The frontline medical staff are under heavy workload conditions and are at high risk of infection with coronavirus disease 2019. This pandemic has burdened unprecedented psychological stress. The study aimed to compile and analyze the challenges of mental health among medical staff during the COVID-19 outbreak
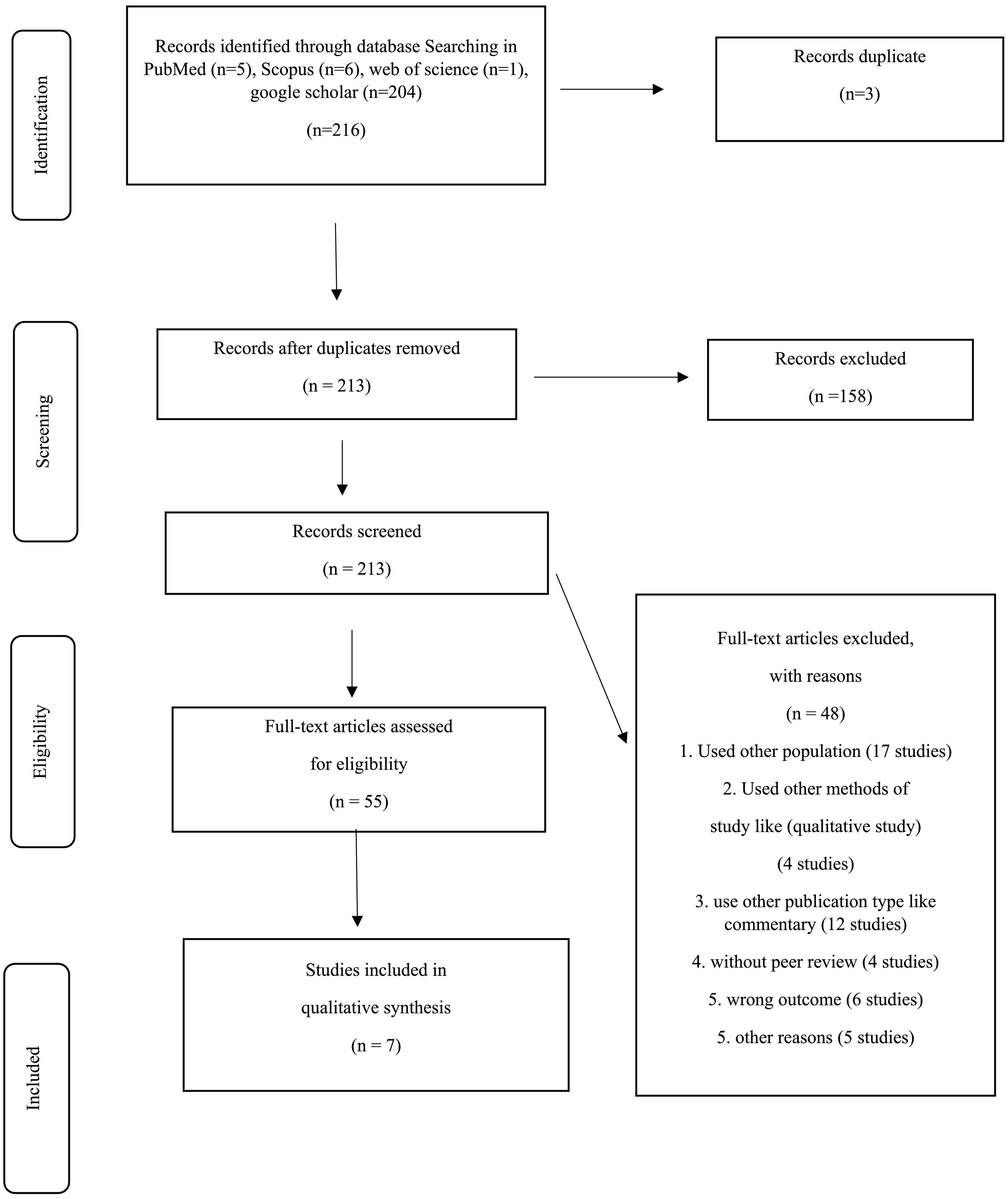
MethodPubMed, Scopus, Web of science, and google scholar databases were systematically searched for published studies. Cross-sectional studies examining the impact of the COVID-19 outbreak on the medical staff's mental health were selected.
ResultEventually, 7 articles were extracted for the final analysis after reviewing the titles, abstracts, and full text. The results show that the most common psychological problems of medical staff include stress, anxiety, and depression. The medical staff had higher levels of fear, anxiety, and stress than the management staff. Among physicians and nurses, the two groups that are most involved with patients with COVID-19, the nurses showed more anxiety and stress than physicians.
ConclusionThe mental health of the medical staff during the COVID-19 epidemic is at greater risk than ever before. Therefore, it is necessary to adopt comprehensive and effective supportive policies and strategies for health systems and governments.
El personal médico de primera línea se encuentra en condiciones de gran carga de trabajo y tiene un alto riesgo de infección por la enfermedad del coronavirus 2019. Esta pandemia ha causado un estrés psicológico sin precedentes. El objetivo del estudio fue recopilar y analizar los desafíos de la salud mental en el personal médico durante el brote de COVID-19.
MétodoSe realizaron búsquedas sistemáticas de estudios publicados en las bases de datos PubMed, Scopus, Web of Science y Google Scholar. Se seleccionaron estudios transversales que examinaran el impacto del brote de COVID-19 en la salud mental del personal médico.
ResultadoFinalmente, se extrajeron 7 artículos para el análisis final después de revisar los títulos, resúmenes y texto completo. Los resultados muestran que los problemas psicológicos más comunes del personal médico incluyen estrés, ansiedad y depresión. El personal médico tenía niveles más altos de miedo, ansiedad y estrés que el personal administrativo. Entre los médicos y enfermeros, los dos grupos que más se involucran con los pacientes con COVID 19, los enfermeros mostraron más ansiedad y estrés que los médicos.
ConclusiónLa salud mental del personal médico en la epidemia de COVID 19 está en mayor riesgo que nunca. Por lo tanto, es necesario adoptar políticas y estrategias de apoyo integrales y efectivas por parte de los sistemas de salud y los gobiernos.
As of mid-December 2019, COVID-19 has been released from Wuhan, China, to 216 countries1,2, and now the disease has become a global problem3. Human-to-human transmission, asymptomatic carriers, and high transmission capacity have played a role in this epidemic1,4.
As the disease is transmitted through small droplets and direct contact, nurses and physicians are at risk5. The rapid spread of the disease and the spread of epidemics have put a lot of physical and psychological pressure on care and treatment personnel6 because, during the spread of diseases, health workers suffer from an increased workload, and increased working hours, as well as a lot of stress6–8. According to previous studies on SARS [Severe acute respiratory syndrome] and MERS [Middle East respiratory syndrome], healthcare workers experienced a lot of psychological stress due to working in high-risk areas9. Factors such as social stigmatization, contact with infected patients, an increasing number of confirmed cases, reduction of protective equipment, working in heavy clothing, widespread media coverage, lack of specific drugs and vaccines, as well as reports of contamination of health workers to COVID 19 and their mortality10,11 are effective in causing this stress and lead to increased concern and anxiety in these people7,10,12,13. The research results showed that half of the clinical staff reported a 56% increase in stress levels and a 53% increase in workload in SARS epidemics in Singapore14.
Facing the critical situation puts medical personnel at the forefront of the fight against COVID-19 and risk for mental and emotional disorders15. Numerous studies have shown that employees of the treatment team experienced depression and anxiety during the epidemic COVID 1916–18. However, stress is the most important environmental risk factor for mental disorders, and long-term stress can put people at greater risk for infection2.
Attention to mental health has been important in all areas of life, including the working life of the individual, because the factors in the work environment are widely related to the health and illness of working people. Mental health is one of the most important factors in human development and fact, it is an aspect of the general concept of health and relies on methods and measures that are used to prevent the spread of mental illness, treatment, and rehabilitation. It is also considered one of the pillars of health and the necessity of a useful, effective, and satisfying individual life. Promoting the mental health of the people of a society, especially its influential and constructive groups, is a necessity for the dynamism, prosperity, and uplifting of that society19.
However, the healthcare sector is one of the most important areas for health development because it is directly related to human health. Therefore, it is very important to have mental health in this group, because this group of people needs a strong interpersonal relationship that leads to professional cohesion, and this is provided by their comprehensive health. The mental health and severity of the perceived stress of the treatment team are important in the efficiency and quality of their performance, and high mental health care providers can provide good services to patients20. On February 15, 2020, the National Health Council (NHC) issued a statement highlighting the importance of providing psychological intervention and support to medical staff5. To emphasize the importance of mental health in the staff of the health team, especially nurses, and considering the naming of 2020 as the Year of Nurses and Midwives21, it is necessary to reach a consensus on this issue by using a systematic review. Therefore, the present study was conducted to achieve mental health challenges during the epidemic of COVID-19 disease in medical staff. It is hoped that the knowledge gained will help to better understand these problems and apply them to the care of the health care team.
MethodsThe present study is a systematic review conducted following the Cochrane manuscript22, Based on this directive manuscript, the following steps were considered.
Select a questionThe first step in studying the current systematic review is to select the research question that the present study intends to answer the question "What are the mental health challenges in medical staff during the COVID-19 epidemic?" is done.
Selection criteriaA comprehensive overview of all articles published in the four databases PubMed, Scopus Direct, Google Scholar, and Web of science between December 1, 2019, and April 12, 2020, using the keywords 'Covid19', 'coronavirus', 'mental health, 'mental hygiene', 'medical staff', which was selected from the Medical Subject Headings (MESH), and It was also used by OR and AND operators. All published cross-sectional articles were included in the study of any mental health problems caused by the treatment of Covid19 in the treatment team. English and non-English articles were the criteria for entering the study. We excluded the lack of access to full-text articles, peer-review articles, narrative reviews, thesis, editorials, protocols, letters to the editor, and conference papers.
Study selectionThe preliminary search was conducted by two authors, and all searched articles were entered into the End not and the duplicate studies were deleted. Two authors independently and blindly reviewed all articles in terms of title and abstract and, if necessary, resolved disputes with the consent or participation of a third reviewer.
Data extraction and quality assessmentWe used structured forms to extract relevant data, such as country, journal, authors, year of publication, setting, type of sampling, sample size, Characteristic of the participant, analytic test, measurement tools, mental health problem, and main study results. We extracted the prevalence rate or frequency or mean± SD of the mental health problem in the participants. Two researchers independently assessed the quality of the studies incorporated in the review using a bias risk assessment tool, Strengthening21. One reviewer extracted all the data and assessed the risk of bias, while a second reviewer cross-checked the information for accuracy and completeness.
ResultsThe search resulted in a total of 216 records. After 3 duplicates were removed 213 records remained to be screened. We excluded 158 records based on title and abstract screening. We assessed 55 articles in full text, of which we excluded 48. Seven published studies met the inclusion criteria for this systematic review. Fig. 1 illustrates the selection process of the included studies.
Eventually, 7 articles were reviewed. All descriptive articles were cross-sectional, all done in China. Various tools have been used to assess mental health disorders, levels of stress and anxiety, depression, insomnia, burnout, post-traumatic stress disorder, and fear. Table 1 summarizes the studies.
The summary of the included studies.
| Author (s)(Year) | Aim | Measurement | Sample size | Type of sampling | Papulation | Characteristics |
|---|---|---|---|---|---|---|
| Mo, et al. (2020)24 | To investigate work stress among Chinese nurses that are supporting Wuhan in fighting against Coronavirus Disease 2019 infection and explore relevant influencing factors. | Stress Overload Scale (SOS) | 180 | convenient sampling | Nurses | Most participants were female (90%), work experience 2 to 32 years, undergraduates (79.44%), Senior nurses (56.67%), married (49.44%), and age 21-48 years. |
| Self-Rating Anxiety Scale (SAS) | ||||||
| Lai, et al (2020)23 | To assess the magnitude of mental health outcomes and associated factors among health care workers treating patients exposed to COVID-19 in China. | -Patient Health Questionnaire | 1257 | cluster sampling | Nurses: 764 (60.8%) and physicians 493 (39.2%) | Most participants were women (76.7%), married, widowed, or divorced (66.7%), undergraduate or less (75.8%), junior technical title (55.6%), frontline health care workers (41.5%) and age 26-40 years |
| -Generalized Anxiety Disorder scale | ||||||
| -Insomnia Severity Index | ||||||
| -Impact of Event Scale–Revised | ||||||
| Wu, et al (2020)27 | to compare the frequency of burnout between physicians and nurses on the front line and those working in usual wards. | Maslach burnout inventory | 190 | Census | Nurses & physicians | Median of age: 33 years |
| Most participants were women (83%), married (68%), medical oncology (54%), | ||||||
| Work experience 6-10 years (37%), 21-40 working hours per week (54%) | ||||||
| Kang, et al (2020)26 | Explore the mental health status of medical and nursing staff in Wuhan, the efficacy of the psychological care accessed, and their psychological care needs. | -Patient Health Questionnaire | 994 | Census | Nurses: 811(81.6%) physicians: 183 (18.4%) | Most participants were female (85.5%), aged 25 to 40 years (63.4%), married (56.9%), undergraduate or less (85%), and junior technical title (66.3%). |
| -Generalized Anxiety Disorder (GAD-7) | ||||||
| -Insomnia Severity Index (ISI) | ||||||
| -Impact of Event Scale-Revised (IESR) | ||||||
| Lu, et al (2020)25 | to realize the psychological status of the medical workforce | The numeric rating scale (NRS)-Hamilton Anxiety Scale (HAMA)- Hamilton Depression Scale(HAMD) | 2299 | Census | Medical staff (doctors and nurses): 2042 AdministrativeStaff (including the logistics): 257 | Most participants were femail (76.7%), aged 31 to 40 (43%), Working years (36.15%), married (71.2%), One or more Children (65.6%) |
| Huang, et al (2020)15 | To investigate the mental health of clinical first line medical staff in COVID-19 epidemic and provide theoretical basis for psychological intervention. | -Self-rating anxiety scale (SAS) | 230 | cluster sampling | Nurses: 160 (69.6%) | Most participants were female (81.3%), aged 20-59 years, married (77%), junior college (58.7%) |
| -Post Trauma Stress Disorder Self-Rating Scale(PTSD-SS) | Doctors: 70 (30.4%) | |||||
| Zhu, et al (2020)2 | the prevalence and influencing factors of anxiety and depression symptoms in first-line anti-epidemic medical staff and their coping styles for these negative emotions. | -self-rating anxiety scale (SAS)-self-rating depression scale (SDS)-simplified coping style questionnaire (SCSQ) | 165 | Census | Nurses: 86 Doctors: 79 | Most participants were female (83%), unmarried (72.1%), no child (80.6%), Undergraduate (60.6%), and aged (34.16 ± 8.06) years,Length of employment (11.35 ± 8.60) years, Working days in epidemic area (15.65 ± 46.63) days |
In five studies, nurses and physicians were the study population. The most common mental health problems were stress, anxiety, and depression. As 44.6% of nurses had anxiety, 34% had insomnia, 71.5% had stress, and 50.4% had depression23, Mo et al. reported nurses' stress levels (39.91 ± 12.92) and anxiety levels (32.19 ± 7.56), which was higher than the national standard (29.8 ± 0.46)24. In a study by Lu et al., Conducted at Fujian Provincial, the medical staff had 22.6 percent mild to moderate anxiety and 2.9 percent severe anxiety, 8.11 percent mild to moderate depression, and 0.3 percent severe depression. And the fear level in the medical staff was moderate to high25. In another study conducted by Huang et al., 23.04% of the medical staff were anxious, of which 2.17% had severe anxiety, 4.78% had moderate anxiety, and 16.09% had mild anxiety. Also, the stress level in medical personnel was 27.39%15. 36 percent of medical staff had very mild mental health disorders, 34.4% had mild disorders, 22.4% had moderate and 6.2% had severe disorders26. The results of a study by Zhu et al. In Guangzhou showed that the prevalence of anxiety in nurses was 27.9% and the prevalence of depression was 43%. Also, the prevalence of anxiety in physicians was 11.4% and depression was 45.6%2. The results also showed that factors related to the mental health problems of medical staff included, being single, working long hours per week, being more professional, nursing24 working in isolation, worries about being infected with the virus, lack of personal protective equipment, concerns about not controlling the prevalence of Covid19, frustration with treatment outcomes, feelings of loneliness due to separation from loved ones25, and a history of anxiety and depression2.
The results of studies comparing mental health problems in the two groups of physicians and nurses indicate that the mental health of physicians was more favorable than that of nurses (P = .007) so the level of anxiety in nurses was higher than that of physicians, 26.88. Percentage versus 14.29%2,15. Studies have also shown that women are more anxious and stressed than men15,23, Sleep disorders were more common in first-line personnel than in second-line personnel (P <.001)23. Employee burnout was lower in first-line personnel than in common wards (P <.0001). Also, there was less concern about the contamination of oneself and one's family with Covid19 and concerns about the prolonged duration of the outbreak in first-line personnel than in other wards27. Also, medical personnel had higher levels of fear, anxiety, and stress than management personnel26.
DiscussionThe most important mental health problems during the prevalence of COVID-19 in the medical staff in this systematic review were stress, anxiety, and depression. Sleep disorders, burnout, anxiety, and fear were other problems related to the mental health of the treatment team in the prevalence of COVID-19, which was systematically reviewed. The occurrence of stress and anxiety in medical staff is not a new phenomenon, and due to the nature of working with human lives, difficult working conditions, unconventional shifts, and unpredictable working conditions, medical staff experience some degree of stress and anxiety28–30. However, the COVID-19 outbreak has created complex conditions for the medical staff, which has changed the severity and extent of the psychological damage inflicted on the medical staff. Factors such as; Facing an emerging infectious agent with little information about it increases the risk of becoming ill, worrying about one's family situation, putting too much pressure on a large number of patients, insufficient resources and facilities, and so on, increased stress and anxiety in the treatment team in the COVID 19 epidemic24,31,32.
In this regard, Zhu et al. Reported the prevalence of anxiety and stress in the treatment team during the Corona epidemic in China above; Anxiety levels in nurses and physicians were reported to be 27.9% and 11.4%, respectively, and the prevalence of depression was 43% and 45.6%2. A study by Huang et al. Also showed a high level of stress and anxiety experienced by the treatment team during the Corona epidemic, stating that 23% of the treatment staff experienced anxiety, and 27.39% experienced stress15. A study by Lai et al. Reported that nurses' anxiety rate as a member of the treatment team during the Corona epidemic was 44.6 percent and stress levels were 71.5 percent23, indicating a high level of perceived stress and anxiety. The study also reported 34 percent of insomnia and 50.4 percent of depression. On the other hand, research has shown that depression and insomnia are both directly related to the amount of stress perceived and will increase stress in the individual28,33, Therefore, it can be inferred that all of these factors have exacerbated each other due to the synergistic effect they have on each other, and as a result, the mental health of the treatment team during the Corona era has been more and more threatened.
During this period, fear is another problem that threatens the mental health of the treatment team. A study by Lu et al. found that those in the treatment team who were in close contact with COVID-19 experienced 1.4 times more fear than others25. Concerns about family health, stigma, isolation, and distance from the treatment team for not getting sick34 and lack of medication and equipment35 have been reported in the Corona epidemic. Although fear is mentioned in articles in this systematic review in only one of them, the experience of fear and its constant understanding will have a negative impact on health and well-being36 and although less attention has been paid to this issue in the articles, it should not be overlooked.
Occupational burnout was another result of this systematic review, and it was found that the prevalence of COVID-19 was able to cause some degree of burnout in the treatment team. Although the prevalence of this mental health risk factor was lower than that of stress, anxiety, and depression, and was mentioned only in one article, it is a very important finding because safety and quality of care have a close relationship37. Of course, perhaps one of the reasons for such a result is that stress and anxiety show their symptoms in a shorter time than burnout, and burnout occurs as a result of long-term stress experiences38,39. Therefore, perhaps in future studies and in the face of longer-term exposure to COVID-19, burnout will be identified as one of the most common mental health challenges in the treatment team. Studies have shown that burnout with work pressure, challenging work environment, high stress, fatigue from work-related sense37,40, high patient acceptance41, and lack of resources and facilities42 are in connection; All of these factors have occurred in the corona epidemic, and therefore in this health crisis has affected the whole world. Due to the factors mentioned above, the burnout of the treatment team should be taken seriously. Occupational burnout, on the other hand, is associated with stress39,43, depression40, and anxiety44, and so it can be argued that exposure to stress, anxiety, or depression can accelerate burnout. Therefore, practical solutions to solve these problems should be sought by the treatment team.
Among the strategies that can be used in Corona epidemic to prevent or moderate mental health problems in the medical staff, can refer to increase the support of the institute and system, emotional support of the treatment team, teaching effective adaptability styles and coping, Stress management45, self-care treatment by adequate rest, eating adequate fluids and healthy food, exercise, and avoiding inappropriate adaptation styles such as resorting to tobacco, alcohol, or medication34.
ConclusionIn this systematic review, it was found that the COVID-19 epidemic was due to; High acceptance, double workload, high risk of getting sick, dealing with the complex and unpredictable work environment, lack of medicine and equipment, isolation, family distance, stigma, and community distance from the treatment team for fear of the spread of the disease is subject to a great deal of physical and psychological stress. These mental health factors have put the treatment team at greater risk than ever before; as in the Corona epidemic, the treatment team experiences unprecedented stress, anxiety, depression, fear, insomnia, and burnout. Therefore, it is necessary to adopt appropriate strategies and policies to deal with and reduce these factors, especially stress and anxiety, which were the most threatening factors to the mental health of the medical staff. Therefore, it is recommended that at this critical time, the country's health organizations provide more and better quality support to the medical staff and try to reduce the severity of the psychological damage to the medical staff by adopting appropriate and effective strategies. Because there is still no definite timeline for the end of the COVID-19 epidemic, the healthcare system of countries needs the effective services of the treatment team more than ever. Therefore, by identifying these mental health threats in this systematic review, we must now look for logical and possible solutions.
LimitationsThe speed with which articles related to COVID-19 are published is expanding day by day, but due to the importance of the topic, the present research team had to review the articles systematically within the period specified in the proposal. Therefore, it is possible that after the end of this review, other valuable findings will be mentioned in the articles that did not enter our study due to the nature of the systematic review and the determination of the search time. Therefore, more systematic reviews are recommended in the future.
FundingThe author(s) disclosed the receipt of the following financial support for the research, authorship, and/or publication of this article: This study was financially supported by the Research Vice-Chancellor of Mazandaran University of Medical Sciences (Grant No. 7444).
Ethical statementThis study was approved by the ethics committee of Mazandaran University of Medical Sciences (Code: IR.MAZUMS.REC.1399.7444).
AuthorshipAll of the authors participated in the study design, the article search, the study selection.
Process, the data extraction and analysis, and the drafting of the manuscript.
The authors express their gratitude to the Deputy of research of Mazandaran University of medical sciences (Sari, Iran) for their contribution to financial support.