Ulcerative colitis (UC) is an inflammatory bowel disease, usually begins in the rectum and can involve the entire colon. Damage done by this condition can lead to several intestinal and extraintestinal manifestations (EIMs). Due to malnutrition, malabsorption and medications used in UC patients, bone mineral loss seems to happen at a higher pace, compared to healthy population. In this study, we aim to investigate bone mineral density (BMD) and its related biomarkers like Vitamin K, Vitamin D and Calcium in patients with UC.
MethodOne hundred and one documented UC patients with at least one year of treatment entered our study. BMD was measured with dual X-ray absorptiometry. Lab tests were done to examine Vitamin K, Vitamin D, Calcium and Magnesium levels in patients’ serum.
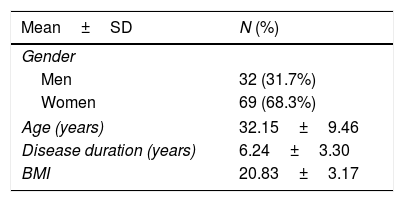
ResultsAmong 101 patients, 32 (31.7%) were men and 69 (68.3%) were women. The mean age of participants was 32.15±9.46 years. The mean duration of the disease was 6.24±3.30 years. Based on the femoral T-score index, 75 (74.3%) patients had normal femoral density, 24 (23.8%) were osteopenic and (2%) 2 patients had osteoporosis. Bone loss significantly correlated with age and disease. Patients with lower BMI tend to have lower BMD values. The data analysis revealed lower levels of Vitamin K, Vitamin D and Calcium in UC patients significantly decreased bone density indexes, except for lumbar T-score which did not showed a clear relationship with serum Vitamin K. Also, the cumulative dose of prednisolone significantly reduced all BMD indicators, especially in patients with longer disease durations.
ConclusionBMD in UC patients seems to decrease at a higher pace and it's associated with lower levels of Vitamin K, Vitamin D and Calcium in serum as well as corticosteroid consumption. Close follow-ups, dietary supplements and corticosteroid usage limitations could be beneficial for UC patients and decrease the risk of developing osteoporosis.
La colitis ulcerosa (CU) es una enfermedad inflamatoria intestinal, generalmente comienza en el recto y puede afectar todo el colon. El daño causado por esta condición puede conducir a varias manifestaciones intestinales y extraintestinales (EIM). Debido a la desnutrición, la malabsorción y los medicamentos utilizados en los pacientes con CU, la pérdida de minerales óseos parece ocurrir a un ritmo más rápido, en comparación con la población sana. En este estudio, nuestro objetivo es investigar la densidad mineral ósea (DMO) y sus biomarcadores relacionados como la vitamina K, la vitamina D y el calcio en pacientes con CU.
MétodoCiento uno pacientes con CU documentados con al menos un año de tratamiento ingresaron a nuestro estudio. La DMO se midió con absorciometría de rayos X dual. Se realizaron pruebas de laboratorio para examinar los niveles de vitamina K, vitamina D, calcio y magnesio en el suero de los pacientes.
ResultadosEntre 101 pacientes, 32 (31,7%) eran varones y 69 (68,3%) eran mujeres. La edad media de los participantes fue de 32,15±9,46 años. La duración media de la enfermedad fue de 6,24±3,30 años. Según el índice de puntuación T femoral, 75 (74,3%) pacientes tenían densidad femoral normal, 24 (23,8%) pacientes eran osteopénicos y 2 (2%) pacientes tenían osteoporosis. La pérdida ósea se correlacionó significativamente con la edad y la enfermedad. Los pacientes con un IMC más bajo tienden a tener valores de DMO más bajos. El análisis de datos reveló niveles más bajos de vitamina K, vitamina D y calcio en pacientes con CU que disminuyeron significativamente los índices de densidad ósea, excepto para la puntuación T lumbar que no mostró una relación clara con la vitamina K sérica. Además, la dosis acumulada de prednisolona redujo significativamente todos los indicadores de DMO, especialmente en pacientes con enfermedad de mayor duración.
ConclusiónLa DMO en pacientes con CU parece disminuir a un ritmo más rápido y está asociada con niveles más bajos de vitamina K, vitamina D y calcio en suero, así como con el consumo de corticosteroides. Los seguimientos minuciosos, los suplementos dietéticos y las limitaciones en el uso de corticosteroides podrían ser beneficiosos para los pacientes con CU y disminuir el riesgo de desarrollar osteoporosis.
Inflammatory bowel diseases (IBD), including Ulcerative Colitis (UC) and Crohn's Disease (CD), have an increased prevalence in recent years, especially in middle-income countries like Iran.1 Osteoporosis in patients with IBD has been discussed widely in previous studies.2,3 Several mechanisms in IBD patients increase the risk of osteoporosis.4 Malabsorption of Calcium and Vitamin D due to small intestine involvement or surgical procedures, malnutrition and decreased mineral intake, and drugs used in treating IBD patients such as corticosteroids all have a cumulative effect on the bone loss process.5
The role of Vitamin D and Calcium in delaying bone loss is well known.6,7 As osteoporosis was associated with low levels of Vitamin K in several studies,8,9 this vitamin has gained more attention in osteoporotic processes. Increased fracture rate was seen in patients with low Vitamin K intake.10 Also, patients showed a decreased fracture rate when they took Vitamin K supplements.11 Due to malabsorption and malnutrition, IBD patients tend to have lower blood Vitamin K levels, similar to Vitamin D and Calcium.5 These pieces of evidence have encouraged us to include Vitamin K as a factor in our study.
Corticosteroids are used widely in the treatment of IBDs.12 Increased osteoclasts formation and osteoblasts apoptosis, decreased intestinal absorption, and increased urinary exertion of Calcium have been observed in patients with IBD under corticosteroid treatment in previous studies. Although corticosteroids accelerate the bone loss process, these changes seem to be reversible if IBD patients stop taking these medications.13
In this paper, we studied bone loss in IBD patients using Bone Densitometry (BMD) of multiple sites. We acquired serum levels of Vitamin K, Vitamin D, and Calcium to measure if these components are related to the bone loss process in IBD. We also went through patients’ drug history to see if taking corticosteroids accelerates bone loss in these patients.
Materials and methodAll UC patients (diagnosis confirmed by endoscopy and biopsy) from 2015 to 2020 attending the Gastroenterology Clinic of Sina Hospital, Tehran, who took treatment for at least one year entered our study. Patients’ characteristics and demographic data were extracted from the clinic's database retrospectively. Patients who already received treatment for osteoporosis or had other conditions like end-stage renal disease (ESRD), chronic kidney disease (CKD), cirrhosis, and cancer were excluded. Finally, a total number of 101 patients were included in our study and followed up prospectively in the course of our study. There were 32 men and 69 women ranged between 18 to 52 years old. Disease duration varied from 1 year to 17 years. All patients were treated with 5-aminosalicylic acid; 17 also took azathioprine. Twenty-five patients were using glucocorticoids or had a history of taking these medications. The National Committee of Ethics approved this study in September 2020. All data remained concealed, and patients’ rights were preserved.
Patients’ bone density measured by dual-energy X-ray absorptiometry (DXA) from Lumbar spine (L1-L4), and femoral neck (Lunar Prodigy Advance, GE Healthcare, Illinois, USA). BMD results were reported as standard deviations from the mean peak value for a reference population of the same sex and race (T-score) and normal values corrected for age and sex (Z-score). Reference values are determined by the Iranian normal population score.14
Fasting blood samples were stored at −30°C until analysis. High-performance liquid chromatography (HPLC) was used for Vitamin K measurement. 25-hydroxyvitamin D2 level was measured by radioimmunoassay (RIA), and Spectrophotometry was used to determine blood's Calcium and Magnesium levels.
Results were expressed by Mean and Standard Deviation (SD) for continuous variables and frequency and percentage for categorical variables. Spearman's rank correlation coefficient was used to investigate correlations. Qualitative variables were analyzed by the Mann–Whitney test. A P-value<0.05 was significant in all tests. All data were analyzed by IBM SPSS software version 26.
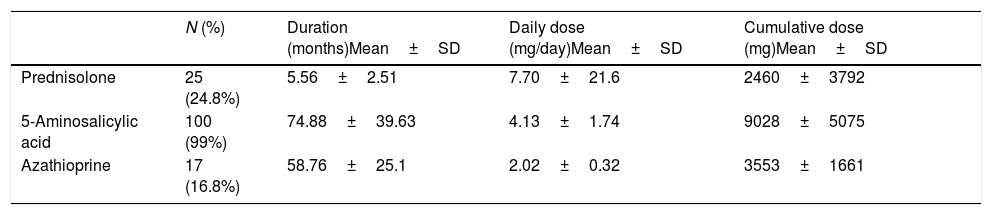
ResultsAll demographic data and clinical features have shown in Table 1. The mean age of participants and the mean duration of their disease were 32.15±9.46 and 6.24±3.30, respectively—normal distribution of all variables tested by the Shapiro–Wilk test. The mean body mass index (BMI) of participants was 20.83±3.17. The mean Z-score and T-score for the femoral neck were −0.30±0.60 and −0.52±0.76, respectively. According to T-score reference values, 75 patients (74.3%) had a normal bone density, 24 (23.8%) were osteopenic, and 2 (2%) were osteoporotic. The lumbar spine indexes with a mean Z-score of −0.35±0.61 and a mean T-score of −0.60±0.72 revealed the bone density of 81 patients (80.2%) were normal, 19 (18.8%) were osteopenic, and 1 (1%) was osteoporotic. In our laboratory findings, the mean serum's 25OH-VitD level was 36.94±8.11, the mean Vitamin K was 0.70±0.25, and the mean Calcium and Magnesium concentrations were 9.34±0.43 and 1.82±0.26, respectively. The mean daily and cumulative drug dosages have shown in Table 2.
Medications used in the treatment of ulcerative colitis.
| N (%) | Duration (months)Mean±SD | Daily dose (mg/day)Mean±SD | Cumulative dose (mg)Mean±SD | |
|---|---|---|---|---|
| Prednisolone | 25 (24.8%) | 5.56±2.51 | 7.70±21.6 | 2460±3792 |
| 5-Aminosalicylic acid | 100 (99%) | 74.88±39.63 | 4.13±1.74 | 9028±5075 |
| Azathioprine | 17 (16.8%) | 58.76±25.1 | 2.02±0.32 | 3553±1661 |
In a statistical analysis with Spearman's rank correlation coefficient, T-score and Z-score values for the femoral neck were significantly correlated with cumulative dosages of 5-aminosalicylic acid and glucocorticoids, as well as BMI and serum concentrations of 25OH-VitD, Vitamin K, and Calcium (p<0.05). This correlation was also significant in lumbar BMD values. Azathioprine dosage and serum Magnesium levels showed no significant correlation with femoral neck BMD values. Although in the lumbar region, an increase in blood Magnesium significantly increased the lumbar spine's T-score values (p<0.05).
DiscussionThis study investigated the bone loss process in UC patients to see if it's related to their demographic features like age or gender, laboratory findings, and medication types and dosages. Although bone density values negatively correlated with patients’ age and disease duration, BMI played a protective role against osteoporosis. Among our laboratory indexes, a rise in Vitamin K, Vitamin D, and Calcium significantly enhanced T-score values for both femoral and lumbar regions. Glucocorticoids like prednisolone had the most negative impact on bone density values, compared to 5-aminosalicylic and azathioprine.
In 2004, G Barrera et al. conducted a study on 845 healthy subjects to investigate bone density indexes based on their BMIs.15 Based on their results, individuals with a BMI of more than 30 are less likely (about one-third) to experience osteoporosis than patients with BMI less than 25. Azzopardi et al. in 2013 studied 83 CD patients, and they found a significant increase in T-score values in individuals with higher BMIs.16 Our study also proves that patients’ BMI significantly correlates with bone density indexes and bone loss process. Although our population mainly were young and middle-aged adults (range 18–52 years), patients’ age negatively correlated with bone density values. In a study in 2007, Bianchi also concluded regardless of the population's age groups, there is a significant decrease in their bone density values with aging.17 Khosla et al. also emphasized this relation in a study on 56 young individuals with a median age of 34.18
Several studies discussed the role of Vitamin K in osteoporosis. Tauseef et al. considered malabsorption to be the reason for low levels of serum Vitamin K in IBD patients. In 2008, Kuwabara et al. conducted a study of 70 patients with IBD (29 CD, 41 UC) and measured their bone density indexes and serum levels of Vitamin K and D.19 They found a statistically significant correlation between decreased Vitamin K levels and the development of osteoporosis in IBD patients. Except for the lumbar T-score, Vitamin K also correlated with other bone density indexes in our study; however, this relation was not statistically strong.
Calcium and Vitamin D roles in bone turnover are clear, and their supplements are widely used in patients with higher risks of osteoporosis. In a review article in 2013, Mouli et al. found a higher prevalence of Vitamin D deficiency and insufficiency in IBD patients than healthy individuals.20 After reviewing 22 studies on this matter, they also mentioned malnutrition and malabsorption as the main reason for decreased Vitamin D levels in these patients. Similar to Vitamin D, Calcium is believed to be reduced in IBD, according to previous studies.21 Our study results also showed lower amounts of serum Vitamin D and Calcium in UC patients significantly decreased all BMD indexes and subsequently accelerated the bone loss process.
Corticosteroid's destructive effects on bone density discussed widely in recent years.22,23 By stimulating osteoclasts formation, promoting osteoblasts apoptosis, and reducing Calcium's intestinal absorption, Corticosteroids are believed to minimize bone minerals through different mechanisms, suggested by Piodi et al. study in 2014.24 Jahnsen et al. conducted a study on sixty CD and sixty UC patients with a 2-year follow-up to investigate the role played by possible contributing factors in their bone loss process.25 They found one of these roles could be played by Corticosteroids, as they witnessed poorer bone density outcomes in treatment with higher doses. Our results showed patients under treatment with corticosteroids significantly had lower BMD indexes. Drug administration in UC patients should be monitored closely, and Corticosteroid therapy should be limited to short periods. Unlike corticosteroids, we found no correlation between azathioprine dosage and bone density indexes. Although 5-aminosalicylic acid correlated weakly with BMD values, we believe this relationship to be accidental since all of our participants were taking 5-aminosalicylic acid, and other devastating factors like age or disease duration could be involved. We suggest future studies with a larger population and more extensive follow-ups to investigate this matter.
Young adult and middle-aged UC patients are at risk of developing osteoporosis.26 Decrease in serum Vitamin K, Vitamin D, and Calcium in these patients as well as taking corticosteroids in the course of treatment significantly reduce BMD values. Taking dietary supplements and avoiding corticosteroid regimens are potentially beneficial for UC patients to mitigate the risk of osteoporosis.
Conflict of interestsAuthors declared no conflict of interests.