Technology Enhanced Medical Education International Conference (THEME 2019)
Más datosThe purpose of this systematic review is to examine a study of early initiation of breastfeeding for the development of neonatal intestinal microbiota.
MethodThe method used was an online database that has been published. Keywords used include breast milk composition; compare breastfed and formula-fed (breastmilk and formula milk); gut microbiota in infants; early initiation.
ResultsBased on the review of 12 selected articles, it was found that breast milk contains various prebiotics that can be transmitted to infants through breastfeeding. The dominant prebiotics is Lactobacillus spp., Bifidobacterium spp., and Staphylococcus spp. which has different amounts depending on the type of breast milk provided.
ConclusionBreastfeeding has many benefits, especially for the baby's immunity and digestion. Giving early initiation of breastfeeding means giving breastfeeding early in life so that it greatly affects the development of good bacterial colonies in infants.
The World Health Organization (WHO) in its global strategy states that exclusive breastfeeding during the first 6 months of life is very good, besides that WHO also recommends giving early initiation of breastfeeding within the first hour of birth.1 Khan et al. found that neonates given breastfeeding after the first hour of life had 2 times (combined odds ratio [OR] 2.02; 95% CI: 1.40, 2.93) the risk of dying in the first month of life compared with neonates who were given ASI in the first hour.2 Providing early initiation can prevent an increase in half of the newborn deaths and improve the nutritional status of children.3 In Indonesia in 2018 the number of IMD is 58.2% with an IMD<1h as much as 84.1%.4 Early breastfeeding initiation can also increase breastfeeding exclusively in infants.5
Breastmilk contains a diverse bacterial community and can be transferred to more babies by direct breastfeeding than by using breastmilk pumps.6,7 Existing bacterial include E. coli, Enterobacteriaceae, Staphylococcus spp., Bacteroides spp., Bifidobacterium spp., Enterococcus spp., and Lactobacillus spp.8 The advantage of bacteria transferred through breast milk is that it can prevent infection, allergies, colic/crying and obesity in infants.9
MethodKeywords used to search for articles in identification based on clinical studies and observational study. Keywords contain breast milk composition; compare breastfed and formula-fed; gut microbiota in infants; early initiation.
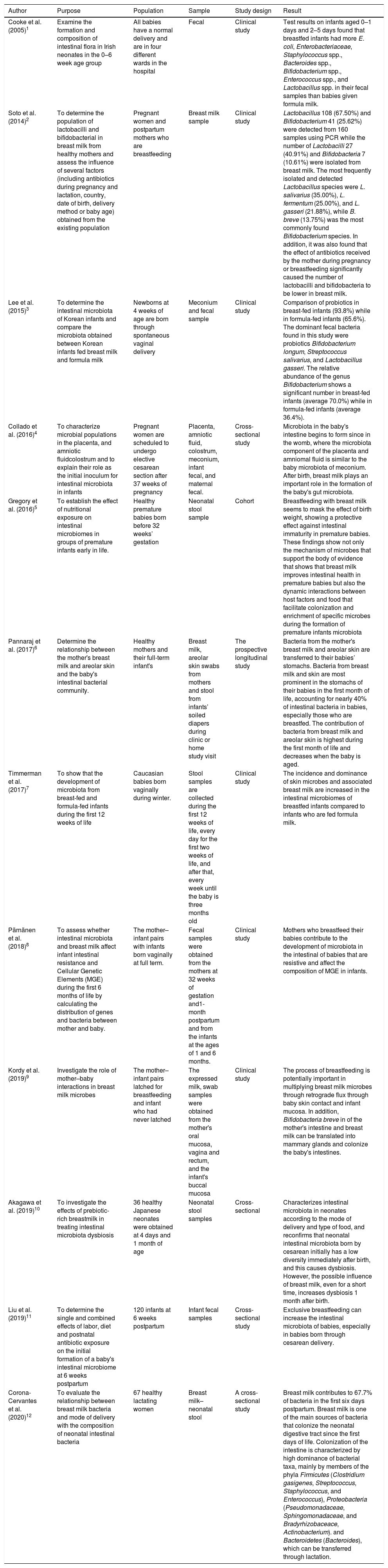
ResultReferring to several articles found relating to the initiation of early breastfeeding, breastfeeding, and the development of bacteria in the baby's intestines. The author chose 12 articles based on clinical research that looked at the effect of breastfeeding on the development of bacteria in the intestines of infants. The characteristics of the six studies are presented in Table 1.
Characteristics, sample, and results of selected studies.
| Author | Purpose | Population | Sample | Study design | Result |
|---|---|---|---|---|---|
| Cooke et al. (2005)1 | Examine the formation and composition of intestinal flora in Irish neonates in the 0–6 week age group | All babies have a normal delivery and are in four different wards in the hospital | Fecal | Clinical study | Test results on infants aged 0–1 days and 2–5 days found that breastfed infants had more E. coli, Enterobacteriaceae, Staphylococcus spp., Bacteroides spp., Bifidobacterium spp., Enterococcus spp., and Lactobacillus spp. in their fecal samples than babies given formula milk. |
| Soto et al. (2014)2 | To determine the population of lactobacilli and bifidobacterial in breast milk from healthy mothers and assess the influence of several factors (including antibiotics during pregnancy and lactation, country, date of birth, delivery method or baby age) obtained from the existing population | Pregnant women and postpartum mothers who are breastfeeding | Breast milk sample | Clinical study | Lactobacillus 108 (67.50%) and Bifidobacterium 41 (25.62%) were detected from 160 samples using PCR while the number of Lactobacilli 27 (40.91%) and Bifidobacteria 7 (10.61%) were isolated from breast milk. The most frequently isolated and detected Lactobacillus species were L. salivarius (35.00%), L. fermentum (25.00%), and L. gasseri (21.88%), while B. breve (13.75%) was the most commonly found Bifidobacterium species. In addition, it was also found that the effect of antibiotics received by the mother during pregnancy or breastfeeding significantly caused the number of lactobacilli and bifidobacteria to be lower in breast milk. |
| Lee et al. (2015)3 | To determine the intestinal microbiota of Korean infants and compare the microbiota obtained between Korean infants fed breast milk and formula milk | Newborns at 4 weeks of age are born through spontaneous vaginal delivery | Meconium and fecal sample | Clinical study | Comparison of probiotics in breast-fed infants (93.8%) while in formula-fed infants (65.6%). The dominant fecal bacteria found in this study were probiotics Bifidobacterium longum, Streptococcus salivarius, and Lactobacillus gasseri. The relative abundance of the genus Bifidobacterium shows a significant number in breast-fed infants (average 70.0%) while in formula-fed infants (average 36.4%). |
| Collado et al. (2016)4 | To characterize microbial populations in the placenta, and amniotic fluidcolostrum and to explain their role as the initial inoculum for intestinal microbiota in infants | Pregnant women are scheduled to undergo elective cesarean section after 37 weeks of pregnancy | Placenta, amniotic fluid, colostrum, meconium, infant fecal, and maternal fecal. | Cross-sectional study | Microbiota in the baby's intestine begins to form since in the womb, where the microbiota component of the placenta and amniomal fluid is similar to the baby microbiota of meconium. After birth, breast milk plays an important role in the formation of the baby's gut microbiota. |
| Gregory et al. (2016)5 | To establish the effect of nutritional exposure on intestinal microbiomes in groups of premature infants early in life. | Healthy premature babies born before 32 weeks’ gestation | Neonatal stool sample | Cohort | Breastfeeding with breast milk seems to mask the effect of birth weight, showing a protective effect against intestinal immaturity in premature babies. These findings show not only the mechanism of microbes that support the body of evidence that shows that breast milk improves intestinal health in premature babies but also the dynamic interactions between host factors and food that facilitate colonization and enrichment of specific microbes during the formation of premature infants microbiota |
| Pannaraj et al. (2017)6 | Determine the relationship between the mother's breast milk and areolar skin and the baby's intestinal bacterial community. | Healthy mothers and their full-term infant's | Breast milk, areolar skin swabs from mothers and stool from infants’ soiled diapers during clinic or home study visit | The prospective longitudinal study | Bacteria from the mother's breast milk and areolar skin are transferred to their babies’ stomachs. Bacteria from breast milk and skin are most prominent in the stomachs of their babies in the first month of life, accounting for nearly 40% of intestinal bacteria in babies, especially those who are breastfed. The contribution of bacteria from breast milk and areolar skin is highest during the first month of life and decreases when the baby is aged. |
| Timmerman et al. (2017)7 | To show that the development of microbiota from breast-fed and formula-fed infants during the first 12 weeks of life | Caucasian babies born vaginally during winter. | Stool samples are collected during the first 12 weeks of life, every day for the first two weeks of life, and after that, every week until the baby is three months old | Clinical study | The incidence and dominance of skin microbes and associated breast milk are increased in the intestinal microbiomes of breastfed infants compared to infants who are fed formula milk. |
| Pärnänen et al. (2018)8 | To assess whether intestinal microbiota and breast milk affect infant intestinal resistance and Cellular Genetic Elements (MGE) during the first 6 months of life by calculating the distribution of genes and bacteria between mother and baby. | The mother–infant pairs with infants born vaginally at full term. | Fecal samples were obtained from the mothers at 32 weeks of gestation and1-month postpartum and from the infants at the ages of 1 and 6 months. | Clinical study | Mothers who breastfeed their babies contribute to the development of microbiota in the intestinal of babies that are resistive and affect the composition of MGE in infants. |
| Kordy et al. (2019)9 | Investigate the role of mother–baby interactions in breast milk microbes | The mother–infant pairs latched for breastfeeding and infant who had never latched | The expressed milk, swab samples were obtained from the mother's oral mucosa, vagina and rectum, and the infant's buccal mucosa | Clinical study | The process of breastfeeding is potentially important in multiplying breast milk microbes through retrograde flux through baby skin contact and infant mucosa. In addition, Bifidobacteria breve in of the mother's intestine and breast milk can be translated into mammary glands and colonize the baby's intestines. |
| Akagawa et al. (2019)10 | To investigate the effects of prebiotic-rich breastmilk in treating intestinal microbiota dysbiosis | 36 healthy Japanese neonates were obtained at 4 days and 1 month of age | Neonatal stool samples | Cross-sectional | Characterizes intestinal microbiota in neonates according to the mode of delivery and type of food, and reconfirms that neonatal intestinal microbiota born by cesarean initially has a low diversity immediately after birth, and this causes dysbiosis. However, the possible influence of breast milk, even for a short time, increases dysbiosis 1 month after birth. |
| Liu et al. (2019)11 | To determine the single and combined effects of labor, diet and postnatal antibiotic exposure on the initial formation of a baby's intestinal microbiome at 6 weeks postpartum | 120 infants at 6 weeks postpartum | Infant fecal samples | Cross-sectional study | Exclusive breastfeeding can increase the intestinal microbiota of babies, especially in babies born through cesarean delivery. |
| Corona-Cervantes et al. (2020)12 | To evaluate the relationship between breast milk bacteria and mode of delivery with the composition of neonatal intestinal bacteria | 67 healthy lactating women | Breast milk–neonatal stool | A cross-sectional study | Breast milk contributes to 67.7% of bacteria in the first six days postpartum. Breast milk is one of the main sources of bacteria that colonize the neonatal digestive tract since the first days of life. Colonization of the intestine is characterized by high dominance of bacterial taxa, mainly by members of the phyla Firmicutes (Clostridium gasigenes, Streptococcus, Staphylococcus, and Enterococcus), Proteobacteria (Pseudomonadaceae, Sphingomonadaceae, and Bradyrhizobaceace, Actinobacterium). and Bacteroidetes (Bacteroides), which can be transferred through lactation. |
Breast milk is a source of nutrition for babies that contain lots of natural prebiotics that can be transmitted to babies through breastfeeding.9 These good bacteria play an important role in the development and maturation of a baby's immune system. Some bacteria obtained from breast milk such as E. coli, Enterobacteriaceae, Staphylococcus spp., Bacteroides spp., Bifidobacterium spp., Enterococcus spp., and Lactobacillus spp.7,8,10,11 The type of prebiotics in breast milk is not affected by the prebiotic supplementation consumed by the mother.21 However, the amount of prebiotics can be influenced by the consumption of antibiotics during pregnancy or breastfeeding.10 Prebiotic transmission from mother to baby through breastfeeding is most common in infants who are breastfed aged 0–5 days.8 This is in line with the statement that early breast milk or colostrum contains more lactic acid bacteria and Bifidobacterium. Colostrum itself can be immediately given during the early breastfeeding initiation process.
Breastfeeding can prevent babies from developing septicemia, gastroenteritis, bacterial diarrheal pathogens, urinary tract infections, rotavirus infections, necrotizing enterocolitis, allergies, colic/crying, and obesity in infants.9 Besides breastfeeding can also prevent mothers from experiencing acute otitis media. Whereas in newborns with dysbiosis such as premature babies and born by cesarean section, breastfeeding can increase good intestinal micriobium.
ConclusionEarly breastfeeding initiation is very good to reduce the incidence of infant mortality because the provision of early breastfeeding initiation means giving breastfeeding early in life so that it greatly affects the development of good bacterial colonies in infants. The colony of bacteria formed in the baby's intestine that functions as a prebiotic can prevent infection, allergies, colic, and obesity in infants. Because of the many benefits derived from breast milk, it is highly recommended for exclusive breastfeeding and early breastfeeding initiation so that the baby gets colostrum.
Conflict of interestThe authors declare no conflict of interest.
Peer-review under responsibility of the scientific committee of the Technology Enhanced Medical Education International Conference (THEME 2019). Full-text and the content of it is under responsibility of authors of the article.