Información de la revista
Vol. 154. Núm. 3.
Páginas 110-111 (febrero 2020)
Compartir
Descargar PDF
Más opciones de artículo
Vol. 154. Núm. 3.
Páginas 110-111 (febrero 2020)
Letter to the Editor
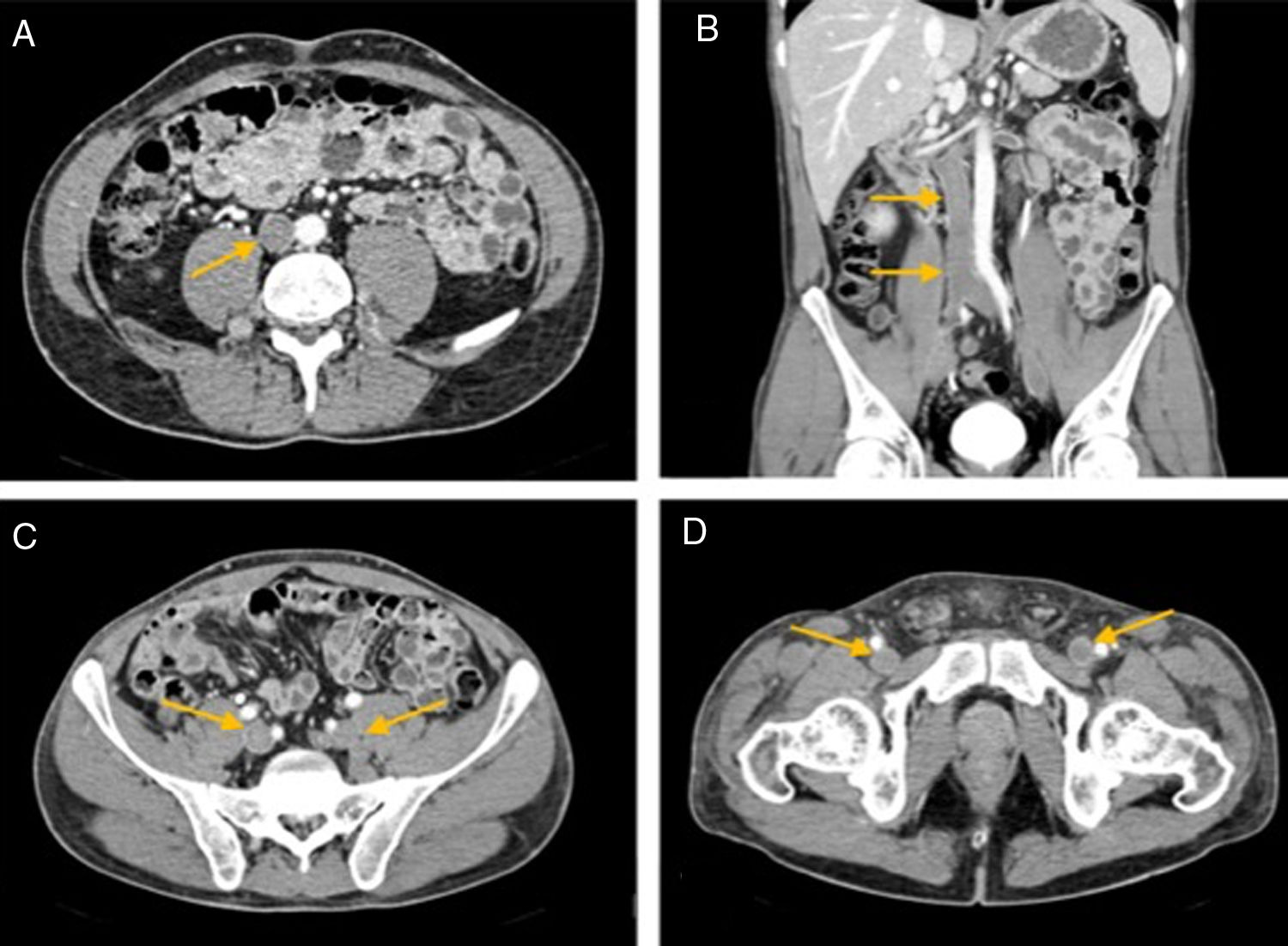
Massive deep venous thrombosis in a patient addicted to cocaine
Trombosis venosa profunda masiva en un paciente adicto a la cocaína
Visitas
18
Ricardo A. Losno
, José C. Milisenda, Jesús Aibar
Autor para correspondencia
Servicio de Medicina Interna, Hospital Clinic, Barcelona, Spain
Este artículo ha recibido
Información del artículo
Opciones para acceder a los textos completos de la publicación Medicina Clínica
Suscriptor
Suscribirse
Comprar
Contactar
Teléfono para suscripciones e incidencias
De lunes a viernes de 9h a 18h (GMT+1) excepto los meses de julio y agosto que será de 9 a 15h
Llamadas desde España
932 415 960
Llamadas desde fuera de España
+34 932 415 960
E-mail