On 31st December 2019, China reported that several cases of pneumonia of unknown origin had occurred in Wuhan (Hubei Province), the cause of which was identified on 7th January 2020: a new coronavirus initially named 2019 novel coronavirus (2019-nCoV). On 11th February, the World Health Organization (WHO) renamed the new virus SARS-CoV-2 due to the similarities between the cause of the severe acute respiratory syndrome that broke out in 2003 and COVID-19 (Coronavirus Infectious Disease 2019).1 On 30th January, WHO declared the outbreak a Public Health Emergency of International Interest, and a pandemic on 11th March. As of 21st March 2020, 311,314 cases have been reported in 188 affected countries, with 13,079 deaths as a result of the infection and 95,800 people recovered (https://www.worldometers.info/coronavirus/). The statistics probably reflect a bias toward the most serious cases, which have more contact with the health system. However, many cases may be undiagnosed, as they are asymptomatic patients who do not go to a health center or mild symptomatology cases that are not confirmed due to the limited availability of diagnostic tests in many countries, such as Spain. Therefore, these statistics are likely to underestimate mild and asymptomatic cases, with the pandemic having a higher prevalence.2
COVID-19 infection can develop as a mild, moderate, or severe illness, including severe pneumonia, acute respiratory distress syndrome (ARDS), sepsis, and septic shock. The incubation period ranges from about 5 days (interval: 4–7 days) to a maximum of 12–13 days. Mild cases may develop flu-like symptoms: high fever, myalgia, fatigue, and respiratory symptoms, especially dry cough, with possible progression to pneumonia. The onset is usually less abrupt than in the flu, and upper respiratory symptoms seem minor or absent.2,3
The main source of infection is other patients already infected with SARS-CoV-2. This is transmitted through respiratory droplets (aerosols>5μm) over short distances (1.5–2m) when patients cough, speak or sneeze, and through contaminated hands when in close contact with the mouth, nose, or bulbar conjunctiva. Prolonged contact represents the highest risk, with casual contacts being less likely to cause contagion. There can be infections from asymptomatic patients and even from people in the incubation period of the disease.2,4 Transmission through infected surfaces is likely, with SARS-CoV-2 recently reported to remain on plastic and stainless steel up to 72h.5
The diagnosis of COVID-19 disease is made through reverse transcription polymerase chain reaction [RT-PCR]) with the detection of nucleic acids of SARS-CoV-2 or by the virus's genetic sequencing. Pharyngeal or nasopharyngeal smear samples, sputum, stools, or blood may be used. The virus can also be isolated in airway epithelial cell cultures, but this is done exclusively in specialized laboratories.6
Therefore, RT-PCR screening is regarded as the gold standard laboratory test for the diagnosis of COVID-19. False negatives have been documented in some cases, likely due to inappropriate viral sample material or technical problems during nucleic acid extraction.7–9
The incidence of COVID-19 has been observed to be higher in men than in women, for which the influence of the X chromosome and sex hormones on innate and adaptive immunity has been suggested as a possible explanation.10,11
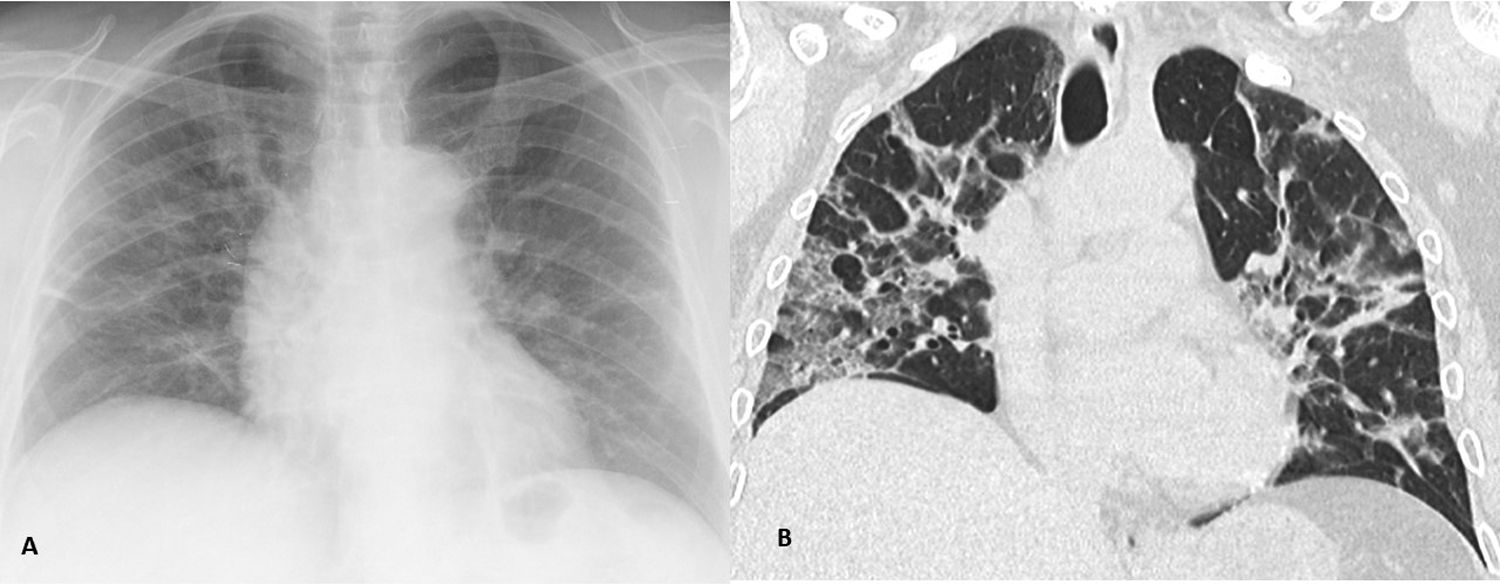
The respiratory system is the first to be affected by COVID-19, so in suspicious cases it is common to request a chest X-ray (CXR) as the first imaging test. However, its diagnostic performance in the initial stages of the disease is limited, since it has been reported that pathological findings identifiable on chest computed tomography (CCT) may not be detected on X-rays.7,12,13
This fact, together with the initial circumstances of the epidemic, when the accumulation of suspected cases exceeded the availability of RT-PCR tests, led to certain working groups adopting CCT as a diagnostic test in the absence of RT-PCR, leading to an unprecedented number of CCT studies to try to characterize a novel infectious disease. The CCT obtained very good results in these studies, observing that the pathological findings of the CCT can occur even before the symptoms7,12,13 and be diagnostic in patients with initial RT-PCR false-negative results.7,8,14 Therefore, it was concluded that CCT is a very valuable tool to diagnose COVID-19 infection, both in the initial assessment of lung involvement and for its follow-up.7,15,16
This article aims to identify the characteristics of this rapidly progressive viral pneumonia on imaging tests, both on CXR and CCT. The characteristic imaging findings of the different stages of the disease, the evolution of the findings associated with the progression of the disease or with clinical improvement, and the variation in the prevalence of the different patterns according to the age of the patients are also explained.
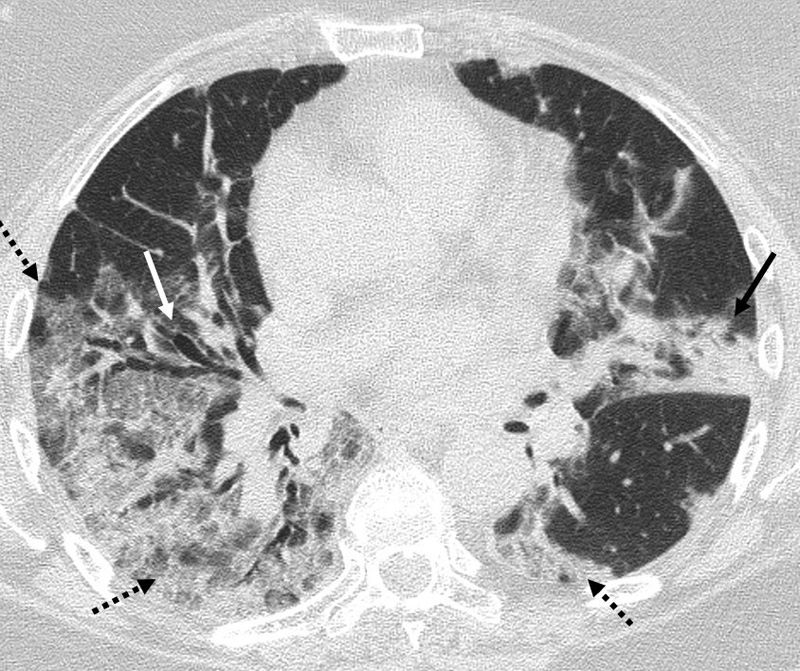
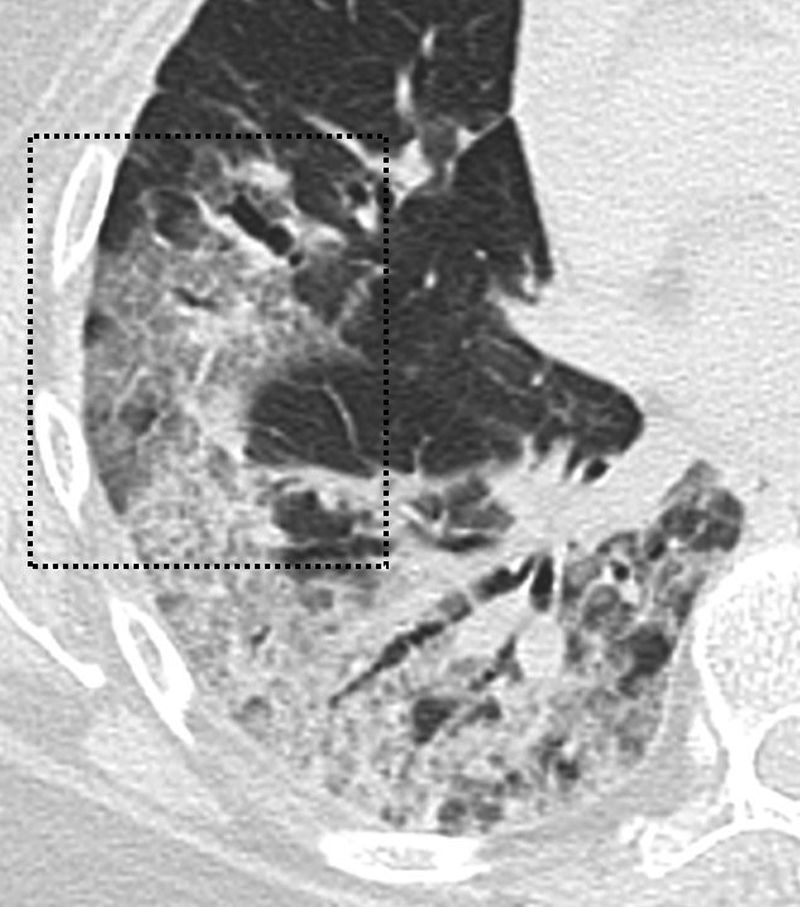
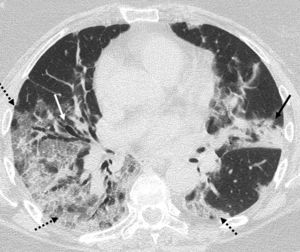
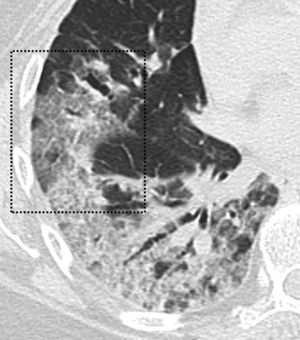
Radiological findingsAccording to several studies and reviews, ground-glass opacities, either alone or in combination with pulmonary consolidations, is the most common finding on CCT (Fig. 1). Other findings include interlobular septal thickening, bronchiectasis (Fig. 1), pleural thickening, crazy-paving pattern, bilateral lower lobe involvement and peripheral and posterior location predominance (Fig. 2), with diverse incidence in the different studies.7,12,16–19
As a reminder of the radiological lexicon, we consider it interesting to make a brief description of the characteristics of ground-glass opacities (GGO), consolidations and crazy-paving pattern. The term GGO describes the parenchymal opacification of the lung which produces a smaller increase in attenuation compared to consolidation, so that, despite the increase in density, the pulmonary vessels and the bronchial walls continue to be differentiated from the affected parenchyma. GGO represent a partial invasion of the airspace, they are less opaque than the consolidations and, as an important consequence, a CCT is more sensitive than the CXR regarding their detection.20
Consolidation refers to the occupation of the airspace by pathological products (pus, water, blood, etc.). Consolidation occurs as a homogeneous increase in pulmonary parenchymal attenuation (increased density) that obscures the margins of vessels and airway walls. It may exhibit the air-bronchogram sign, which refers to the visualization of air-filled bronchial lumens within a pulmonary parenchymal opacity which, in turn, implies airway patency.20
The crazy-paving pattern is characterized by a inter and intralobular septal thickening superimposed on GGO, simulating a crazy-paving floor, a finding that is also identified much more easily on CCT than on CXR.20
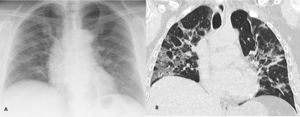
The lower sensitivity of CXR for GGO detection (Fig. 3), the most common finding of COVID-19 pulmonary infection that may go unnoticed, has been postulated as the reason for the low sensitivity of CXR compared to CCT in the initial diagnosis of this infection.16,21
According to the review carried out by Salehi et al., of 919 patients with confirmed SARS-CoV-2 infection (COVID-19), the most commonly found findings on CCT were: GGO (88.0%), bilateral involvement (87.5%), peripheral distribution (76.0%) and multilobar involvement (more than one lung lobe) (78.8%).7 There are studies that report that up to 38% of patients showed involvement of the 5 lung lobes, with the right lower lobe being the most commonly affected (76%) and the middle lobe the least affected (56%).7,22
The predominantly peripheral distribution is more accurately detected in the CCT studies compared to the CXR studies, with bilateral pneumonia being the most common finding identified in CXR.16
Pleural effusion, pericardial effusion, mediastinal lymphadenopathy, cavitation, halo sign, and pneumothorax were detected less commonly in affected patients.7,18,19,23,24 Cavitation is an air-filled space following necrosis of the parenchyma, in this case inflammatory, which is visualized as an area of radiolucency or low attenuation within a lung consolidation. The halo sign is a ground-glass opacity around a nodule or mass.20
Acute pulmonary thromboembolism in COVID-19 has been reported as a rare complication.25 Another rare form of presentation is the pattern of organized pneumonia, including the reverse halo sign consisting of a ground-glass area surrounded by a complete or nearly complete consolidation ring.16,19,26
Radiological findings according to the stage of the diseaseLung lesions have been found to be detected in CCT studies from even before the onset of symptoms to day 14 after the onset of symptoms, with an average of 4 days.7,18
Jin et al. carried out a classification of the patients with COVID-19 in 5 stages, according to the progression time: ultra-early, early, rapid progression, consolidation and dissipation. The first or ultra-early stage comprised the first and second weeks after exposure, the patients were asymptomatic, and the most common CCT scan finding was to observe single or multiple GGOs, patchy consolidations, lung nodules with surrounding ground-glass opacity and air bronchogram.7,15 The second or early stage, related to the first and second day after the onset of symptoms, included the majority (54%) of patients, and was characterized by single or multiple GGOs and the combination of GGOs with interlobular septal thickening (crazy-paving). In the third or rapid progression stage, between days 3 and 7 from the onset of symptoms, large confluent consolidations were observed with air bronchogram. The fourth consolidation stage corresponds to the second week of the symptomatic period, in which there is a reduction in the size and density of lung consolidations. Finally, in the fifth stage or that of dissipation, 2–3 weeks from clinical onset, pulmonary opacities are patchier and bronchial wall thickening and reticulation due to intra and interlobular septal thickening are more commonly observed.7,15
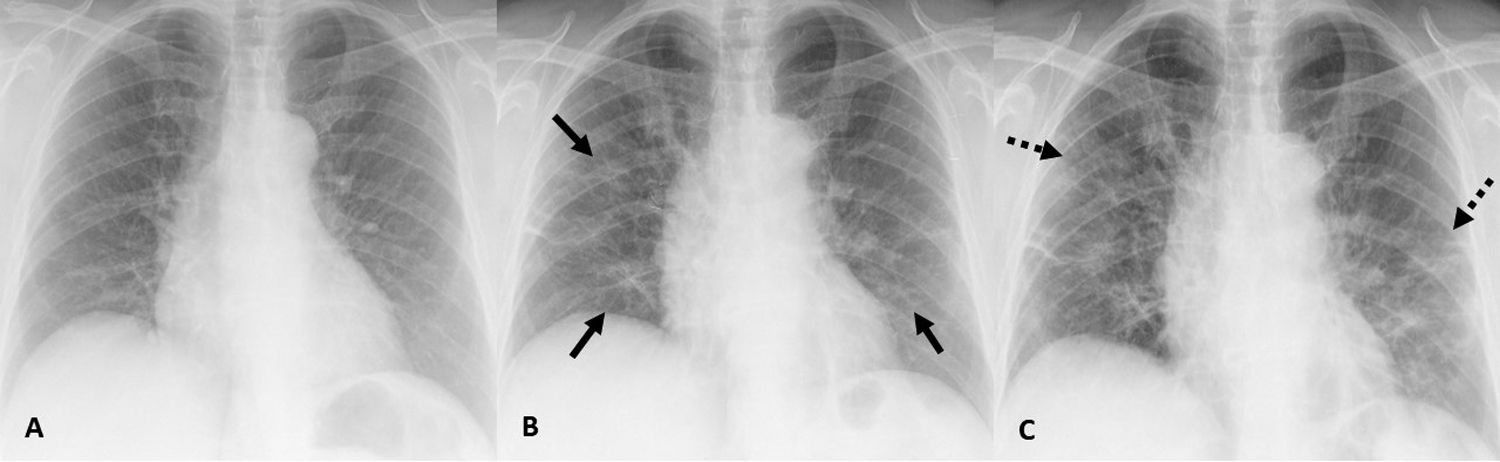
The study by Pan et al. included a follow-up CCT, which showed that GGO, consolidations and septal thickening increased in the majority of patients (85%) who experienced disease progression, suggesting fibrotic changes.7,13 Several studies have reported that this interlobular septal thickening occurs only secondary to GGO and consolidations, so that as the disease progresses, the prevalence of the reticular pattern due to septal thickening increases.19 These findings can also be identified on CXR (Fig. 4).
(A) CXR image of a 75-year-old patient who came to the emergency department and presented with 1-day history of COVID-19 infection-compatible symptoms without initial radiographic abnormalities and with a positive PCR result for SARS-CoV-2. (B) CXR image, 4 days later, in which bilateral GGO are identified. (C) CXR image, 2 days later, in which a reticular pattern is observed due to septal thickening with persistence of GGO.
Patients who showed pulmonary nodules on the initial CCT also showed an increase in their number and size, or their fusion, during follow-up. However, a decrease in the attenuation of other nodules was also identified in the same follow-up study.7,13
According to another study that also evaluated changes in tomographic findings over the course of the disease, GGO with a lower number of affected lobes predominated in the early stages and, as the disease progressed, there was an increase in this pattern's involvement, an increase in the affected lung lobes and the occurrence of pulmonary consolidations. On average, it was observed that CCT findings are more significant on day 10 of the disease and that, after day 14, 25% of the patients showed an improvement in radiological findings, including a decrease in the number of affected lobes, a resolution of the crazy-paving pattern and the consolidations.7,27
In patients with poor progression, findings seem to develop toward patterns that are compatible with ARDS, identifiable in both CXR and CCT. ARDS is the complication that usually requires the transfer of patients with COVID-19 to ICUs and the most common cause of death in ICUs in this group.7 In the studies of patients admitted to the ICU, the most commonly described findings were multilobar and subsegmental consolidations.28 The occurrence of pleural effusion has been reported as a complication of late stages of the disease, probably secondary to heart failure in the context of ARDS.7,17
In pregnant women, the usual progression reported also starts with GGO in the initial stages, which as the disease progresses develops into consolidations and crazy-paving patterns, with resolution of these findings in the final stages. In this group of patients, the most common symptoms were fever (13/15 patients) and cough (9/15 patients). The most common laboratory abnormality was lymphopenia (12/15 patients). All pregnancies were successfully completed, patients recovered, and newborns had no complications.29
Radiological findings according to age groupsSong et al. carried out a study in which patients were classified into 2 groups according to their age, patients younger than 50 and patients older than 50. In the youngest group of patients, 77% had GGO, and only 23% had lung consolidations, while in the group of patients over 50 years, GGO were present in 55% and consolidations in 45%, difference that was statistically significant between both groups (p<0.001). Atypical findings were also more common in older patients.15,18
Correlation between reverse transcriptase polymerase chain reaction results and chest computed tomographyGenerally, published studies show an agreement between positive RT-PCR results and CCT findings consistent with COVID-19 infection. However, a limited number of patients with COVID-19-compatible radiological findings on CTT have been reported to have negative RT-PCR results in the first few days. The first TCT study showed GGO that later evolved to foci of consolidation. RT-PCR results in these patients turned positive between days 2 and 8.8,14
Comparison between radiological findings of COVID-19 pneumonia and other viral pneumoniasThe study carried out by Cheng et al. included a comparison between the imaging tests findings of patients with COVID-19 pneumonia and SARS-CoV-2 negative patients who had pneumonia from other viruses. In the case of SARS-CoV-2 positive patients, lung opacities had a peripheral location in 100% of the cases, while this was only 31.8% in the negative. The number of affected lung segments and lobes was also higher in the case of positive cases (15 segments and 5 lobes in positives, 9 and 3.5, respectively, in negative cases). In COVID-19 cases, it was more common to find the air bronchogram sign and reticular pattern, while in negative patients, it was more common to identify centrilobular nodules.10
The radiological findings of viral pneumonias are remarkably diverse. Pneumonia caused by the varicella-zoster virus is characterized by halo-sign nodules and GGOs in both lungs. Influenza A virus infection is characterized by multiple areas of consolidation and diffuse ground-glass opacities, similar to the presentation of COVID-19 pneumonia. Therefore, in a context of continuous SARS-CoV-2 spread that coincided with the circulation of other respiratory viruses, confirmation by PCR would be necessary to determine whether any pulmonary CCT pathological findings were the result of SARS-CoV-2 or whether they had been caused by another virus, for example, the influenza A virus.10
An important consideration is the fact that the radiological findings must be interpreted in an epidemiological context with risk of SARS-CoV-2 infection such as the one that, unfortunately, is affecting Spain today. In populations with a low SARS-CoV-2 infection pre-test probability, these typical imaging findings should be interpreted with caution.7
ConclusionsCCT has proven to be an imaging technique with particularly good results to identify lung involvement caused by SARS-CoV-2 (COVID-19), even in asymptomatic patients. Ground-glass opacities, isolated or in combination with lung consolidations, is the most common radiological finding.
The radiological findings that correlate with clinical improvement occur after 2 weeks of favorable symptom progression and include a gradual consolidation resolution, with a decrease in the number of lesions and the number of affected lung lobes. On the other hand, in cases of poor progression, the most common cause of transfer to ICUs and the first cause of death is ARDS.
Some studies show that CCT findings can vary according to the age of the patients, with consolidations being more common in older patients and GGO in younger patients.7
It should be borne in mind that radiological findings must be interpreted in an epidemiological context with a risk of SARS-CoV-2 infection.
The authors consider that, despite the existence of published clinical guidelines that strongly recommend performing CTT in patients with suspected COVID-19,7 if this option were to be considered in countries such as Spain, it would be necessary to consider the availability of computed tomography equipment and health personnel to carry them out. In our opinion, new studies are needed to evaluate the role that CCT can have in determining or modifying the therapeutic management that these patients will need. The authors consider it interesting and necessary to carry out studies on the utility of CXR in the monitoring of the disease, and its comparison with CCT in order to find the most effective therapeutic management, since the availability of portable CXR equipment is greater, it is a faster, cheaper, simpler technique and means less radiation for patients.
In the case of patients with negative PCR results, but with typical clinical manifestations, history of exposure and, therefore, a high clinical suspicion of infection, CCT can be a highly valuable diagnostic technique because it can detect the characteristic findings of the disease.7
Conflict of interestThe authors declare no conflict of interest.
The authors want to express our recognition and appreciation to all the health professionals who are working to fight this pandemic. We would like to express our gratitude to our colleagues of the Obispo Polanco General Hospital of Teruel and especially to the radiologic technologists, PS García, EO Navarro and L Oro.
Please cite this article as: Sánchez-Oro R, Torres Nuez J, Martínez-Sanz G. La radiología en el diagnóstico de la neumonía por SARS-CoV-2 (COVID-19). Med Clin (Barc). 2020;155:36–40.