Influenza infection is a highly contagious systemic illness that associates annual epidemics and a heavy socioeconomic burden, affecting anyone at any age. The highest annual incidence occurs in children under 15 years of age and in older individuals over 65. The clinical manifestations of influenza are very variable, and greater morbidity is usually observed in younger children (especially under 2 years of age), in individuals over 65, and in the population with underlying diseases. The highest mortality figures are observed in patients 65 years of age or older and in subjects with diseases included in the defined risk groups.1 In 2018, influenza was associated with an estimated 3–5 million severe cases and between 290,000 and 650,000 deaths annually worldwide.2
Influenza also generates a significant disease burden in both primary and hospital care in Spain. In the last annual report of the Influenza Surveillance System in Spain (SVGE), published by the Carlos III Health Institute (ISCIII), in the 2019–2020 season, 619,000 cases of influenza were confirmed by viral detection in primary care, 27,700 patients were hospitalized, 1800 were admitted to intensive care units, and 3900 deaths were attributable to this viral infection.3 Associated costs in primary care, hospital care, treatment and work absenteeism amount to 1000 million euros per year,4 most of which is spent on the population of individuals with comorbidities, in whom expenditure accounted for 67.1% of the overall health costs for influenza in the 2017/2018 season.5 These data show that current preventive strategies aimed at subjects with comorbidities, regardless of age, are insufficient. It is essential that we examine how to improve the prevention of influenza in this population, given the direct implications and the importance of reducing the clinical and economic burden of this infection in Spain.
Commitment to seasonal influenza vaccination is key to intensifying protection among the most vulnerable populations. This document aims to analyze current influenza vaccination recommendations from the Ministry of Health and to identify those published by the main Spanish scientific societies for patients included in the risk groups defined by the Ministry of Health to support strategies focused on improving vaccination coverage.
Population groups who are candidates for influenza vaccinationThe WHO recommends annual vaccination in: (i) pregnant women at any stage of pregnancy; (ii) children aged 6 months to 5 years; (iii) people over 65 years; (iv) patients with chronic diseases; and (v) health professionals.6
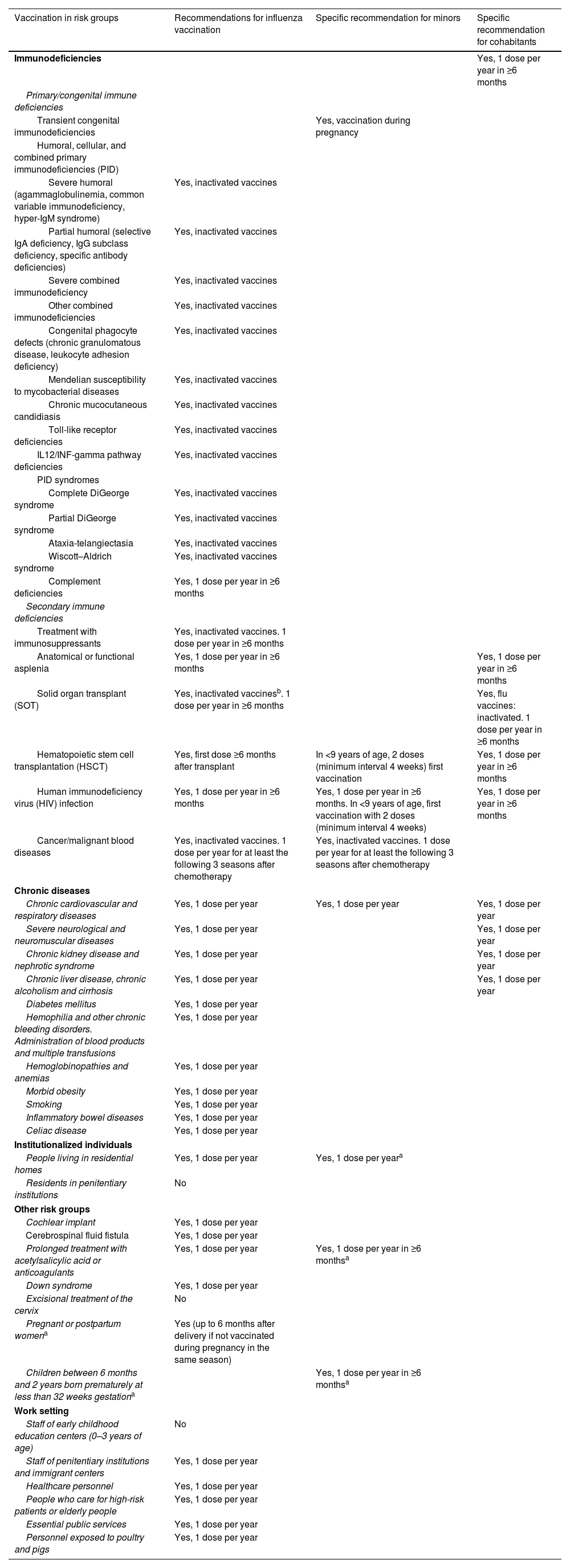
In Spain there are specific recommendations on vaccination in at-risk groups that vary according to the level of immunodeficiency, the type of immunosuppressive treatment and the type of vaccine (Table 1)7; these recommendations set out the vaccination procedures for at-risk patients in the Preventive Medicine and Public Health and in primary care. Therefore, to raise awareness of the importance of the protection of these patients against seasonal influenza, each of the medical societies linked to them should issue and distribute to their members all the necessary recommendations.
Spanish Ministry of Health influenza vaccination recommendations in risk groups.
| Vaccination in risk groups | Recommendations for influenza vaccination | Specific recommendation for minors | Specific recommendation for cohabitants |
|---|---|---|---|
| Immunodeficiencies | Yes, 1 dose per year in ≥6 months | ||
| Primary/congenital immune deficiencies | |||
| Transient congenital immunodeficiencies | Yes, vaccination during pregnancy | ||
| Humoral, cellular, and combined primary immunodeficiencies (PID) | |||
| Severe humoral (agammaglobulinemia, common variable immunodeficiency, hyper-IgM syndrome) | Yes, inactivated vaccines | ||
| Partial humoral (selective IgA deficiency, IgG subclass deficiency, specific antibody deficiencies) | Yes, inactivated vaccines | ||
| Severe combined immunodeficiency | Yes, inactivated vaccines | ||
| Other combined immunodeficiencies | Yes, inactivated vaccines | ||
| Congenital phagocyte defects (chronic granulomatous disease, leukocyte adhesion deficiency) | Yes, inactivated vaccines | ||
| Mendelian susceptibility to mycobacterial diseases | Yes, inactivated vaccines | ||
| Chronic mucocutaneous candidiasis | Yes, inactivated vaccines | ||
| Toll-like receptor deficiencies | Yes, inactivated vaccines | ||
| IL12/INF-gamma pathway deficiencies | Yes, inactivated vaccines | ||
| PID syndromes | |||
| Complete DiGeorge syndrome | Yes, inactivated vaccines | ||
| Partial DiGeorge syndrome | Yes, inactivated vaccines | ||
| Ataxia-telangiectasia | Yes, inactivated vaccines | ||
| Wiscott–Aldrich syndrome | Yes, inactivated vaccines | ||
| Complement deficiencies | Yes, 1 dose per year in ≥6 months | ||
| Secondary immune deficiencies | |||
| Treatment with immunosuppressants | Yes, inactivated vaccines. 1 dose per year in ≥6 months | ||
| Anatomical or functional asplenia | Yes, 1 dose per year in ≥6 months | Yes, 1 dose per year in ≥6 months | |
| Solid organ transplant (SOT) | Yes, inactivated vaccinesb. 1 dose per year in ≥6 months | Yes, flu vaccines: inactivated. 1 dose per year in ≥6 months | |
| Hematopoietic stem cell transplantation (HSCT) | Yes, first dose ≥6 months after transplant | In <9 years of age, 2 doses (minimum interval 4 weeks) first vaccination | Yes, 1 dose per year in ≥6 months |
| Human immunodeficiency virus (HIV) infection | Yes, 1 dose per year in ≥6 months | Yes, 1 dose per year in ≥6 months. In <9 years of age, first vaccination with 2 doses (minimum interval 4 weeks) | Yes, 1 dose per year in ≥6 months |
| Cancer/malignant blood diseases | Yes, inactivated vaccines. 1 dose per year for at least the following 3 seasons after chemotherapy | Yes, inactivated vaccines. 1 dose per year for at least the following 3 seasons after chemotherapy | |
| Chronic diseases | |||
| Chronic cardiovascular and respiratory diseases | Yes, 1 dose per year | Yes, 1 dose per year | Yes, 1 dose per year |
| Severe neurological and neuromuscular diseases | Yes, 1 dose per year | Yes, 1 dose per year | |
| Chronic kidney disease and nephrotic syndrome | Yes, 1 dose per year | Yes, 1 dose per year | |
| Chronic liver disease, chronic alcoholism and cirrhosis | Yes, 1 dose per year | Yes, 1 dose per year | |
| Diabetes mellitus | Yes, 1 dose per year | ||
| Hemophilia and other chronic bleeding disorders. Administration of blood products and multiple transfusions | Yes, 1 dose per year | ||
| Hemoglobinopathies and anemias | Yes, 1 dose per year | ||
| Morbid obesity | Yes, 1 dose per year | ||
| Smoking | Yes, 1 dose per year | ||
| Inflammatory bowel diseases | Yes, 1 dose per year | ||
| Celiac disease | Yes, 1 dose per year | ||
| Institutionalized individuals | |||
| People living in residential homes | Yes, 1 dose per year | Yes, 1 dose per yeara | |
| Residents in penitentiary institutions | No | ||
| Other risk groups | |||
| Cochlear implant | Yes, 1 dose per year | ||
| Cerebrospinal fluid fistula | Yes, 1 dose per year | ||
| Prolonged treatment with acetylsalicylic acid or anticoagulants | Yes, 1 dose per year | Yes, 1 dose per year in ≥6 monthsa | |
| Down syndrome | Yes, 1 dose per year | ||
| Excisional treatment of the cervix | No | ||
| Pregnant or postpartum womena | Yes (up to 6 months after delivery if not vaccinated during pregnancy in the same season) | ||
| Children between 6 months and 2 years born prematurely at less than 32 weeks gestationa | Yes, 1 dose per year in ≥6 monthsa | ||
| Work setting | |||
| Staff of early childhood education centers (0–3 years of age) | No | ||
| Staff of penitentiary institutions and immigrant centers | Yes, 1 dose per year | ||
| Healthcare personnel | Yes, 1 dose per year | ||
| People who care for high-risk patients or elderly people | Yes, 1 dose per year | ||
| Essential public services | Yes, 1 dose per year | ||
| Personnel exposed to poultry and pigs | Yes, 1 dose per year | ||
Recommendations extracted from the document “Working Group on vaccination in the adult population and risk groups of the Vaccinations Program and Registration White Paper. Vaccination in risk groups of all ages and in certain situations. Public Health Commission of the Interterritorial Council of the National Health System. Ministry of Health, Consumer Affairs and Social Welfare, July 2018”.
Additional observations from “Vaccination recommendations for the influenza season 2022–2023. Public Health Commission of the Interterritorial Council of the National Health System, September 2022”. Inactivated vaccines: influenza vaccines that are not live attenuated, including influenza vaccines containing both fractionated viruses and surface antigens.
If the transplantation is carried out in the influenza season, the administration of inactivated vaccine is recommended 1 month after the intervention, and if not performed during the influenza season, it is recommended after 3–6 months.
HIV: human immunodeficiency virus; HSCT: hematopoietic stem cell transplant; PID: primary immunodeficiency; SOT: solid organ transplant.
The groups who are candidates for vaccination against seasonal influenza include patients with diseases that are highly prevalent in Spain, such as diabetes mellitus (DM) (5.1 million cases),8 chronic obstructive pulmonary disease (COPD) (2.9 million reported cases),9 asthma (2.5 million cases),10 human immunodeficiency virus (HIV) infection (0.8 cases per 100,000 population),11 and malignancies (280,100 diagnosed cases per year).12 These form part of an extensive list of diseases in which, despite the recommendations, vaccination coverage remains very low. Specifically, the latest available data from the primary care clinical database of the Spanish National Health System showed a rate of influenza vaccination coverage of 51.9% in COPD patients, 18.5% in asthma patients, 45.3% in DM patients, 38.1% in cancer patients, and 28.7% in HIV patients.13
Co-infection by SARS-CoV-2 and influenza viruses could increase the risk of both infections in the most vulnerable populations, so it is essential to stress the importance of improving protection by offering the influenza vaccine. In terms of public health, the impact of the nationwide influenza vaccination program could have been greater if a higher percentage of the population in the main risk groups listed above had received the vaccine.
Current Ministry of Health recommendationsIn 2018, the Ministry of Health published a paper on vaccination for risk groups of all ages and in certain situations (Table 1).7 According to this report, the annual influenza vaccination strategy is aimed at preventing infection in people at a higher risk of complications if they do contract the disease, and in people who might transmit it to this most vulnerable population, mentioning cohabitants. This document is complemented each season by a set of recommendations issued by the Ministry. Current recommendations for the 2022–2023 season14 include the vaccination of older individuals, preferably over the age of 65, people under 65 who are at high risk of complications from influenza, pregnant women in any trimester of gestation, and women during the postpartum period up to 6 months after delivery.15
The current recommendations for influenza vaccination in risk groups7 were reviewed by a representative from a total of 19 professional associations or scientific societies and approved by the Public Health Commission of the Interterritorial Council of the National Health System (CISNS). The recommendations were drawn up based on the approved guidelines of the CISNS, with updates based on scientific evidence or according to the risk of each population group. Clinical practice guidelines, manuals, recommendations and position papers published by reference groups were consulted as supporting material.7 Based on this document, data extraction was performed for the current recommendations for influenza vaccination in individuals at risk, incorporating the latest updates of the document entitled Vaccination Recommendations for the 2022–2023 Influenza Season published by the same board in September 20227,14 (Table 1).
There are 2 major risk groups: individuals with immunodeficiencies; and those with chronic diseases. In Spain, there are significant numbers of patients in each of these groups: for example, oncological disease is the second most frequent cause of death in Spain,16 while the group of chronic diseases includes patients with chronic cardiovascular and respiratory diseases and diabetes, which represent the first, third and fourth most frequent causes of death in Spain, respectively.16
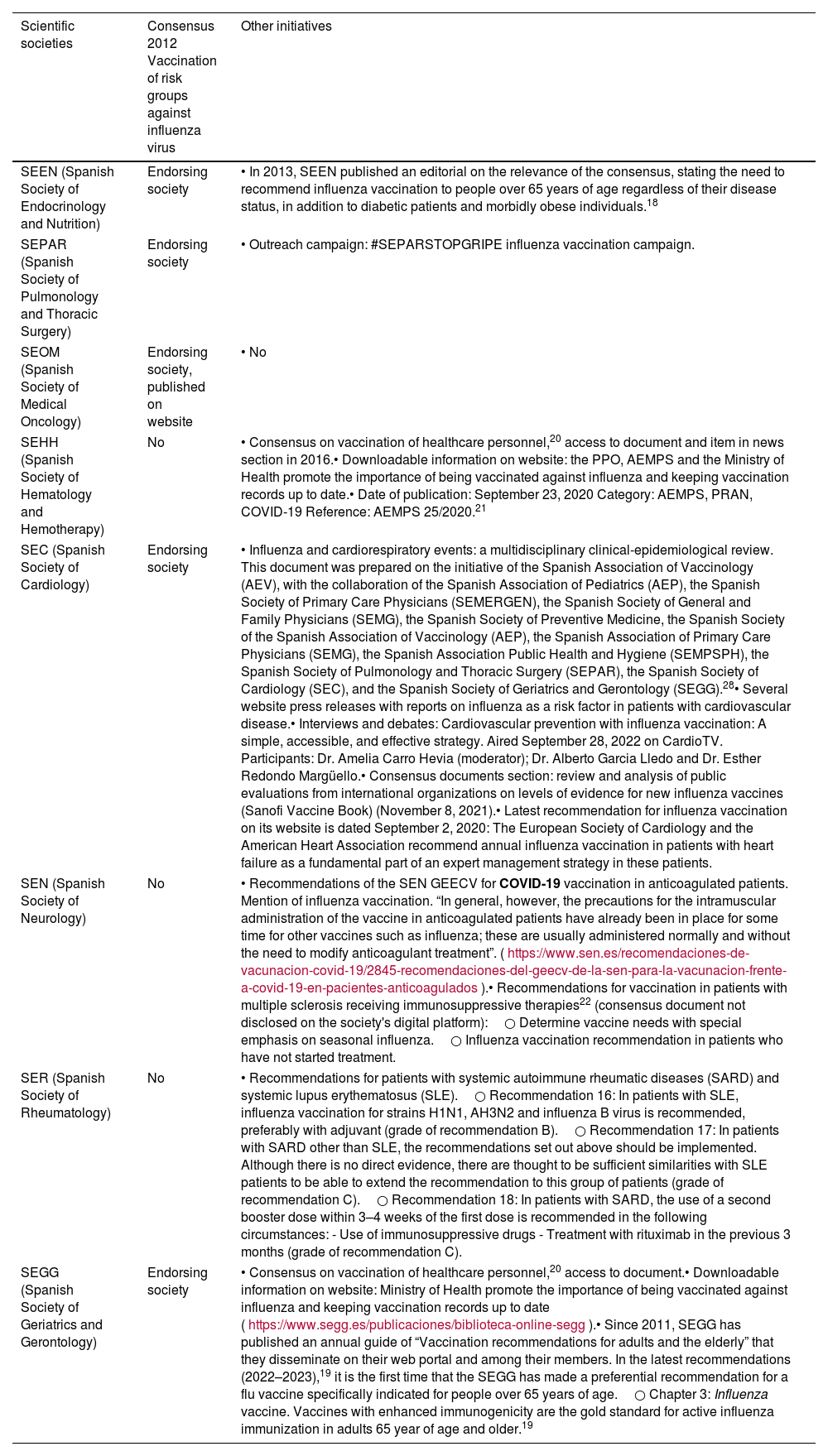
Current recommendations issued by the scientific societiesThe scientific societies are committed to annual influenza vaccination and, as such, they ensure that vaccination recommendations are passed on to their members, so that they can improve the care of their at-risk populations. Some of the main Spanish scientific societies whose members manage patients in the risk groups suggested by the Ministry of Health are the following: Spanish Society of Geriatrics and Gerontology (SEGG), Spanish Society of Endocrinology and Nutrition (SEEN), Spanish Society of Pulmonology and Thoracic Surgery (SEPAR), Spanish Society of Medical Oncology (SEOM), Spanish Society of Hematology and Hemotherapy (SEHH), Spanish Society of Cardiology (SEC), Spanish Society of Neurology (SEN), and Spanish Society of Rheumatology (SER).
The scientific societies that were selected to analyze the grade of influenza recommendations and the dissemination of these guidelines to their members were not among the group of professional associations/scientific societies that were involved in reviewing the Ministry's latest current recommendations.7 However, some of these groups collaborated in the preparation of the 2012 consensus document endorsed by various scientific societies, the General Board of Nursing, and the influenza study group, in which they echoed the recommendations of the Ministry and provided evidence to support these recommendations.17 This document highlights the importance of taking action and vaccinating those groups in which influenza infection carries a higher risk of complications, and looks beyond the protection of individuals over 60–65 years.17 It also underlines the need for the different specialist departments to have access to annually updated protocols (despite partial repetitions), and to involve patient associations to achieve wider uptake. Yet a decade later, this document has not been updated, and data on vaccination coverage13 show that the drive for vaccination in risk groups is still insufficient.
A search was conducted for recommendations on influenza vaccination and the publication of recommendations on the websites of the various selected scientific societies. Table 2 shows the guidelines or mentions of influenza vaccination recommendations in risk groups that appear on the digital platforms of the different scientific societies. Specifically, SEEN, SEPAR, SEC, SEGG and SEOM are among the bodies that endorsed the 2012 Vaccination of risk groups against the influenza virus consensus mentioned above.17 In 2013, SEEN published an editorial on the relevance of this consensus, reaffirming the need for influenza vaccination in patients with endocrinological diseases,18 but they failed to engage in any further initiative or dissemination among their community. SEPAR and the SEC mention their own vaccination campaigns in their news sections, and report on other initiatives aimed at raising awareness about influenza vaccination. Since 2011, SEGG has published an annual guide of “Vaccination recommendations for adults and the elderly” that they disseminate on their web portal and among their members.19 SEOM also posts the aforementioned consensus directly on its website, although it has not undertaken any other action regarding influenza vaccination since the publication of the consensus.17 SEHH has posted the consensus on the vaccination of health workers on its website20 and offers access to the document, and in 2016 they included an item in their news section. They also include in this section a public information notice from the Spanish Agency for Medicines and Medical Devices (AEMPS) and the Ministry of Health on the importance of getting vaccinated against influenza, published in September 2020.21 SEN, and specifically the cerebrovascular disease study group (GEECV), published a series of recommendations for COVID-19 vaccination in anticoagulated patients that briefly mentioned influenza vaccination. They also published a consensus document on vaccine recommendations that included influenza vaccination in patients with multiple sclerosis who are candidates for immunosuppressive therapies.22 Finally, SER publishes its own recommendations for patients with systemic autoimmune rheumatic diseases and systemic lupus erythematosus.23
Compilation of recommendations on vaccination against influenza included in Spanish scientific society communications included in the risk groups defined by the Spanish Ministry of Health.
| Scientific societies | Consensus 2012 Vaccination of risk groups against influenza virus | Other initiatives |
|---|---|---|
| SEEN (Spanish Society of Endocrinology and Nutrition) | Endorsing society | • In 2013, SEEN published an editorial on the relevance of the consensus, stating the need to recommend influenza vaccination to people over 65 years of age regardless of their disease status, in addition to diabetic patients and morbidly obese individuals.18 |
| SEPAR (Spanish Society of Pulmonology and Thoracic Surgery) | Endorsing society | • Outreach campaign: #SEPARSTOPGRIPE influenza vaccination campaign. |
| SEOM (Spanish Society of Medical Oncology) | Endorsing society, published on website | • No |
| SEHH (Spanish Society of Hematology and Hemotherapy) | No | • Consensus on vaccination of healthcare personnel,20 access to document and item in news section in 2016.• Downloadable information on website: the PPO, AEMPS and the Ministry of Health promote the importance of being vaccinated against influenza and keeping vaccination records up to date.• Date of publication: September 23, 2020 Category: AEMPS, PRAN, COVID-19 Reference: AEMPS 25/2020.21 |
| SEC (Spanish Society of Cardiology) | Endorsing society | • Influenza and cardiorespiratory events: a multidisciplinary clinical-epidemiological review. This document was prepared on the initiative of the Spanish Association of Vaccinology (AEV), with the collaboration of the Spanish Association of Pediatrics (AEP), the Spanish Society of Primary Care Physicians (SEMERGEN), the Spanish Society of General and Family Physicians (SEMG), the Spanish Society of Preventive Medicine, the Spanish Society of the Spanish Association of Vaccinology (AEP), the Spanish Association of Primary Care Physicians (SEMG), the Spanish Association Public Health and Hygiene (SEMPSPH), the Spanish Society of Pulmonology and Thoracic Surgery (SEPAR), the Spanish Society of Cardiology (SEC), and the Spanish Society of Geriatrics and Gerontology (SEGG).28• Several website press releases with reports on influenza as a risk factor in patients with cardiovascular disease.• Interviews and debates: Cardiovascular prevention with influenza vaccination: A simple, accessible, and effective strategy. Aired September 28, 2022 on CardioTV. Participants: Dr. Amelia Carro Hevia (moderator); Dr. Alberto Garcia Lledo and Dr. Esther Redondo Margüello.• Consensus documents section: review and analysis of public evaluations from international organizations on levels of evidence for new influenza vaccines (Sanofi Vaccine Book) (November 8, 2021).• Latest recommendation for influenza vaccination on its website is dated September 2, 2020: The European Society of Cardiology and the American Heart Association recommend annual influenza vaccination in patients with heart failure as a fundamental part of an expert management strategy in these patients. |
| SEN (Spanish Society of Neurology) | No | • Recommendations of the SEN GEECV for COVID-19 vaccination in anticoagulated patients. Mention of influenza vaccination. “In general, however, the precautions for the intramuscular administration of the vaccine in anticoagulated patients have already been in place for some time for other vaccines such as influenza; these are usually administered normally and without the need to modify anticoagulant treatment”. (https://www.sen.es/recomendaciones-de-vacunacion-covid-19/2845-recomendaciones-del-geecv-de-la-sen-para-la-vacunacion-frente-a-covid-19-en-pacientes-anticoagulados).• Recommendations for vaccination in patients with multiple sclerosis receiving immunosuppressive therapies22 (consensus document not disclosed on the society's digital platform):○ Determine vaccine needs with special emphasis on seasonal influenza.○ Influenza vaccination recommendation in patients who have not started treatment. |
| SER (Spanish Society of Rheumatology) | No | • Recommendations for patients with systemic autoimmune rheumatic diseases (SARD) and systemic lupus erythematosus (SLE).○ Recommendation 16: In patients with SLE, influenza vaccination for strains H1N1, AH3N2 and influenza B virus is recommended, preferably with adjuvant (grade of recommendation B).○ Recommendation 17: In patients with SARD other than SLE, the recommendations set out above should be implemented. Although there is no direct evidence, there are thought to be sufficient similarities with SLE patients to be able to extend the recommendation to this group of patients (grade of recommendation C).○ Recommendation 18: In patients with SARD, the use of a second booster dose within 3–4 weeks of the first dose is recommended in the following circumstances: - Use of immunosuppressive drugs - Treatment with rituximab in the previous 3 months (grade of recommendation C). |
| SEGG (Spanish Society of Geriatrics and Gerontology) | Endorsing society | • Consensus on vaccination of healthcare personnel,20 access to document.• Downloadable information on website: Ministry of Health promote the importance of being vaccinated against influenza and keeping vaccination records up to date (https://www.segg.es/publicaciones/biblioteca-online-segg).• Since 2011, SEGG has published an annual guide of “Vaccination recommendations for adults and the elderly” that they disseminate on their web portal and among their members. In the latest recommendations (2022–2023),19 it is the first time that the SEGG has made a preferential recommendation for a flu vaccine specifically indicated for people over 65 years of age.○ Chapter 3: Influenza vaccine. Vaccines with enhanced immunogenicity are the gold standard for active influenza immunization in adults 65 year of age and older.19 |
2012 Consensus: Societies involved (Coordinator R. Cisterna): SEMERGEN (Spanish Society of Primary Care Physicians), SEMG (Spanish Society of General and Family Physicians), SEMST (Spanish Society of Medicine and Occupational Safety), SEN (Spanish Society of Neurology), SEOM (Spanish Society of Medical Oncology), SEPAR (Spanish Society of Pulmonology and Thoracic Surgery), SESLAP (Spanish Society of Occupational Health in Public Administration), SEGG (Spanish Society of Geriatrics and Gerontology), SEEN (Spanish Society of Endocrinology and Nutrition), SED (Spanish Diabetes Society), SEC (Spanish Society of Cardiology), CGE (General Council of Nursing), AEEMT (Spanish Association of Specialists in Occupational Medicine) and GEG (Influenza Study Group).
This analysis shows that influenza vaccination recommendations issued by the scientific societies need to be given more widespread exposure: in general, they are published irregularly, and they are not updated. Consequently, the professional members of the societies do not always have the information they need to address this issue satisfactorily. It is also clear that greater efforts during the influenza vaccination campaign from the different medical institutions would boost vaccination among risk groups and would prevent the decision from falling upon each individual specialist.
Overview of the current situationThe main objective of vaccination against seasonal influenza is to reduce morbidity and mortality and the socioeconomic impact of the infection. Individuals with comorbidities constitute a fundamental target group in this area. We have, therefore, analyzed the steps taken by seven of the main scientific societies to disseminate the current Ministry of Health recommendations on influenza vaccination among their members.
In the population over the age of 65, influenza vaccination coverage rates did not change much in the last decade, ranging between 54.3% and 57.7% in the seasons 2011–2012 and 2019–2020, respectively.24 However, it is interesting to note the 13-point increase (from 54.7% to 67.7%) between the 2019–2020 and 2020–2021 seasons, coinciding with the arrival of SARS-CoV-2. This reflects the positive impact of nationwide influenza vaccination programs among this risk group, although these figures are still far from the health objectives proposed by the WHO in 2003 to reach a coverage of 75% against influenza.
Current data on the 2022–2023 season are available from Gripómetro, a tool that uses telephone surveys to gather data on influenza vaccination coverage in real time. They indicate that vaccination coverage has been maintained in people over 65 years (67.3%), and has increased among health professionals compared to last year, with 69.2% coverage.25 The advances have been considerable and should be maintained in subsequent campaigns with the aim of achieving the recommended vaccination rates. Health and social welfare personnel are another group in which the WHO aims to achieve 75% influenza vaccination coverage.
As we report here, medical communities need to promote influenza vaccination among groups of high-risk patients, although this initiative has been recommended for many years and is yet to yield results in practice. Data on influenza vaccination coverage by risk group (COPD, diabetes, cancer patients, etc.) provided by the autonomous communities are scant13; if this information were available, we could identify the populations in which more effective strategies are required to increase vaccination coverage. In this respect, the different scientific societies who put their efforts into the preparation of the 2012 consensus document aimed at increasing the vaccination rate among risk groups17 have lost impetus over time, and the vaccination rates and global immunization of the Spanish population have stagnated.
A survey of the understanding, awareness and practices in influenza vaccination in Spain found that influenza is considered an innocuous disease.26 Furthermore, there is considerable fear of vaccine-related adverse effects among the general population, which often leads to unwillingness to be vaccinated, and a low level of understanding among certain health professionals of their role in increasing awareness of recommendations, despite their usefulness in designing specific strategies to expand nationwide vaccination coverage.26 In fact, the main factor for the population when deciding to receive influenza vaccination is the trust placed in the advice given by their health professional.27 In strategic terms, it is essential that the scientific societies draw up coordinated, structured communication plans for health personnel to make a real impact on the final decision of individuals to be vaccinated against influenza, particularly in the case of patients in the higher risk groups.
This document aims to highlight the need for a global response from associations of health professionals to provide a coordinated response aimed at maximizing vaccination campaigns among risk groups. Although the Spanish societies included in this analysis adhere to the applicable Ministry of Health recommendations, more efforts are needed to promote vaccination in the population. The latest influenza vaccination recommendations set out various strategies, including the need to reinforce the commitment of healthcare communities to influenza vaccination,14 so it is now the responsibility of the scientific societies to establish a proposal and implement the necessary initiatives. The main challenges for the future will be to promote the collection of seasonal influenza vaccination data by risk group to analyze the work carried out by each of the scientific societies and to identify the areas of lowest coverage and develop strategies to improve them.
It is essential that the main scientific societies involved in the management of patients with the most prevalent severe pathologies in Spain, that is to say, the population most requiring influenza vaccination, prioritize outreach initiatives aimed at sharing information and awareness of the importance of influenza vaccination among its members, with the aim of increasing vaccination coverage, reducing morbidity and mortality, and reducing the impact of the significant socioeconomic burden associated with influenza.
Ethical considerationsThe obtention of written informed consent was not necessary to fulfill the present study.
FundingEditorial assistance for the preparation of the article was provided by Medical Statistics Consulting and funded by Sanofi.
Conflict of interestMaría Ángeles Clemente Maya is an employee of Sanofi and may own shares or options in the company's stock.
Ana María Grande-Tejada has collaborated in educational activities funded by GSK, MSD, Pfizer, and Sanofi and has received compensation for services as a consultant for Sanofi, GSK, MSD, Pfizer, and Novartis.