Las puntuaciones HEART, TIMI y GRACE son herramientas valiosas en la evaluación pronóstica de eventos cardiovasculares tempranos en pacientes con síndrome coronario agudo (SCA). Sin embargo, su uso combinado no ha sido exhaustivamente investigado.
ObjetivosDeterminar el valor pronóstico de la mortalidad intrahospitalaria y a los 6 meses mediante las puntuaciones GRACE, TIMI y HEART en pacientes con SCA.
MétodosRealizamos un estudio descriptivo transversal con seguimiento longitudinal de 68 pacientes con SCA durante 6 meses en el Hospital General Central de Can Tho, Vietnam.
ResultadosLa puntuación GRACE demostró un buen valor pronóstico para la mortalidad hospitalaria (AUC = 0.805, sensibilidad = 90%, especificidad = 65.51%). La puntuación TIMI tuvo un valor pronóstico deficiente para la mortalidad hospitalaria (AUC = 0.682, sensibilidad = 60%, especificidad = 63.79%) y la mortalidad a los 6 meses (AUC = 0.692, sensibilidad = 60%, especificidad = 66.03%). En contraste, la puntuación HEART tuvo un buen valor pronóstico para la mortalidad hospitalaria (AUC = 0.726, sensibilidad = 50%, especificidad = 89.74%) y a los 6 meses (AUC = 0.805, sensibilidad = 57.1%, especificidad = 97.14%).
ConclusiónLas puntuaciones GRACE demuestran un mayor valor pronóstico para la mortalidad hospitalaria en pacientes con síndrome coronario agudo en comparación con las puntuaciones TIMI y HEART.
In recent decades, numerous prognostic models have been developed to assess the risk of mortality in patients with acute coronary syndrome. These models encompass those derived from clinical trials, such as the TIMI score, and models based on multinational registry studies, like the GRACE score. Additionally, there are newly developed scores, such as the HEART score, which has demonstrated high effectiveness in risk stratification of chest pain patients in the emergency department.1,2 Recent studies have indicated that the prognostic value of the GRACE, TIMI, and HEART scores may vary among different populations at risk. While there have been several studies in Vietnam on the prognostic value of the GRACE and TIMI scores,3–5 research on the specific prognostic value of the HEART score in patients with acute coronary syndrome remains limited. Consequently, our study was conducted with the aim of determining the prognostic value of in-hospital and 6-month mortality using the GRACE, TIMI, and HEART scores in patients with acute coronary syndrome.
MethodsStudy design and study populationStudy populationA cross-sectional descriptive study with patients aged 18 years and older diagnosed with acute coronary syndrome, at the Cardiology Department and Interventional Cardiology Unit of Can Tho Central General Hospital from December 2020 to July 2022.
Inclusion criteriaAll patients aged ≥18 years received a definitive diagnosis of acute coronary syndrome,6,7 patients or family members consented to participate in the study.
Exclusion criteriaPatients who were lost to follow-up after discharge and were not followed-up until the sixth month, insufficient variables to assess the risk scores, patients are unable to hear and respond to interviews.
Study objectivesGeneral characteristics of the study populationGender, clinical features of acute coronary syndrome, and the characteristics of the GRACE,8,9 TIMI,10 and HEART11 scores as shown in Appendix A.
Determining the prognostic value of mortality using the GRACE, TIMI, and HEART scores in patients with acute coronary syndromeComparing the prognostic value of the GRACE, TIMI, and HEART scores is achieved by comparing the area under the ROC curve of each pair of scores. The accuracy of the ROC curve area for the 3 scores (GRACE, TIMI, and HEART) is assessed. Model accuracy is evaluated using the Hosmer-Lemeshow test with p > .05 as a well-fitted model and a suitable score to include in the prognostic model. Comparing the prognostic value according to the GRACE, TIMI, and HEART scores by DeLong test to compare the area under the ROC curve of each pair of scales, the difference is statistically significant at p < .05.
Data collection and measurementsData collectionPatients aged ≥18 years admitted to the hospital with a diagnosis of ACS, recorded clinically, medical history, cardiovascular risk factors, laboratory tests at admission, then GRACE, TIMI, and HEART scores were calculated. Patient follow-up during hospitalization involved recording all cases of mortality from any cause. After patient discharge, follow-up was conducted until the sixth month, during which all cases of mortality from any cause were documented (Central Figure).
Data analysisAfter data collection, the collected data were filtered, coded, and analyzed using the statistical software SPSS 22.0 to calculate descriptive statistical features such as frequency and percentage (%). The model's accuracy was assessed using the Hosmer-Lemeshow test, with p-value >.05 indicating a well-fitted model. The DeLong test was used to compare the area under the ROC curve for each pair of scores, and the results were statistically significant at p < .05.
ResultsGeneral characteristics of the study subjectsFemales represent the majority of the study population with 73.5%. Non ST-segment elevation myocardial infarction was the most prevalent clinical presentation, representing 69.1%, while unstable angina had the lowest prevalence at 14.7%. The most common internal medicine treatment approach was conservative management, representing 69.1% (Table 1). The highest rates of in-hospital and 6-month mortality were observed in the group treated with internal medicine and presenting with non ST-segment elevation myocardial infarction (Fig. 1). The majority of in-hospital and 6-month mortality occurred in the high-risk groups according to the scoring systems, with statistically significant differences (p < .05) (Appendix B).
General characteristics of the study subjects.
| Characteristics | n | % |
|---|---|---|
| Female | 50 | 73.5 |
| Age (year) | 76.6 ± 12.8 | |
| Heart rate (beats per minute) | 94.4 ± 16.7 | |
| SBP (mmHg) | 120 (60–190) | |
| Killip classification (%)IIIIIIIV | 3714143 | 54,420.620.64.4 |
| Cardiac arrest on admission | 2 | 2.9 |
| ST changes | 11 | 16.2 |
| Elevated cardiac enzymes | 58 | 85.3 |
| Clinical presentation | ||
| Unstable angina | 10 | 14.7 |
| NSTEMI | 47 | 69.1 |
| STEMI | 11 | 16.2 |
| Treatment approach | ||
| Combined PCI and CABG with internal medicine | 21 | 30 |
| Internal medicine | 47 | 70 |
| Medical history | ||
| Hypertension | 41 | 80 |
| Diabetes mellitus | 22 | 38.6 |
| Smoking | 11 | 19.3 |
| Family history of early-onset cardiovascular disease | 9 | 15.7 |
| Hypercholesterolemia | 26 | 45.6 |
| Previous stenosis of ≥ 50% in the coronary artery | 13 | 22.8 |
| Prior myocardial infarction | 20 | 35 |
| Revascularization of the coronary artery (PCI or CABG) | 6 | 10.5 |
| At least 2 episodes of chest pain within 24 hours before admission | 28 | 49 |
| Use of aspirin in the 7 days prior to admission | 26 | 45.6 |
| Creatinin (mg/dl) | 0.96 (0.47–4.9) | |
| Age ≥ 65 | 50 | 87.7 |
| Anterior myocardial infarction or left bundle branch block | 3 | 27.3 |
| Arrival at the hospital more than 4 hours after symptom onset | 4 | 36.4 |
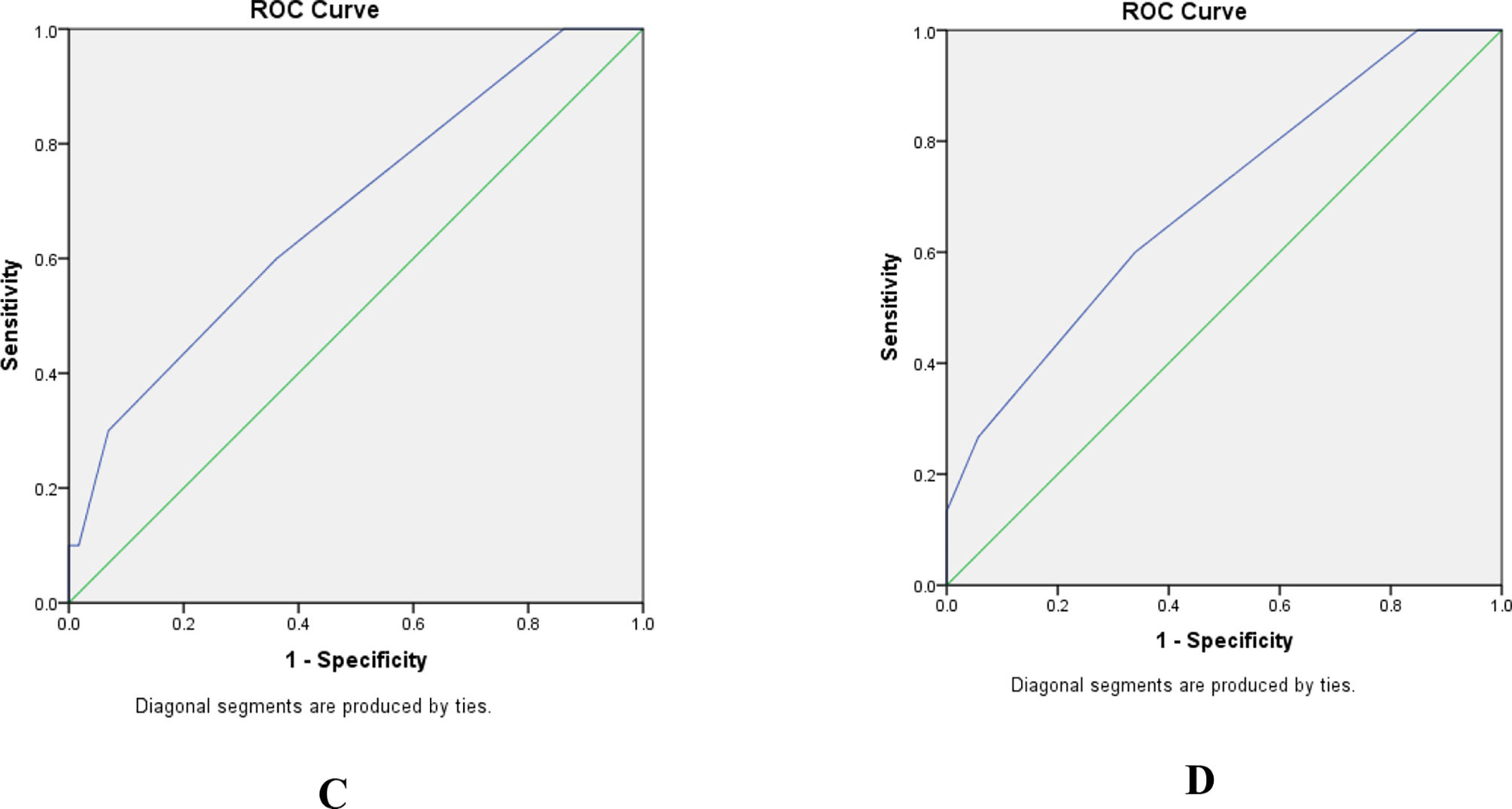
The GRACE score showed a good prognostic value for in-hospital mortality (AUC = 0.805, p = .002) and a quite good prognostic value for 6-month mortality (AUC = 0.786, p = .001) in patients with acute coronary syndrome (Appendix B). The TIMI risk score had a poor prognostic value for both in-hospital mortality (AUC = 0.682, p = .068) and 6-month mortality (AUC = 0.692, p = .024) (Appendix B). The HEART risk score showed a quite good prognostic value for in-hospital mortality (AUC = 0.738, p = .017) and a good prognostic value for 6-month mortality (AUC = 0.825, p < .001) (Fig. 2) and (Table 2).
Prognostic values of the scores for in-hospital and 6-month mortality.
| Score | AUC | 95% CI | p | Cut-off point | Sensitivity | Specificity |
|---|---|---|---|---|---|---|
| In-hospital | ||||||
| GRACE | 0.805 | 0.684–0.927 | 0.002 | 170.5 | 90% | 65.51% |
| TIMI | 0.682 | 0.5–0.863 | 0.068 | 3.5 | 60% | 63.79% |
| HEART | 0.738 | 0.54–0.935 | 0.017 | 8.5 | 50% | 91.37% |
| 6-month | ||||||
| GRACE | 0.786 | 0.675–0.897 | 0.001 | 151.5 | 100% | 49.06% |
| TIMI | 0.692 | 0.541–0.844 | 0.024 | 3.5 | 60% | 66.03% |
| HEART | 0.825 | 0.681–0.97 | <0.001 | 8.5 | 60% | 98.11% |
The Hosmer-Lemeshow test shows that the GRACE score and TIMI score achieved goodness-of-fit for the ACS population, and the HEART score achieved goodness-of-fit for the in-hospital ACS population but not for the 6-month follow-up ACS population (Table 3). The prognostic values of in-hospital mortality for acute coronary syndrome patients were not statistically different between the 2 different scoring systems. The prognostic values of 6-month mortality for acute coronary syndrome patients were not statistically different between the 2 different scoring systems (Table 4).
Comparison of in-hospital mortality prognostic values between TIMI and HEART scores in patients with acute coronary syndrome.
| TIMI | HEART | p | GRACE | HEART | p | GRACE | TIMI | p | |
|---|---|---|---|---|---|---|---|---|---|
| In-hospital mortality | In-hospital mortality | In-hospital mortality | |||||||
| AUC | 0.682 | 0.738 | .497 | 0.805 | 0.738 | .510 | 0.805 | 0.682 | .1759 |
| 6-month mortality | p | 6-month mortality | p | 6-month mortality | p | ||||
| AUC | 0.786 | 0.825 | .639 | 0.692 | 0.825 | .086 | 0.786 | 0.692 | .291 |
In our study population, 73.5% are female, which differs from some other studies3,4 conducted in the Vietnamese population. However, our findings align with studies indicating that gender differences become less significant as age increases.12,13 It's noteworthy that with advancing age, the risk of acute coronary syndrome and related complications tends to increase.14,15 The majority of patients in our study (69.9%) were managed with internal medicine without PCI, similar to the findings in Tan Van Nguyen's study.3 Additionally, our study reported in-hospital and 6-month mortality rates of 14.7% and 22.1%, respectively, which were higher than those reported by foreign authors, such as Keith Fox, with a rate of 19.8%.16,17
Prognostic values of mortality according to the GRACE, TIMI, and HEART scores in patients with acute coronary syndromeThe GRACE score demonstrated a strong ability to differentiate between risk categories for in-hospital and 6-month mortality in patients with non-ST-elevation acute coronary syndrome, consistent with findings from other studies.17-19 In our study, the average HEART score was 7 points, with the high-risk group comprising 55.9% of patients. This finding was similar to the study conducted by Six et al, where the HEART score was 6.51 ± 1.84.20 Our study showed that the in-hospital mortality rate in the high-risk group was significantly higher than in the moderate-risk group (11.8% vs. 2.9% with p = .05). Similarly, the 6-month mortality rate was also higher in the high-risk group compared to the moderate-risk group (19.1% vs. 2.9% with p = .024). Therefore, the HEART score demonstrated a good ability to differentiate between risk categories in predicting both in-hospital and 6-month mortality, which aligns with the study by authors AJ Six, BE Backus, and JC Kelder.20
Regarding in-hospital mortality, the GRACE score exhibited the best prognostic value, while the TIMI score had the lowest prognostic value. The area under the ROC curve for the GRACE, TIMI, and HEART scores was AUC = 0.805, AUC = 0.682, and AUC = 0.738, respectively. However, these differences were not statistically significant when comparing each pair using the DeLong test. Our study results differ from those of authors where the AUC for GRACE, TIMI, and HEART scores were AUC = 0.73, AUC = 0.80, and AUC = 0.86, respectively.21,22 Kao et al.'s study on a group of diabetic patients with non-ST-elevation acute coronary syndrome in Taiwan also showed that the TIMI score had a better predictive ability for major cardiovascular events within 1 year after discharge compared to GRACE (AUC under the ROC curve = 0.74 vs. 0.72). The authors explained that the inferior prognostic performance of GRACE was due to the relatively low number of patients in Killip classes III/IV.23
For 6-month mortality, the HEART score had the highest prognostic value with an AUC under the ROC curve of 0.825, followed by the GRACE score with an AUC of 0.786, and the TIMI score had the lowest prognostic value with an AUC of 0.692. However, these differences were not statistically significant when comparing each pair using the DeLong test. A study by Hang Zhu in a female patient group showed that the GRACE score had a higher prognostic value than TIMI (AUC = 0.81 vs. AUC = 0.68), and the difference was statistically significant.2
We believe that the HEART score has strengths in including various cardiovascular risk factors, such as hypercholesterolemia, hypertension, diabetes, smoking, family history of early coronary artery disease, obesity, and history of coronary artery disease, contributing to its superior prognostic value compared to other scores. Moreover, relying on a minimum number of variables, including clinical history, electrocardiogram, age, cardiovascular risk factors, and cardiac enzymes, makes the HEART score simple and convenient. However, the Hosmer-Lemeshow test results indicated that the HEART score is not suitable for predicting 6-month mortality. Thus, we hope to see further studies in the future to evaluate the role of this score in predicting mortality in acute coronary syndrome patients, particularly at the 6-month mark.
ConclusionsThe GRACE score demonstrated good prognostic value for in-hospital mortality and quite good prognostic value for 6-month mortality. Conversely, the TIMI risk score showed poor prognostic value for both in-hospital and 6-month mortality. The HEART score exhibited quite good prognostic value for in-hospital mortality and good prognostic value for 6-month mortality. However, the results of the Hosmer-Lemeshow test indicated that the HEART score is not suitable for predicting 6-month mortality.
Author contributionConceptualization; Dang Duy Truong, Phuong Kim Huynh, An Viet Tran
Methodology; An Viet Tran, Dang Duy Truong, Toan Hoang Ngo
Software; Toan Hoang Ngo
Formal analysis; Toan Hoang Ngo, Dang Duy Truong
Data curation; Son Kim Tran, Oanh Thi Kim Nguyen
Writing – original draft preparation; Toan Hoang Ngo, An Viet Tran
Writing – review and editing; Toan Hoang Ngo, Dang Duy Truong, An Viet Tran, Oanh Thi Kim Nguyen, Son Kim Tran, Phuong Kim Huynh
All authors have read and agreed to the published version of the manuscript.
FundingToan Hoang Ngo was funded by the Master, PhD Scholarship Programme of Vingroup Innovation Foundation (VINIF), code VINIF.2023.TS.132.
Ethics approvalOur study was approved by the Institutional review board of Can Tho University of Medicine and Pharmacy (Approval number: 2420/QD-DHYDCT, 12/9/2020).
We would like to thank the Rectorate Board of Can Tho University of Medicine and Pharmacy and Can Tho University of Medicine and Pharmacy Hospital for creating favorable conditions for this study to be carried out.
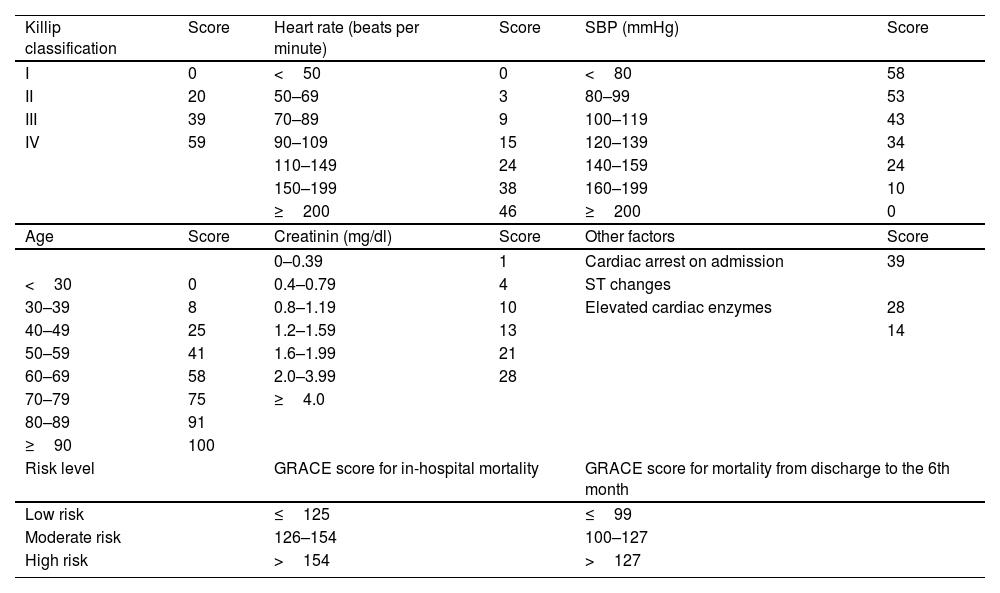
GRACE score in non ST-segment elevation myocardial infarction patients:8
| Killip classification | Score | Heart rate (beats per minute) | Score | SBP (mmHg) | Score |
|---|---|---|---|---|---|
| <50 | 0 | <80 | 58 | ||
| I | 0 | 50–69 | 3 | 80–99 | 53 |
| II | 20 | 70–89 | 9 | 100–119 | 43 |
| III | 39 | 90–109 | 15 | 120–139 | 34 |
| IV | 59 | 110–149 | 24 | 140–159 | 24 |
| 150–199 | 38 | 160–199 | 10 | ||
| ≥200 | 46 | ≥200 | 0 | ||
| Age | Score | Creatinin (mg/dl) | Score | Other factors | Score |
| <30 | 0 | 0–0.39 | 1 | Cardiac arrest on admission | 39 |
| 30–39 | 8 | 0.4–0.79 | 4 | ST changes | |
| 40–49 | 25 | 0.8–1.19 | 10 | Elevated cardiac enzymes | 28 |
| 50–59 | 41 | 1.2–1.59 | 13 | 14 | |
| 60–69 | 58 | 1.6–1.99 | 21 | ||
| 70–79 | 75 | 2.0–3.99 | 28 | ||
| 80–89 | 91 | ≥4.0 | |||
| ≥90 | 100 | ||||
| Risk level | GRACE score for in-hospital mortality | GRACE score for mortality from discharge to the 6th month | |||
| Low risk | ≤108 | ≤88 | |||
| Moderate risk | 109–140 | 89–118 | |||
| High risk | >140 | >118 | |||
GRACE score in ST-segment elevation myocardial infarction patients.8,9
| Killip classification | Score | Heart rate (beats per minute) | Score | SBP (mmHg) | Score |
| I | 0 | <50 | 0 | <80 | 58 |
| II | 20 | 50–69 | 3 | 80–99 | 53 |
| III | 39 | 70–89 | 9 | 100–119 | 43 |
| IV | 59 | 90–109 | 15 | 120–139 | 34 |
| 110–149 | 24 | 140–159 | 24 | ||
| 150–199 | 38 | 160–199 | 10 | ||
| ≥200 | 46 | ≥200 | 0 | ||
| Age | Score | Creatinin (mg/dl) | Score | Other factors | Score |
| 0–0.39 | 1 | Cardiac arrest on admission | 39 | ||
| <30 | 0 | 0.4–0.79 | 4 | ST changes | |
| 30–39 | 8 | 0.8–1.19 | 10 | Elevated cardiac enzymes | 28 |
| 40–49 | 25 | 1.2–1.59 | 13 | 14 | |
| 50–59 | 41 | 1.6–1.99 | 21 | ||
| 60–69 | 58 | 2.0–3.99 | 28 | ||
| 70–79 | 75 | ≥4.0 | |||
| 80–89 | 91 | ||||
| ≥90 | 100 | ||||
| Risk level | GRACE score for in-hospital mortality | GRACE score for mortality from discharge to the 6th month | |||
| Low risk | ≤125 | ≤99 | |||
| Moderate risk | 126–154 | 100–127 | |||
| High risk | >154 | >127 | |||
The TIMI score in Non ST-segment elevation myocardial infarction patients.10
| Factors | Score | |
|---|---|---|
| - Age ≥65 years old. | 1 | |
| - Presence of at least 3 of the following risk factors: high blood pressure (blood pressure ≥140/90 mmHg) or currently on antihypertensive medication, diabetes mellitus, smoking, hypercholesterolemia, family history of premature coronary artery disease (men ≤55 years old, women ≤65 years old). | 1 | |
| - Previous coronary artery stenosis ≥50%; for patients without coronary angiography results, if there is a history of non-invasive cardiac testing (NMCT) or a previous percutaneous coronary intervention (PCI) or coronary artery bypass surgery, it will be considered as 1 point. | 1 | |
| - ST-segment changes ≥0.5 mm at the time of admission. | 1 | |
| - Experienced at least 2 episodes of chest pain within the 24 h prior to admission. | 1 | |
| - Used aspirin within 7 days prior to admission. | 1 | |
| - Elevated cardiac enzymes. | 1 | |
| Total | 07 | |
| Low risk: 0–2 points | Moderate risk: 3–4 points | High risk: 5–7 points |
TIMI score in ST-segment elevation myocardial infarction patients.10
| Factor | Score | |
|---|---|---|
| Age 65–74 | 1 | |
| Age >75 | 2 | |
| History of prior coronary artery disease (CAD)/coronary artery bypass graft (CABG)/angina | 1 | |
| Systolic blood pressure <90 mmHg | 3 | |
| Heart rate >100 beats per minute | 2 | |
| Killip class II–IV | 2 | |
| Body weight <67 kg | 1 | |
| Anterior ST-segment elevation myocardial infarction (STEMI), left bundle branch block | 1 | |
| Arrival at the hospital more than 4 h after symptom onset | 1 | |
| Total score | 14 | |
| Low risk: 0–3 points | Moderate risk: 4–6 points | High risk: >6 points |
The HEART score.11
| Transformation | 0 points | 1 points | 2 points |
|---|---|---|---|
| Medical history | Non-typical angina | Atypical angina | Typical angina |
| Electrocardiogram | Completely normal | Nonspecific ST-T wave changes | Significant ST-segment deviation |
| Age | <45 | 45–64 | Age ≥65 |
| Risk factors (elevated blood cholesterol, high blood pressure, diabetes mellitus, smoking, family history, obesity) | 1–2 risk factors | ≥3 risk factors or history of coronary artery atherosclerosisa | |
| Troponin | Within normal limits | Elevated 1–3 times above normal limits. | Elevated more than 3 times above normal limits. |
| Total score: 10 points | |||
| Low risk: 0–3 points | Moderate risk: 4–6 points | High risk: 7–10 points | |
Mortality rates according to the risk categories of the GRACE, TIMI, and HEART scores.
| Score | Mortality | Low risk | Moderate risk | High risk | p |
|---|---|---|---|---|---|
| GRACENSTEMI | In-hospital | 0% | 0% | 14% | .027 |
| 6-month | 0% | 0% | 21.1% | .024 | |
| GRACESTEMI | In-hospital | 0% | 0% | 18.2% | .22 |
| 6-month | 0% | 0% | 27.3% | .54 | |
| TIMINSTEMI | In-hospital | 0% | 10.5% | 3.5% | .056 |
| 6-month | 0% | 17.5% | 3.5% | .209 | |
| TIMISTEMI | In-hospital | 0% | 9% | 9% | .114 |
| 6-month | 0% | 9% | 18% | .248 | |
| HEART | In-hospital | 0% | 2.9% | 11.8% | .05 |
| 6-month | 0% | 2.9% | 19.1% | .024 |