Deep learning is a subset of machine learning using a multilayer artificial neural network. Deep learning algorithms can be used in self-driving cars, fraud detection, healthcare, entertainment, machine translation and virtual assistants.
AI and its sub-areas such as robotics, internet of things, and machine learning can have significant impacts on our societies. AI technology can improve human life quality, making life easier, safer and more productive (Malik et al., 2021; Grover et al., 2020; Hradecky et al., 2022). There are several application areas of AI that make our life easier such as face recognition for security, automation for industry, natural language processing for translation, robotics for homes, machine learning and vision for healthcare (Herath et al., 2022). AI has transformed our society to move into the Industry 4.0 revolution due to the internet of things, cloud computing, robotics, cyber physical systems and machine to machine communication (Votto et al., 2021). When used effectively, the smart automation and interconnectivity can allow people to save time, manage work, flexibility and collaborations (Kar et al., 2021; Ahsan et al., 2022). However, technology skeptics question if AI is really needed in our daily life? AI can bring negative impact on societies such as undesirable social change, unemployment, wealth inequality and cybercrime. Therefore, the use of AI in different sectors of our society is currently an area of active research interest. On this note, this research paints a picture on the use of AI in the healthcare sector.
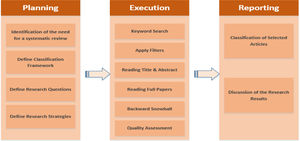
Review planning and methodologyA systematic review is a means of identifying, evaluating and interpreting all available research relevant to a particular research question, topic, or phenomenon of interest (Kitchenham and Charters, 2007). In addition, it is defined as a methodology that summarizes the process of collecting, arranging, and assessing literature in a review domain (Dabić et al., 2020; Paul et al., 2021). A systematic review was considered appropriate in this study based on the purpose of this research, which is to identify key findings in current research and to offer suggestions for future research (Eteokleous et al., 2016; Paul and Benito, 2018; Hao et al., 2019). A systematic review can contribute significantly to the understanding of the research area, identifying lacunas and suggesting forthcoming research themes (Khatoon and Rehman, 2021). Systematic reviews can take numerous forms; they have been categorized by some researchers as domain, theory and method-based reviews (Palmatier et al., 2018), whereas Paul and Criado (2020) categorized systematic reviews into different sub-forms of domain-based reviews: structured theme-based reviews, framework-based reviews, bibliometric reviews, hybrid reviews, and conceptual reviews.
Systematic reviews have become increasingly important in all disciplines, and increasingly adopted in the combination areas of IT and healthcare sectors (Kamboj and Rahman, 2015). Professionals and academics involved in the IT and healthcare industries follow systematic reviews to stay abreast of their fields, and they are often used as a starting point for developing technology guidelines (Moher et al., 2009) for adoption in other areas, including healthcare. This systematic review is based on the structured process proposed by Watson (2015), which explicitly prescribes the steps and processes for literature searching. These searching process steps include planning, execution, and reporting. It is complex and time-consuming for IT professionals and healthcare experts to check relevant articles for evidence-based practice because of the huge number of continuously refreshing IT and healthcare-related publications (Bastian et al., 2010). Moreover, when IT professionals and healthcare experts make decisions, they do not depend on the results of a single study since some studies may elicit prejudices or based on limited data, making the results inconclusive (Abbas et al., 2008). In both practical and academic work, IT professionals and healthcare experts must rely on strong evidence to inform practice. According to Evans (2003), a systematic review is a pre-eminent approach to aid evidence-based IT and healthcare practice. Boell and Cecez-Kecmanovic (2015) assert that the rigor of following a pre-defined protocol and particular search process makes systematic review an efficient approach. Watson recognizes the relevance of efficiency in research but argues that effectiveness is also important. He states that effectiveness is attained by “synthesizing the literature and revealing the depth of knowledge on an area's critical key concepts and the relationships between these concepts” (Watson 2015, p. 185).
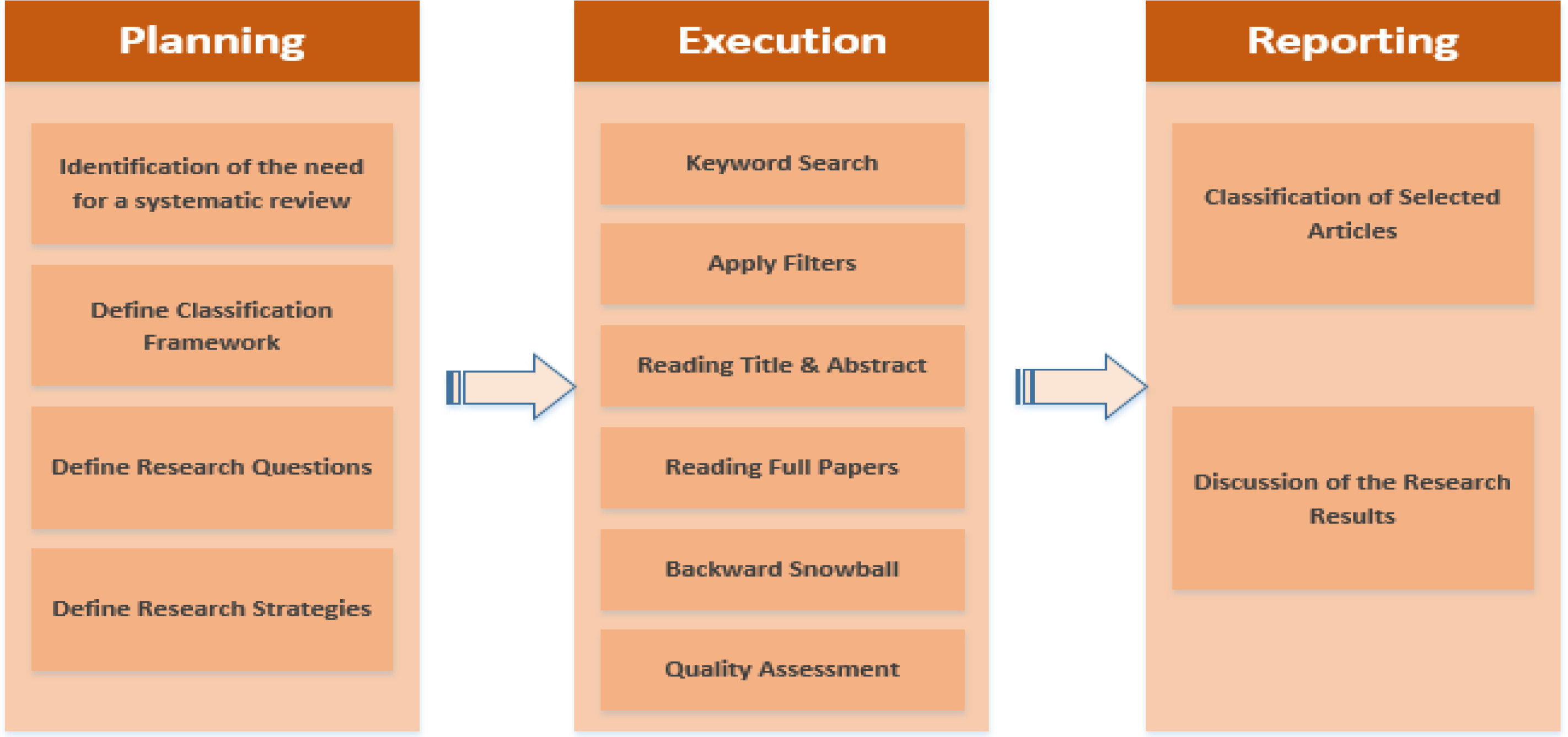
Applying the rules and guidelines of systematic reviews is crucial for researchers who undertake this approach (Kitchenham and Charters, 2007). Commencing the review process using a protocol to identify, select, and assess the relevant literature will make the systematic review highly efficient (Tranfield et al., 2003). The systematic process should be reproducible, objective, transparent, unbiased, and rigorous (Boell and Cecez-Kecmanovic, 2015). The systematic review approach adopted in the current paper embraces the strategies and rules depicted by Kitchenham and Charters (2007) and Ali et al. (2018a; 2020; 2021). This study is conducted in three stages, as proposed by Watson (2015). In addition, several collective rules and guidelines were applied for the different steps of this systematic review that are identified by Kitchenham and Charters (2007) and Ali et al. (2018a; 2020; 2021). Rules and guidelines applied during the planning stage include identification of the need for a systematic review, defining a classification framework, defining research questions, and defining research strategies. The execution step includes the techniques of keyword search, filter application, title and abstract reading, full article reading, backward snowball and quality assessment. In the reporting step, this research included classification of the selected articles and discussion of the results. The steps, rules and guidelines applied for this systematic review are described in Fig. 1.
Planning stageThe first step of the planning stage is to identify the requirements of the systematic review. The need for a systematic review arises from the requirement of researchers to summarize all existing information about a phenomenon in a thorough and unbiased manner. As argued in the previous section, there is dynamic research on how AI enables the healthcare sector in relation to functions, benefits, and challenges. However, to the best of our knowledge, there is no systematic review that outlines these research findings and provides a profound analysis of the research and practice related to this topic.
The second step of the planning stage consists of developing the research review protocol, which serves as a base to understand the current theoretical and practical perspectives on the topic. In this research, the review protocol specifies the methods used to undertake a specific systematic review. A predefined protocol is necessary to reduce the possibility of researcher bias. For example, without a protocol, the selection of individual studies or the analysis may be driven by researcher expectations. The initial classification framework was authored by Ngai and Wat (2002) who used it to conduct a systematic review of journal articles related to how advanced technologies enable various sectors. This type of classification framework has also been applied by Ali et al. (2018a; 2020) to investigate how cloud computing benefits the healthcare sector and to investigate how blockchain technology benefits the finance sector. In this research, the proposed classification framework has been updated by adding two new dimensions related to how AI is applied in the healthcare sector. The framework is divided into four different dimensions, specifically the benefits, challenges, methodology, and functionalities. Each of these dimensions consists of different categories that group several factors based on the findings of the review of the selected articles.
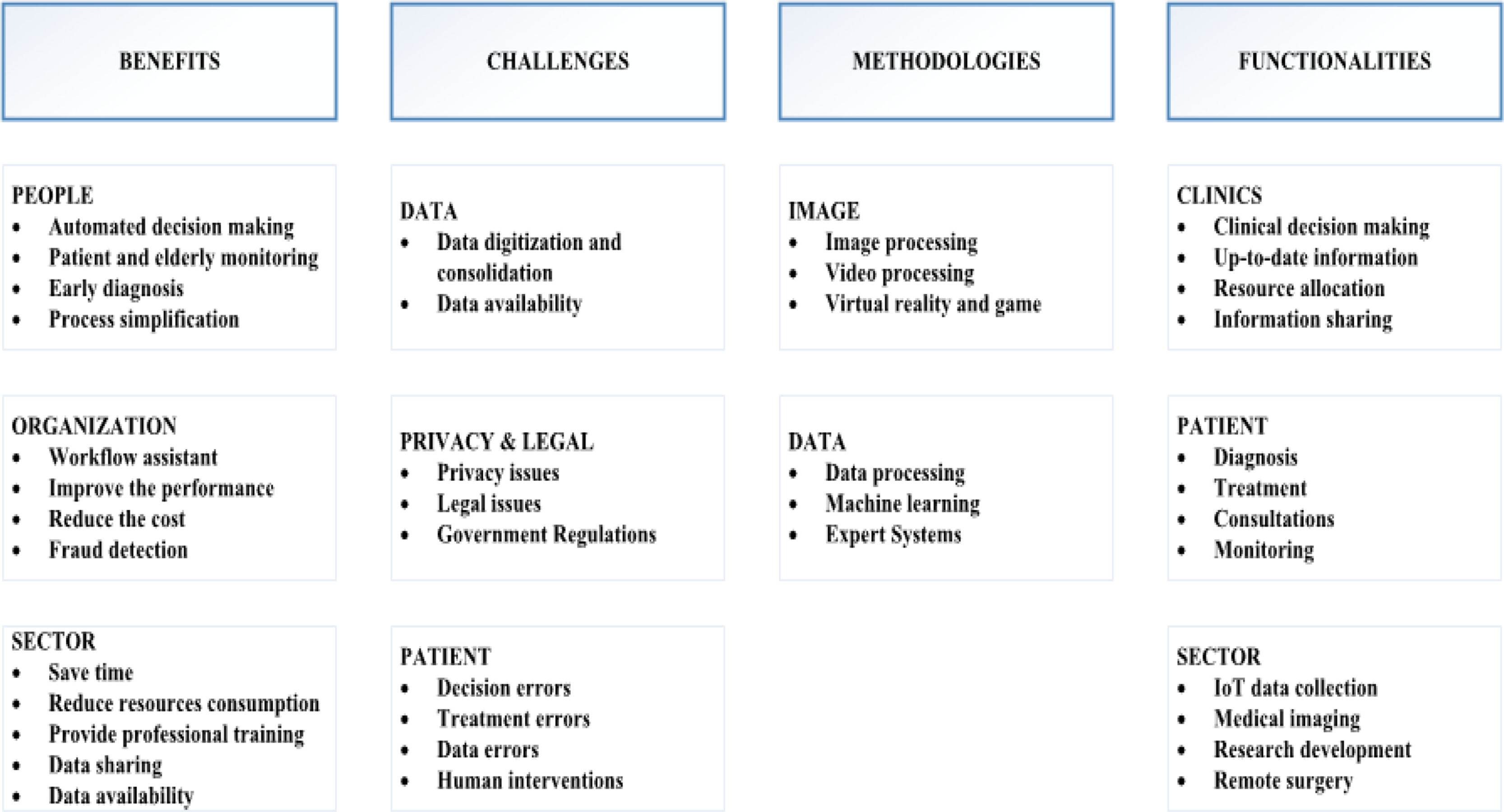
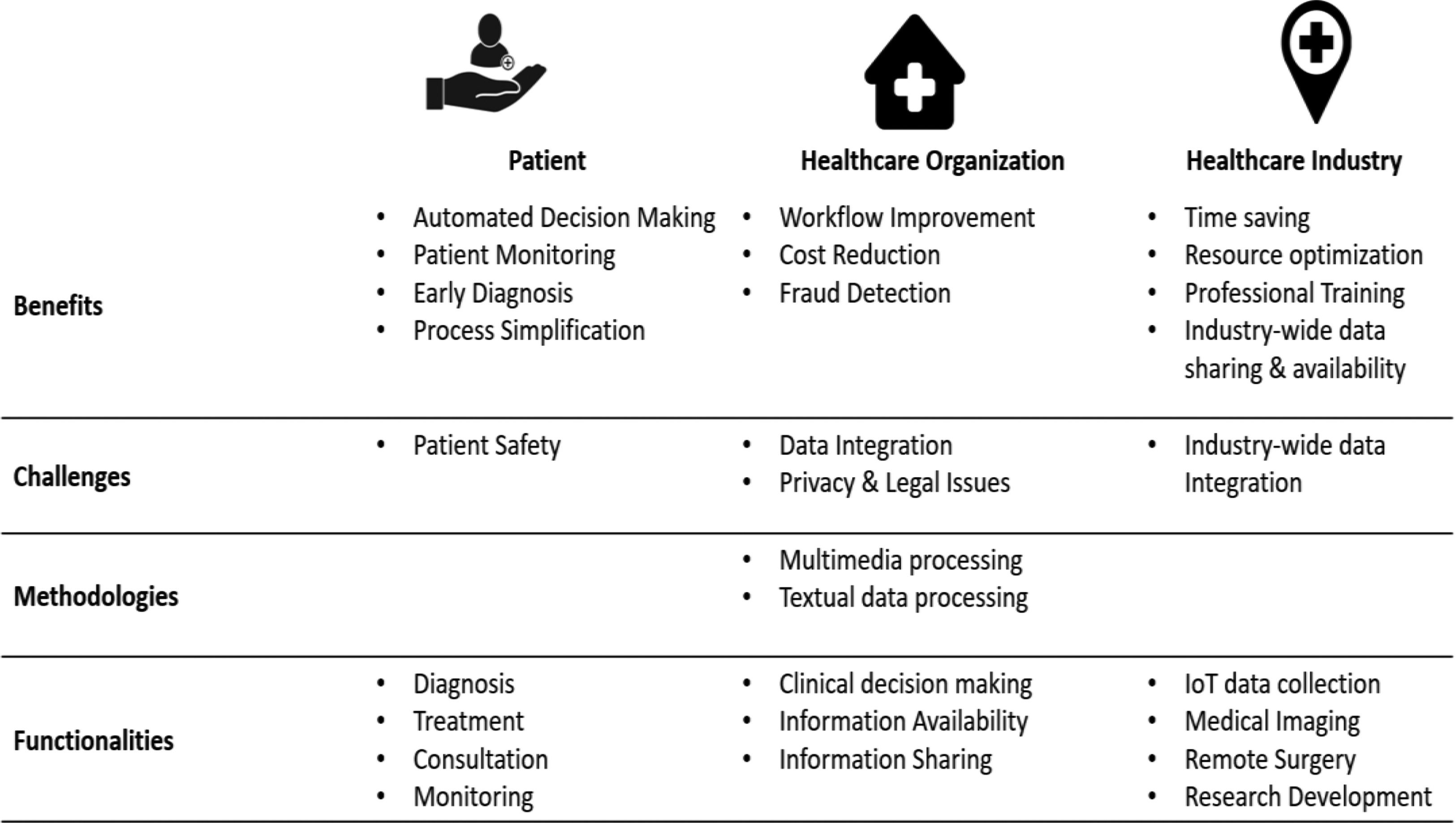
The developed classification framework encompasses four specific dimensions, and each dimension has specific categories. In each category, relevant factors were identified: (1) Benefits, which are the advantages that organizations obtain from using AI. These include benefits to people that consist of automated decision-making patient monitoring, particularly elderly patient monitoring; early diagnosis; and process simplification (Woo, 2021; Rahman, 2020; Sasubilli, 2020; Deebak, 2021). They also include benefits to organizations that consist of workflow assistance, improved performance, reduced cost, and fraud detection (Minz, 2017; Dhieb, 2020; Zhou, 2020; Bernardini, 2021). The final category of this dimension is benefits to sectors that consist of saving time, reducing resource consumption, and providing professional training, data sharing, and data availability (Guo, 2018; Gupta, 2019; Jaiman, 2020; Yu, 2021; Kaur, 2021). (2) Challenges are the issues that organizations might face when using AI. These include challenges related to the data, which consist of data digitization and consolidation and data availability (Patii, 2017; Chen, 2018; Murray, 2019; Dhieb, 2020). They also include privacy/legal challenges, which consist of privacy issues, legal issues, and government regulations (Jumelle, 2014; Bryson, 2018; Ali et al., 2018b; Zerka, 2020; Shaban-Nejad, 2021). The final category of this dimension refers to challenges related to the patient and that consist of decision errors, treatment errors, data errors, and human interventions (Lim, 2015; Hasan, 2017; Srivastava, 2019; Tsang, 2020; Madanan, 2021). (3) Methodology is the process that organizations adopt to use AI. It includes data processing, machine learning, and expert systems (Panayides, 2015; Ragde, 2016; Minz, 2017; Oktay, 2018; Saxena, 2019; Katarya, 2020; Srayya, 2021). (4) Functionalities refer to the features that organizations have access to, due to the use of AI. They include functionalities to clinics that consist of clinical decision-making, up-to-date information, resource allocation, and information sharing (Aljaaf, 2015; Lee, 2017; Zheng, 2018; Murray, 2019; Mary, 2020; Jahan, 2021). They also include functionalities to patients that consist of diagnosis, treatment, consultations, and monitoring (Hassan, 2016; Minz, 2017; Albayrak, 2018; Gandhi, 2019), Tsang, 2020; Dharani, 2021). The final category of this dimension is functionalities related to the sector that consist of IoT data collection, medical imaging, research development, and remote surgery (Lee, 2017; Yang, 2018; Ribbens, 2019; Noothout, 2020; Zhou, 2021; Firouzi et al., 2022). For more details on the dimensions, please refer to Fig 2.
Classification framework (Adapted from Ngai and Wat (2002))
In all, after filtering down the relevant articles to 180 that were part of this review, these articles were investigated based on the four dimensions of the classification framework, namely, benefits, challenges, methodology, and functionalities. Subsequently, the research classification framework was developed to review the literature related to the nature of how AI enables the healthcare sector in relation to the benefits, challenges, methodologies, and functionalities in healthcare research.
Defining the research questions is the third step in the planning stage and is considered a crucial step in any systematic review (Paul et al., 2021). A systematic review achieves its goals when it can answer the research questions (Paul and Benito, 2018). The research questions for this systematic review study are as follows:
- •
What is the most common impact of AI on the healthcare sector?
- •
What are the AI benefits, challenges, methodologies, and functionalities for healthcare?
Defining the strategies for article selection is the fourth step of the planning stage. Strategies for article selection are intended to identify those primary studies that provide direct evidence about the research question. To reduce the likelihood of bias, strategies for article selection should be decided during the protocol definition, although they may be refined during the search process (Dabić et al., 2020). During this step, an integrated search strategy was adopted to cover an extensive automated search of different online databases and a manual review of the selected articles.
Embracing an extensive automated search strategy enables the integration of the most fitting online sources (Golder et al., 2014; Rosado-Serrano et al., 2018). For this systematic review, the chosen online databases include IEEE, Emerald, IS Web of Knowledge, and Scopus. Moreover, for every chosen database, appropriate filtering tools were utilized to restrict the research results so that duplication is minimized (McLean and Antony, 2014). For the manual review, the broad manual review method was adopted which involved first reading the title and abstract of each research article (Golder et al., 2014), and then reading the full content of the selected articles to exclude irrelevant articles (Ali et al., 2018a; 2021).
In addition to the extensive automated search and manual review, the backward snowball technique was used to locate articles that were not identified through the previous strategies. This technique employed a reference rundown to identify new articles (Wohlin, 2014). The backward snowballing technique began by analyzing the reference list and removing articles that did not satisfy the key research criteria, such as language, peer-review status, publication year, and type of publication. Then, the duplicate articles were removed and the remaining articles were incorporated into the study. For full details of the review selection criteria, please refer to Table 1.
Review selection criteria
| Criteria | Inclusion | Exclusion | Rationale |
|---|---|---|---|
| Type of publication | Scholarly articles | Reports and any other sources | To ensure that the research retrieves information of academic level sources. |
| Peer-reviewed | Peer-reviewed | Non-peer-reviewed | To ensure the high quality of the used articles. |
| Publication year | Articles published from 2010 to 2021 | Articles that published prior to 2010 | To ensure the validity of the content in any article used in this research review. The pace of technology changes is relatively rapid and the past 10 years is an appropriate time period when the authors can observe the recent trends. |
| Language | English language | Any language other than English | English is the official language of research articles. |
Table 1 presents the eligibility review selection criteria. These criteria help to produce more accurate, objective, and meaningful results as they ensure that the literature considered in the systematic review is relevant to the study. If established and executed correctly, these criteria also reduce the risk of errors and bias. Failing to consistently apply eligibility criteria leads to the inclusion of irrelevant studies in the review, which in turn can lead to inconsistent conclusions.
Execution stageDuring the execution phase, the strategies specified in the planning phase were used to select relevant articles for the study. The main techniques applied in the study are explained below:
- •
Identifying the search terms is an ongoing process that begins with using unique search words from articles that are recognized in the area of study (Hu and Bai, 2014; Paul et al., 2021). The process ends when all the well-known articles are found using the same principles as above. The selected databases in this study have advanced search features, allowing the combination of relevant search words. In this research study, the following keywords were identified: “artificial intelligence OR “machine learning” OR “data processing” AND “healthcare” OR “medical centre” AND “benefit” OR “advantage” OR “feature” AND “challenge” OR “issue” AND “methodologies” AND “functionality”.
- •
While searching the online databases, filtering tools were applied to optimize the research results (Zhang et al., 2014; Moher et al., 2009). In this research, a number of filters, including the research area (IS and healthcare), year of publication (2010 to 2021), document type (journal articles and conference papers), and language (English) were applied.
- •
Once the results were obtained, the articles were manually checked, focusing on the title and abstract, to ensure that they were relevant to the topic of the current study (Pucher, 2013).
- •
All articles obtained from the previous step were thoroughly analyzed for relevant information on this research topic (Shea et al., 2007).
- •
To identify articles that were not attained through the automated research strategy, backward snowball technique (Spanos and Angelis, 2016) was applied.
- •
To confirm that all the articles included in this research were of value, some quality assessment criteria (Begg et al., 1996; Hu and Bai, 2014) was applied. A checklist was prepared to assess whether to include an article. The checklist questions were adopted from the studies conducted by Ali et al. (2018a; 2021) and Sadoughi et al. (2020). They included the following criteria: the discussion on the research objectives is satisfactory, the research problem and questions are clearly stated, the data used are available and well described, the adopted methodology is thoroughly elaborated, and the research results are presented in a comprehensive manner and answer the research questions.
This research used the quality score to investigate whether the results of the primary study were associated with the quality of the study. In addition, the research investigated whether some of the individual quality factors (i.e., sample size, validation method) were associated with the primary study outcome. After selecting the primary relevant studies, it is necessary to assess the quality to minimize the bias and maximize the validity of the systematic review. Therefore, the 180 remaining articles were assessed based on quality criteria. The selected studies were assessed in terms of scientific diligence, reliability, accuracy, and propriety to ensure that research concepts and methods were respected. The results were checked if they were targeted, original, pertinent, and useful for future researchers, experts and enterprises. These criteria were essential to provide valuable and significant contributions to the research community. The selected studies were classified according to their main research aims, methods, contributions, and results. This categorization helps to identify, extract, classify and synthesize data responding to research issues.
The current review study took place from September 15th, 2021, to December 15th, 2021, following the research protocol stated in the planning stage. The initial search based on the defined keywords identified 1,988 articles. After applying all the filter steps as mentioned in this stage, the final 180 research articles met the quality assessment criteria.
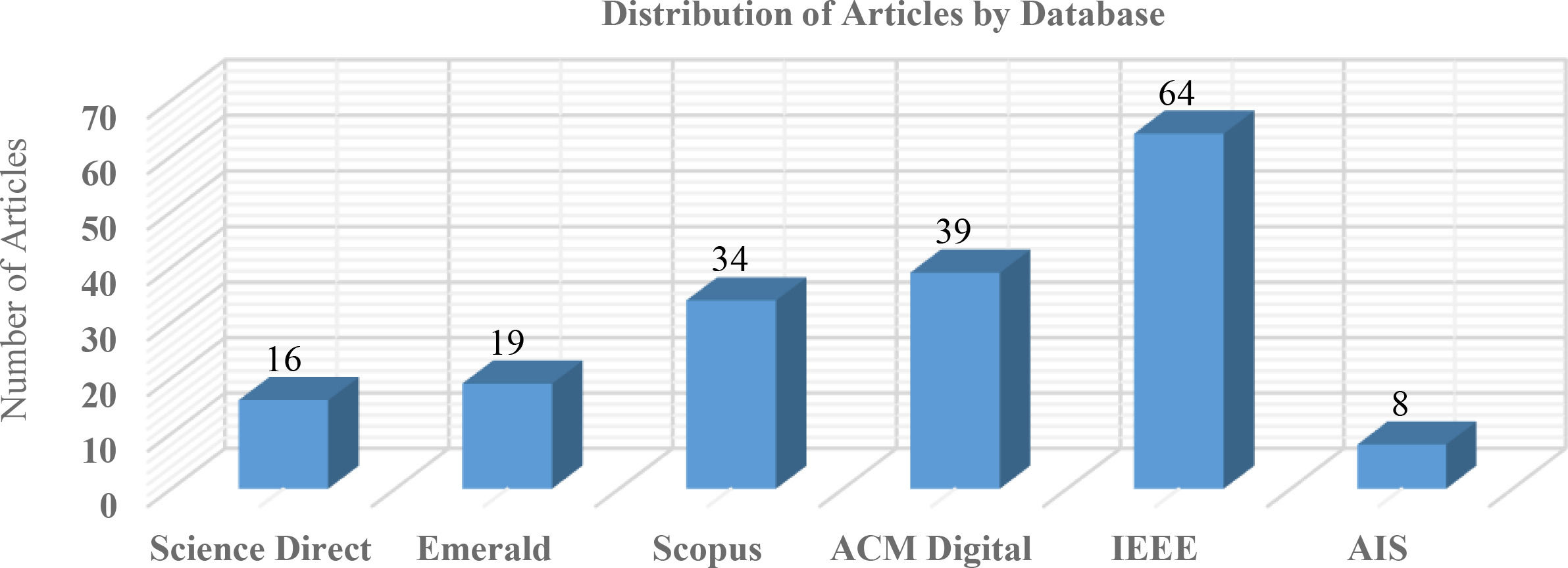
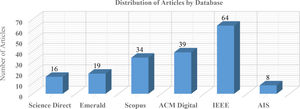
Summarizing stageTable 2 illustrates the final number of articles selected for the present review study. Specifically, based on the initial search process (keywords), 1,988 unique articles were identified. After applying filters, the number of articles was reduced to 936. The researchers then conducted a manual review to identify articles irrelevant to the study. In this process, the researchers focused on both empirical and conceptual articles that were directly related to the topic of this research. As a result, 428 articles were removed, and 508 articles were retained. Next, the full article reading was carried out, where the researchers concentrated on specific criteria, such as objectives, the research questions, the description of the collected data, the methodology applied, the technique used to analyze the data and the presentation of the results. After reading the full articles, another 316 articles were considered insignificant and were removed, which resulted in 192 remaining articles. The backward snowball technique was subsequently applied, which added 42 more articles for a total of 234 articles. Finally, after reviewing based on the quality assessment criteria, 54 articles were removed, finalizing the number of articles for analysis to 180.
Review search results
| An example of a column heading | Automated Search Method | Manual Search Method | Backward Snowball | Final Results | ||
|---|---|---|---|---|---|---|
| 1st Strategy Keywords Results | 2nd Strategy Apply Filter | 3rd Strategy Reading Title and Abstract | 4th Strategy Reading Full Articles | 5th Strategy Backward Snowball Technique | 6th Strategy Quality Assessment | |
| Science Direct | 346 | 149 | 68 | 19 | 24 | 16 |
| Emerald | 239 | 154 | 84 | 22 | 27 | 19 |
| Scopus | 418 | 196 | 92 | 39 | 45 | 34 |
| ACM Digital | 332 | 116 | 77 | 42 | 51 | 39 |
| IEEE | 516 | 238 | 141 | 58 | 69 | 64 |
| AIS | 137 | 83 | 46 | 12 | 18 | 8 |
| Total | 1988 | 936 | 508 | 192 | 234 | 180 |
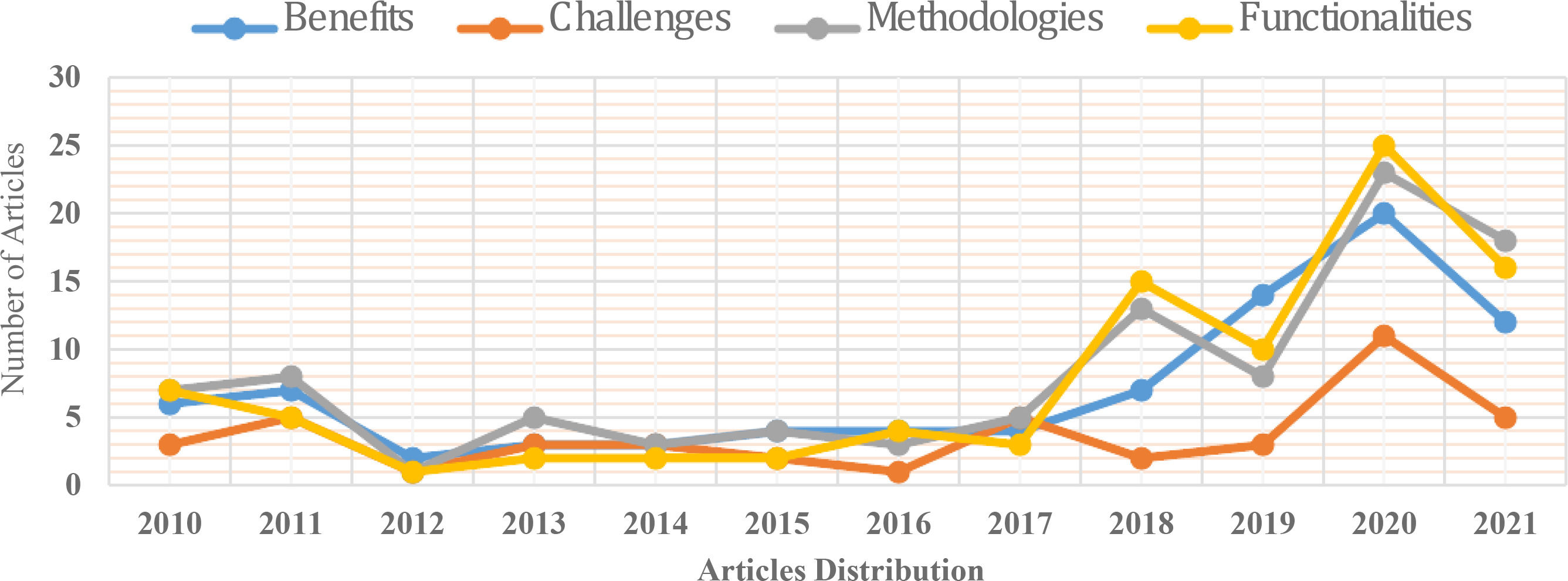
The earliest publications on how AI enabled healthcare sector data were from 2010 (see Fig. 3). The greatest number of articles, 44, was published in 2020, and the lowest number of articles, 4, was published in 2012. Most of the articles were published between 2018 and 2021, thus signifying the recent interest in this research area.
Distribution of articles by databaseFig. 4 illustrates the distribution of the selected articles by database source. 64 articles were identified in the IEEE database, followed by 39 articles from the ACM Digital database, 34 articles from the Scopus database, 19 articles from the Emerald database, 16 articles from the Science Direct database, and only 8 articles from the AIS e-library (see Fig. 4).
Distribution of articles according to the classification frameworkThe research topic is organized into four dimensions: benefits, challenges, methodologies, and functionalities. Fig. 4 displays the quantity of articles published each year in each dimension. Thus, the aggregate number of articles published under benefits is (n=86); challenges (n=44); methodologies (n=98); and functionalities (n=92). The majority of the articles investigating how AI enabled the healthcare sector are related to benefits, methodologies, and functionalities (Fig. 5).
Nevertheless, the number of studies focusing on AI challenges has been the lowest in the past ten years. The benefits of using AI within organizations is another topic of interest to many researchers and is the third most studied topic as per this classification framework. The method that organizations used to adopt and use AI was the second most studied topic as per the classification framework. Meanwhile, functionalities that AI provides to improve the performance of organizations have gained the most significant research attention in the past decade.
Research classification frameworkThe findings of a detailed review of AI and healthcare related articles were put forward and examined. The classification framework was applied by considering the four dimensions: AI-enabled healthcare benefits, challenges, methodologies, and functionalities. For more details, see Table 3, 4, 5, and 6.
AI-enabled healthcare benefits
AI-enabled healthcare challenges
AI-enabled healthcare methodology
AI-enabled healthcare functionalities
Table 3 illustrates the classification framework related to AI-enabled healthcare benefits and comprises specific categories for this dimension, such as benefits to individuals, organizations, and sectors. Additionally, in each category, relevant factors were identified that defined the category.
Table 4 demonstrates the classification framework related to AI-enabled healthcare challenges and involves specific categories for this dimension, such as challenges related to data integration, privacy and legal issues, and patient safety. Furthermore, in each category, relevant factors were identified that defined the category.
Table 5 shows the classification framework related to AI-enabled healthcare methodologies and contains specific categories for this dimension, such as multimedia processing and textual data processing. In addition, in each category, relevant factors were identified that defined the category.
Table 6 shows the classification framework related to AI-enabled healthcare functionalities and covers specific categories for this dimension, such as functionalities related to the organization, patient, and sector. Additionally, in each category, relevant factors were identified that defined the category.
Research discussionDimension 1: benefitsThis dimension is related to the advantages that organizations can achieve from using AI. It includes benefits to people that consist of automated decision-making; patient monitoring, particularly elderly patient monitoring; early diagnosis; and process simplification (Sasubilli, 2020; Deebak, 2021). It also includes benefits to organizations that consist of workflow assistance, improvement of performance, reduction of cost, and fraud detection (Zhou, 2020; Bernardini, 2021). The final category of this dimension is benefits to the sector that consist of saving time, reducing resource consumption, and providing professional training, data sharing, and data availability (Yu, 2021; Kaur, 2021). Next is an in-depth description of each category.
Benefits to individualsAI has several benefits to people, including automated decision-making (Sqalli and Al-Thani, 2019; Minz and Mahobiya, 2017; Ribbens et al., 2019; Seeböck et al., 2019; Strachna and Asan, 2020), patient monitoring, including elderly patient monitoring (Wu et al., 2019; Rahman et al., 2020; Comito et al., 2020; Khan et al., 2018; Wong et al.,2020; Mary et al.,2020), early diagnosis (Sasubilli et al.,2020; Jahan and Tripathi, 2021; Ladgham, 2013; Ribbens et al., 2019; Sakkos et al., 2021; Razaak et al.,2014) and process simplification (McGregor et al.,2020; Sqalli and Al-Thani, 2019; Deng et al.,2019).
The benefits to individuals are primarily derived from their collected medical data that are often heterogeneous, complex and not normalized. In addition, they are often large in volume and come in different formats. While this represents a great challenge for medical care practitioners, AI can be very effective in analyzing these types of big data and coming up with innovative solutions that are highly relevant and meaningful for health practitioners, ultimately benefiting the patients in their care, diagnosis and treatment options. Generally speaking, diagnosis- and treatment-related decisions consume both time and effort. AI provides a convenient solution to overcome this challenge, as it has great potential in generating automatic inferences with limited or no human intervention. Some studies even argue that AI can outperform humans in some medical situations related to radiology, cardiology and tumor detection (Kaur et al., 2021; Miller and Brown, 2018).
Sqalli and Al-Thani (2019) address the case of chronic diseases, stating that chronic diseases in particular are exhausting to the healthcare sector in terms of effort and cost because patients frequently visit their healthcare providers because they need continuous care. Some of these visits are unnecessary and cause a waste of time and resources. The authors find that health coaching, which is a healthcare strategy that consists of educating patients to improve their health-related behaviors, also helps in reducing the expenses of chronic patients. They propose a model that integrates health coaching with AI to help patients manage their chronic diseases more effectively by minimizing the number of unnecessary visits. Similar to the system suggested by Murray et al. (2019), the system consists of sensors that capture biometric data, AI models that generate insights about medical conditions and visual analytics tools that display relevant data in graphical and textual formats.
Benefit to organizationOrganizations use AI applications and IT tools to reduce costs (Kaur et al., 2021; Sqalli and Al-Thani, 2019; Zhou et al., 2020; Roa et al., 2011), detect fraud (Dhieb et al.,2020; Rawte and Anuradha, 2015; Capelleveen et al.,2013), improve performance (Ladgham et al.,2013; Minz and Mahobiya, 2017; Maduri et al., 2020), and provide workflow assistance (Bernardini et al., 2021; Wu et al., 2019; Deng et al., 2019; Daltayanni et al.,2012).
For instance, Murray et al. (2019) highlight the difficulty of automatically extracting knowledge using clinical information systems, mainly due to the limited level of data normalization and integration. The authors introduce an artificial AI-empowered network (AI-KEN) to overcome these challenges. It consists of a network based on an AI system that automatically generates clinical notes, using predictive text options to reach normalization, over clinicians’ original notes to ensure data normalization and integration from multiple sources. AI-KEN operates using three main steps. First, it normalizes data using declared transformation rules. Then, it transforms data with validated ontologies to integrate them. Finally, it uses a data analytics model to extract valuable knowledge from the integrated data. Manifold research has introduced AI as a solution for similar complexities to reduce the consumption of resources in the healthcare sector (Sqalli and Al-Thani, 2019; Kaur et al., 2021; Zhou et al., 2020; Roa et al., 2011). Bohr and Memarzadeh state that implementing AI in healthcare can reduce the annual US healthcare costs by USD 150 billion in 2026 (Bohr and Memarzadeh, 2020). This reduction may be applied to other countries but there are limited quantitative evaluation data given the recency of the impact of AI in the healthcare sector.
AI can also assist the healthcare sector by detecting fraudulent claims. Health insurance fraud is a serious challenge in the insurance sector. According to the Federal Bureau of Investigation (FBI), insurance fraud causes an annual $80 billion loss in the USA (Austin, 2018). Moreover, 21% of bodily injury and 18% of personal injury claims that have been sealed with a full refund are fraudulent (Corum, 2017). Fraud detection becomes more challenging to detect with the continuous increase in data volume. Several researchers have attempted to integrate AI into the health insurance sector to detect fraudulent claims (Dhieb et al., 2020; Rawte and Anuradha, 2015; Capelleveen et al., 2013; Gangopadhyay and Chen, 2016; Anbarasi and Dhivya, 2017; Thorntonl, 2015; Ragde et al., 2016; Yang and Hwang, 2014; Bagde and Chaudhari, 2016). Rawte and Anuradha (2015) recommend a hybrid solution that combines clustering and classification to detect duplicated insurance claims. The authors mention that classification methods and clustering methods alone are not sufficient to detect duplicated claims. To overcome this challenge, the authors propose a two-step model. The first step is the claim clustering step performed using the evolving clustering method (ECM). The second step is based on the SVM algorithm classification step that uses the output of the first step as input. Ibrahim (2022) proposed AI based electronic health data recording system in short- and long-term hospitalization.
Dhieb et al. (2020) suggest an insurance system framework that uses extreme gradient boosting (XGBoost) to reduce human interaction, secure insurance activities, alert and inform risky customers, detect fraudulent claims, and reduce monetary loss for the insurance sector. After presenting the blockchain-based framework to enable secure transactions and data sharing among different interacting agents within the insurance network, they propose to employ the machine learning algorithm for the aforementioned insurance services and compare its performance with that of other state-of-the-art algorithms. The results reveal that when applied to an auto insurance dataset, XGboost achieved high performance gains compared to other existing learning algorithms. These are some examples of how recent AI advancements bring benefits to the organizations adopting the AI systems.
Benefit to the sectorThe entire healthcare sector that comprises the hospitals, insurance companies and government agencies also benefit from AI technologies as a whole. Since IT helps to collect, process, share and store patient data (Jumelle et al., 2014; Antoniou et al., 2018; Jaiman and Urovi, 2020; Bennett et al., 2011), building on this data AI can provide support towards professional training (Deist et al., 2020; Paranjape et al., 2019; Torner et al., 2019; Gupta et al., 2019), and such applications can save time (Sasubilli et al., 2020; Strachna and Asan, 2020; McGregor et al., 2020) and reduce resource consumption (Dhieb et al., 2020; Kaur et al., 2021; Kaur et al., 2021).
Extending the application of AI solutions to the field of healthcare brings countless advantages to this crucial field. It helps minimize resource consumption and reduce treatment expenses and time (Bohr and Memarzadeh, 2020). In addition, it accelerates the diagnosis time and thus the decision-making process, which has a major impact on treatment strategies and outcomes and might be lifesaving in critical situations. Data sharing in the health sector is important for individual well-being when followed by different doctors in different health institutions. It is also important for scientific research and progress. However, accessing medical data is often difficult due to regulatory and privacy challenges, according to Deist et al. (2020), who recommend the personal health train (PHT) system, which provides a privacy-by-design infrastructure connecting data sources while promoting the application of machine learning techniques to distributed data. Paranjape et al. (2019) encourage the use of AI for educational purposes and introduce a framework that includes AI into the medical education curriculum. Holistically speaking, AI can be beneficial across the entire healthcare sector.
Dimension 2: challengesA number of challenges may deter organizations from using AI. These include challenges related to the data, which consist of data digitization and consolidation and data availability (Murray, 2019; Dhieb, 2020). They also include challenges related to privacy/legal issues, which consist of privacy issues, legal issues, and government regulations (Zerka, 2020; Shaban-Nejad, 2021). The final category of this dimension is challenges related to the patient that consist of decision errors, treatment errors, data errors, and human interventions (Tsang, 2020; Madanan, 2021). Next is an in-depth description of each category.
Challenges related to privacy/legal issuesThere are obvious privacy issues related to accessing, editing, sharing and using patient data. Cloud computing and AI are often commonly used in different types of applications in the health sector. These systems collect, process, store, monitor and share health data (Sasubilli et al., 2020; Zerka et al., 2020; Peters et al., 2020; Jumelle et al., 2014). Despite the advantages of these systems, there are also some challenges such as security issues, privacy implications, cybersecurity and ethical issues. Hospitals and government agencies usually provide ethical procedures for collecting and sharing data. Permission is required from a government-approved authority to collect and use data, even for research purposes (Wang et al., 2020; Zhou et al., 2021; Bouguettaya et al., 2016). Other ethical issues associated with AI in the healthcare and broader sectors are inequality, unemployment, humanity, commitment to cause, regulatory approaches, behavioral biases, population biases and linking biases (Jameel et al., 2020). In order to reduce ethical issues in AI applications in the health area, there are studies on minimizing negative side effects, reward hacking, safe exploration and robustness (Jameel et al., 2020; Bryson et al., 2018; Zerka et al., 2020; Esmaeilzadeh et al., 2020). Some machine learning algorithms are used for the early prediction, treatment and diagnosis of diseases, and they can make decisions or support doctors’ decisions. Governments have expressed their concerns about these automated processes with respect to protecting patients’ rights. Such concerns have led to several regulations in data collection, processing, technology usage and quality of such data and collection and analysis methodologies. In addition, researchers who are working in the healthcare domain should have a careful focus on data quality, testing of data and documentation (Jumelle et al., 2014; Shaban-Nejad et al., 2021; Esmaeilzadeh et al., 2020) before AI applications can use them.
Challenges related to data integrationSome AI methods require a large volume of data to process. It is sometimes difficult to collect data, especially patient data, because of ethical implications of such data. The application of some classification and clustering algorithms on a very limited amount of data may yield very good accuracy; however, it might not be realistic and applicable (Patii and Iyer, 2017; Murray et al., 2019; Bennett et al., 2011). The collected data require preprocessing to be used in AI techniques. In particular, text data require considerable natural language processing before use. Different types of data, such as text, numeric, image and video, sometimes must be integrated using the same algorithm, which is one of the most difficult challenges in medical data processing (Patii and Iyer, 2017; Murray et al., 2019; Bennett et al., 2011). Medical data can be collected from various sources and formats, such as medical images, 3D video sequences, photographs, and numeric data. Collecting clean, robust and efficient data is a challenge in healthcare data analysis.
Challenges related to patient safetyMachine learning, natural language processing and expert systems use medical data as an input to process and create models to support medical decisions based on health systems. Most of the applications of AI in health systems are related to diagnosis. False decisions in automated diagnosis may have very harmful results. Collected data from hospitals are sometimes not of sufficient quality or simply inaccurate. Data errors are among the top challenges in medical data processing via AI (Nikolaev et al., 2021; Ling et al., 2013; Hasan et al., 2017; Goldberg et al., 2010). Another challenge is decision errors made by machine learning algorithms. Sometimes the applied algorithm is not suitable for the given data, or the data are not sufficiently reliable to be used in classification algorithms such as neural networks, decision trees and Bayesian networks. Several studies have demonstrated possible decision-making problems in the health domain and their solutions (Madanan et al., 2021; Aljaaf et al., 2015; Srivastava and Rossi, 2019; Poletti et al., 2013; Kusano et al., 2017). Currently, a considerable number of AI and IoT devices and software are used in the healthcare sector. However, not all of them are automated: doctors make the final decision, and this interplay between the healthcare practitioners and AI models may end up with false diagnoses and treatment results (Sqalli and Al-Thani, 2019; Lim and Thuemmler, 2015; Mohr et al., 2011; Tsang et al., 2020).
Dimension 3: methodologyMethodology, in this context of application of AI in the healthcare sector, is the process that healthcare organizations adopt to use AI. It includes data processing, machine learning, and expert systems (Oktay, 2018; Saxena, 2019; Katarya, 2020; Srayya, 2021). Medical data can be categorized as images, numeric data and text data in AI applications. Image processing, video processing and virtual reality and games are commonly used techniques in image data analysis (Jahan and Tripathi, 2021; Broehan et al., 2010; Yanhong et al., 2014). On the other hand, numeric data, extracted features from images and text data are also used in machine learning, expert systems and data preprocessing. Next is an in-depth description of each category.
Methodology related to textual data processingThere are several data types in AI applications in the healthcare sector, such as text, numeric data, images, videos and audio. Most of the time, data collected from patients are raw data and need processing before applying machine learning or similar algorithms. For example, quantitative electroencephalography (QEEG) is a signal type that is preprocessed, and several features are extracted for use in the high-level learning process (Ciprian et al., 2020). The quality of ultrasound video sequences is another important parameter of automated early diagnosis. Video encoding and linear regression methods increase the quality of the video (Panayides et al., 2018).
Machine learning algorithms can be used to understand personal health situations. Random forest and other rule-based algorithms are used in analyzing health patterns (Sasubilli et al., 2020). Truth maintenance system (TMS) algorithms predict features from large datasets and apply classification. TMS algorithms give more accurate results than other algorithms in human health pattern recognition. Several algorithms have also been developed for the early diagnosis and treatment of kidney disease (Bernardini et al., 2021). Machine learning algorithms provide monitoring and analysis of the estimated glomerular filtration rate (eGFR), which is an important parameter in the treatment of kidney disease. Another important data application in medicine is magnetic resonance imaging (MRI), which can be applied to image processing, computer vision and machine learning techniques for diagnosis (Jahan & Tripathi, 2021; Ladgham et al., 2013; Minz and Mahobiya, 2017; Nikolaev et al., 2021; Ribbens et al., 2014; Zhong et al., 2020; Ling et al., 2013; Amrane et al., 2018). Lung and breast cancers are two of the most frequent cancers that cause death. Eight percent of women are faced with breast cancer during their life. Machine learning algorithms have a very high success ratio for automated breast cancer detection (Amrane et al., 2018). A naïve Bayes classifier (NBC) and k-nearest neighbor (KNN) algorithm are used to classify the breast as either normal or abnormal. KNN gives a very high accuracy of 97.51%.
Likewise, Ribbens et al. (2014) proposed a new unsupervised segmentation and classification approach for brain MRI images. First, MRI was applied to segmentation to retrieve the feature vector. If clinical experts are experienced in record taking, supervised training can be applied; otherwise, unsupervised training can be applied to classify the brain as normal or requiring further investigation. Probabilistic classification methods yield very promising results in brain MRI images. However, it is difficult to obtain real-time feedback for asthma and eHealth management. Several well-known algorithms, especially NBC and logistic regression supervised classification algorithms, have been developed for early warning systems (Tsang et al., 2020). Yu (2022) and Causey (2022) proposed several object detections, segmentation and tracking methods to recognize tumors in medical images. Results from the use of AI are very promising especially with CT images.
Machine learning algorithms and the Internet of Things (IoT) were also used in several applications of the prediction and data collection of COVID-19 (Dharani and Krishnan, 2021; Hossen and Armoker, 2020; Gazzah and Bencharef, 2020; Elbasi et al., 2021). Probabilistic-based machine learning algorithms such as the Bayesian network and NBC were used to predict the possibility of a patient having COVID-19 (Dharani and Krishnan, 2021). Artificial neural network algorithms produce very promising results in the classification of patient data as virus or no virus. The IoT collects data from crowds using several sensors, such as temperature, distance and the use of masks. Collected data are used as an input to classification algorithms, which provide safe or unsafe crowds in indoor and outdoor public areas.
Expert system techniques also have several applications in health classification, decision-making and patient support systems (Sqalli and Al-Thani, 2019; Yu and Zhou, 2021; Chen et al., 2018; Bernardini et al., 2021; Gandhi et al., 2019; Reddy and Chavan, 2021; Albayrak et al., 2018). The management of chronic diseases is becoming important because of increases in patient visits. These patients need more frequent doctor and laboratory visits, which are time-consuming and costly. Sqalli and Al-Thani (2019) proposed expert system-based models to manage their decision support system. This automated health coaching system collects patient data, performs an analysis, retrieves doctor consultations and gives feedback to patients.
Methodology related to multimedia processingMedical image processing uses several types of images of the human body for early diagnosis and treatment. Computed tomography (CT) and magnetic resonance imaging (MRI) are frequently used in medical image processing research, and several applications already exist in the sector. Doctors, engineers and radiologists work together to analyze medical imaging (Nikolaev et al., 2021; Zhong et al., 2020; Alamri et al., 2010). Medical image processing takes images as an input and applies image processing techniques to understand images, such as resizing, cropping, rotation and editing. Nikolaev et al. (2021) developed a new algorithm using MRI images to diagnose breast cancer. Data preprocessing, segmentation, feature extraction and classification represent the sequence of methods used in breast cancer detection using AI techniques (Zhou et al., 2018; Harinishree et al., 2021; Amrane et al., 2021; Gayathri and Sumathi, 2021; Charan et al., 2018; Osareh and Shadgar, 2018). In addition to image processing, video processing is used in the health sector. Video cameras capture frames from inside the human body to collect more information, which means that in the health sector and AI, early and right decisions can be made. Video capturing also helps doctors in surgery. Sometimes a 2D image is not sufficient to make the right decision. In that case, 3D images can be used, such as for the brain or other organs (Broehan et al., 2010; Razaak et al., 2014; Wu et al., 2013; Panayides et al., 2015; Poletti et al., 2013). The IoT and video can be used for patients, particularly elderly patients being monitored from their home. The IoT collects data, such as temperature, blood rate and heart rate, using wearable technology. Video cameras in a room can be static or moving and provide real-time images and data for analysis. Smart cameras supported by IoT sensors can send an SMS or alarm in the case of any abnormal patient situation. Ahmed et al. (2021) proposed a monitoring system that uses deep learning in the classification of patient situations using IoT and video data. The proposed algorithm has achieved greater than 94% accuracy.
Virtual reality (VR) and game technologies are also commonly used in the health sector. They can be used in the training of doctors and nurses, especially for surgery training. Before performing a procedure, surgeons can practice it in a controlled, safe, and entirely digital environment using virtual reality. Physical therapy, relaxing patients, monitoring patients, disease awareness and medical marketing are other application areas of VR and games in the health sector (Yanhong et al., 2014; Shim et al., 2020; Zhou et al., 2021; Hassan et al., 2016; Li et al., 2018; Burdea et al., 2020). Using VR, doctors can undertake high-quality surgery training. A 360-degree angle from several cameras and an additional model create efficient surgery training for doctors and other health sector workers. This approach can be used in robotic surgery, patient consultation, mental health therapy and pain management. Serious games are computer-based games that can be used in the health sector to educate sector workers and for treatment purposes for some diseases, such as Parkinson's disease (Kusano et al., 2017; Torner et al., 2019; Gupta et al., 2019; Tsai et al., 2011; Cecil and Pirela-Cruz, 2013). A serious game helps patients significantly enhance their quality of life by allowing them to receive treatment and physical therapy from their own home.
Dimension 4: functionalitiesFunctionalities, in the context of this study, refer to the features that healthcare organizations receive through the adoption and use of AI. They include functionalities to clinics that consist of clinical decision-making, up-to-date information, resource allocation, and information sharing (Mary, 2020; Jahan, 2021). It also includes functionalities to patients that support their diagnosis, treatment, consultation, and health monitoring (Tsang, 2020; Dharani, 2021). The final category of this dimension is functionalities related to the sector that consist of IoT data collection, medical imaging, research development, and remote surgery (Ribbens, 2019; Noothout, 2020; Zhou, 2021; Patel et al., 2022). Next is an in-depth description of each category.
Functionalities for the clinicAI technologies have several functionalities in the health sector, such as for clinics, patients and sector. Clinics can use technologies in decision-making (Jahan and Tripathi, 2021; Ladgham et al., 2013; Minz and Mahobiya, 2017), up-to-date information collection (Zhou et al., 2020; Mary et al., 2020; Rong et al., 2020) and information sharing (Wu et al., 2019; Gandhi et al., 2019; Zheng et al., 2018; Jaiman and Urovi, 2020).
In addition, machine learning improves the decision-making process by providing a solution for health-care practitioners and researchers to extract hidden knowledge from the huge amount of available data that cannot be discovered if relying on human effort only. A considerable amount of research has attempted to exploit machine learning to improve and automate the decision-making process in the health-care field (Thakkar et al., 2010; Moein et al., 2010; Nimmagadda et al., 2011; FengGuo et al., 2010; Bennett et al., 2011; Sqalli and Al-Thani, 2019; Minz and Mahobiya, 2017; Ribbens et al., 2019; Seeböck et al., 2019; Strachna and Asan, 2020; McGregor et al., 2020; Comito et al., 2020; Albu, 2017).
Functionalities for the patientPatients are the main concern of health activities. AI technologies can be used for various applications from making appointments to patient monitoring. AI and other information technologies mainly have functionalities in patient diagnosis (Bernardini et al., 2021; Jahan and Tripathi, 2021; Ladgham et al., 2013; Patii and Iyer, 2017; Yang et al., 2018), treatment (Ciprian et al., 2020; Minz and Mahobiya, 2017; Zhou et al., 2021; Hassan et al., 2016), consultation (Sqalli and Al-Thani, 2019; Ladgham et al., 2013; Yu and Zhou, 2021), and health monitoring (Rahman et al., 2020; Maduri et al., 2020; Sakkos et al., 2021).
Many patients are in a healthy state where they need continuous monitoring. They can be either people who are in healthy state or where they cannot take care of themselves or senior patients who need continuous observation due to health or age-related concerns. This type of health monitoring consumes time, human resources and money, which is challenging but they cannot be avoided for patient safety and well-being when following traditional patient monitoring strategies. An innovative solution consists of remote patient monitoring. “Remote patient monitoring is an emerging field of healthcare, which concerns the management of health/illness with the goal of treating or diagnosing illness using information technology and telecommunication tools” (Jeddi and Bohr, 2020). Remote patient monitoring brings many advantages to both patients and hospitals. Tele-health systems are also getting important especially with the COVID-19 pandemic. Jiang (2022) developed a wearable tele-heath system to monitor especially patient and elderly people.
AI reduces hospital loads, resource consumption, hospital occupancy, and wasted time and effort in unnecessary medical intervention by minimizing the number of false alerts and relieving practitioners’ burdens to free their time for more important tasks. In addition, remote patient monitoring brings many benefits for patients, particularly elderly patients. First, it helps them avoid wasting time, effort and money by minimizing unnecessary visits to the hospital. Second, it plays a major role in safety and well-being by sending lifesaving alerts when the situation of the patient requires medical intervention. This is even more efficient when the patient is in weak health and cannot call for help. A great deal of research has been performed to implement and test health monitoring systems that combine biomedical data, collection devices and machine learning (Khan et al., 2020; Maduri et al., 2020; Chauhan et al., 2021; Ahmed et al., 2021). For example, Khan et al. (2020) encourage the inclusion of AI in medical practices to overcome the continuous increase in the number of patients. They state that including AI in medical practice enables doctors to better manage the non-stop biomedical information stream. The authors introduce a prototype that combines an ECG patch and machine learning to monitor patients. The EGC devices collect real-time biomedical data to check the health state of an individual's heart anywhere and anytime. The prototype processes the collected data using an algorithm that exploits multiple machine-learning techniques, including decision trees, regression trees, neural networks, deep learning and support vector machines. The output of these techniques is generated over ensemble methods. This prototype has been tested on adult patients at the Emory University Hospital (EUH). The authors claim that the model succeeded in eliminating unnecessary repetitive tasks, which provide more time for effective treatment tasks and reduce money and effort waste.
Functionalities for the sectorMultiple healthcare departments and sectors can use AI by following a multi-disciplinary approach in data collection using the IoT (Wu et al., 2019; Rahman et al., 2020; Maduri et al., 2020; Patii and Iyer, 2017), medical image processing (Jahan and Tripathi, 2021; Ladgham et al., 2013; Minz and Mahobiya, 2017), research development (Wu et al., 2013; Zhang et al., 2020; Azghadi et al., 2020) and remote surgery (Yanhong et al., 2014; Shim et al., 2020; Zhou et al., 2021; Hassan et al., 2016). A substantial quantity of research has attempted to further extend the medical field by both AI and the IoT. The latter is useful in connecting the infrastructure of the internet and sensor networks, which generate a useful stream of data that can be analyzed using AI models (Maduri et al., 2020; Chauhan et al., 2021; Ahmed et al., 2021).
Diagnosis is a crucial step to achieve successful treatment. Nevertheless, it is very challenging for many diseases, especially in their early stages. Nevertheless, early diagnosis can be a game changer for multiple diseases, as it can help patients, doctors and even hospitals countless effort and resources. For example, patients at the stage of melanomas of a thickness below 1 millimeter have a 95% 5-year survival rate. However, patients at the stage of melanomas of a thickness over 4 mm have only a 45% 5-year survival rate (Balch et al., 2001). The use of AI in measuring and detecting these physical conditions may prove to be the matter of life or death in these cases.
A considerable amount of research has investigated the potential of AI in early diagnosis (Gayathri et al., 2015; Katarya and Srinivas, 2020; Chauhan et al., 2021; Harinishree et al., 2021; Amrane et al., 2018; Charan et al., 2018). Cancer is one illness where early diagnosis may significantly alter the outcome. Early diagnosis of cancer can substantially increase the chance of survival by increasing the chances of treatment success. This can be even more beneficial when spotting cancer before it has the chance to spread.
Gayathri et al. (2015) suggested a model based on fuzzy logic that detects the risk of breast cancer. This model attempts to reduce the duration of diagnosis by implementing linear discriminant analysis (LDA) for feature reduction. The model performs training using a fuzzy inference method called the Mamdani fuzzy inference model. The authors claim that the system achieves an accuracy of 93%. Katarya and Srinivas (2020) approached the early diagnosis of heart diseases using AI. The authors performed a comparative study between AI algorithms using the existing Cleveland database. They found that decision tree and naïve Bayes outperform other models. The authors recommend using search algorithms for feature selection to achieve good accuracy. Murray et al. (2019) consider machine learning solutions to solve the semantic challenges facing health-care practitioners.
The findings outlined from the classification framework is illustrated in Fig. 6.
Research implicationsEmpirical studies that consider AI in healthcare are still emerging compared to the rapid industry adoption of AI solutions in healthcare. Numerous IT vendors have started to deliver cutting-edge AI solutions, which is the next generation of health informatics/digital health solutions being adopted in the healthcare sector. The use of digital tools in medical as well as organizational processes of the healthcare sector is not new; however, the inclusion of AI features is a relatively recent phenomenon.
Implications to theoryStudies on the use of AI in the healthcare sector should adopt cross-theory approach covering the individual (patient and medical staff perspective), organizational (hospital & teams) and industry (healthcare sector) level units of analyses. The benefits of AI to the healthcare sector spans across from an individual level to patients and medical staff, including doctors and nurses, to the organizational and sectoral levels for hospital administrators. AI continues to outperform humans in terms of accuracy, efficiency and timely execution of medical and related administrative processes and these developments may have significant impact on future direction of not only the healthcare sector but for humanity. In terms of patients, the benefits are related to clinical safety, patient experience and holistic care provision that can be studied from a clinical or psychological perspective. For medical practitioners, the key benefit of AI is advancing further studies on medical treatment from faster and accurate diagnosis to execution of robot-supported surgeries. In short, AI is reimagining modern healthcare services where machines can predict complex diagnostic issues and learn and adapt to execute increasingly onerous medical tasks. Research on the decision-making support to individuals and organizations using AI aligns with the decision theory that is predominantly used in expert systems and AI (Horvitz et al., 1988).
The challenges of AI in the healthcare sector are related to the real and perceived data integrity matters and the resultant patient safety and privacy issues. Healthcare is complex, and all patient circumstances and scenarios may have a multitude of environmental and situational factors that are either not recorded in the digital format or too complex to be coded in healthcare data systems. In the absence of these critical data points, the AI solutions may limit the real-life validity and application in diagnosis and treatment options. One might argue that AI can assist medical staff and save time and effort in doing their work, but this may backfire when AI that works as a ‘black-box’ solution becomes harder for healthcare workers to understand and interact with. Because healthcare staff must understand how and why a particular decision is made in terms of diagnosis and treatment choices, it is unlikely that AI can provide such rationale, as the AI outcomes are modeled based on existing data and how its training modules are configured. It is unlikely that medical professionals can simply accept a solution because it is explained by AI solutions that lack responsibility and legal identity. This relates to how AI continue to evolve based on mathematical theories on algorithmic advancements for probabilistic machine learning and associated techniques (Ghahramani, 2015) and how these algorithms can be built to support transparent data integration techniques that promote privacy and security of patient data.
Furthermore, the AI functionalities can be attributed to features for the patients, medical staff, medical organizations and the entire healthcare sector. AI patient benefits map directly to the relevant AI functionalities in the categories of diagnosis, treatment, consultation and health monitoring for self-management of chronic conditions. Likewise, in terms of the functionalities supporting medical organizations, AI optimizes medical processes that lead to clinical decision-making and research of the impact of AI on decision making continue to evolve in the healthcare sector (Lysaght et al., 2019). Data-driven decision-making of AI can also be attributed to information availability and sharing features that are critical for AI systems. The most significant functionalities of AI that support the healthcare sector in general are in the areas of medical imaging and robotic surgery. These areas are new innovations in the healthcare sector, and AI supports innovation in terms of enhanced research and development capacity (Gumbs et al., 2021). Another area of AI functionality is autonomous IoT data collection, which will promote the capturing of significant data points, thereby improving the validity and trust of AI-driven decision outcomes in healthcare systems (Mansour et al., 2021).
Implications to practiceAI supports the healthcare sector by reducing the cost of clinical trials in terms of wasted human hours when developing new medicines. Beyond the medical factors of clinical safety, diagnosis and treatment options, AI solutions can boost patient experience by optimizing patient interaction workflows that are complicated by patient co-morbidities and ailments, insurance coverage matters and other environmental and situational conditions. At the organizational level, AI can optimize healthcare data management by intelligently connecting the most important data points, thereby supporting accurate diagnosis, timely treatment and preventative measures that improve health outcomes.
In terms of practical challenges of AI use in the healthcare sector, data integrity issues exist due to the lack of testing of AI in diagnostic errors. Similarly, the confidentiality, privacy and complexity of medical data in collection and analysis are also compounded by ethical constraints. Configuring a single AI training model may require the processing of thousands of images, which could be time consuming and error prone even with today's automation capabilities. Because privacy-sensitive and complex data types are primary features of medical data, ongoing risks of data breaches and cyberattacks concern the healthcare sector.
Likewise, in terms of methodologies adopted by AI solutions in the health care sector, AI systems are based on modules trained on large and complex data that require high-quality processing and automation systems. Textual data points (notes and reports) are relatively easier to annotate; however, medical data comprise complex data types, including medical images and videos, which require expert review and interpretation. Processing of complex types of data (multimedia) can be a barrier for AI systems as it impedes not only the responsiveness of the AI systems but also the accuracy of the data analysis, thereby potentially compromising patient safety.
Research limitations and future directionsThis research has some limitations. First, there was a lack of specific AI operations that could not be accessed, as academic papers often lack details of the ways AI functions given that these functionalities are largely proprietary in nature. Second, despite the deployment of a thorough search strategy, some studies on AI in healthcare were not included, such as gray literature and reports that were not published in the selected databases that were reviewed.
ConclusionAI technologies, including machine learning, IoT, algorithms, and robots, are utilized to monitor, diagnose, treat and measure risks and benefits, particularly in the healthcare industry. To enhance procedures and facilitate the administration of medicine, healthcare organizations rely heavily on medical data and analytics. This systematic review includes a discussion of the benefits, challenges, methodologies, and functionalities directly related to AI in the healthcare sector. The findings of this review show that AI and its subareas provide benefits to individuals, organizations and health sectors. There are some challenges, such as data integration, privacy issues, legal issues and patient safety. Machine learning, image processing, data mining, expert systems, virtual reality, computer vision and data science are some of the most frequently used AI methodologies in the health sector based on this systematic review. There are several functionalities of AI in health areas, such as diagnosis, treatment, information sharing, security, consultation, monitoring, data collection and remote surgery. This review study offers an understanding of current AI research and its real-world implementation in the healthcare sector.
This review study presented implications for practice as guidance for future studies as well as for decision-makers in the healthcare sector. It is essential to discover whether the benefits of AI outweigh the challenges related to its use in the healthcare sector. According to the literature analyzed in this review, there is sufficient evidence to believe that AI can bring significant benefits to the healthcare sector. However, the challenges related to real and perceived data integrity and the resultant patient safety and privacy issues of using AI in healthcare must be carefully evaluated, especially due to the strict regulations that govern the healthcare sector. As a result, many organizations are working to improve and adapt policies to secure patient data to promote confidentiality.