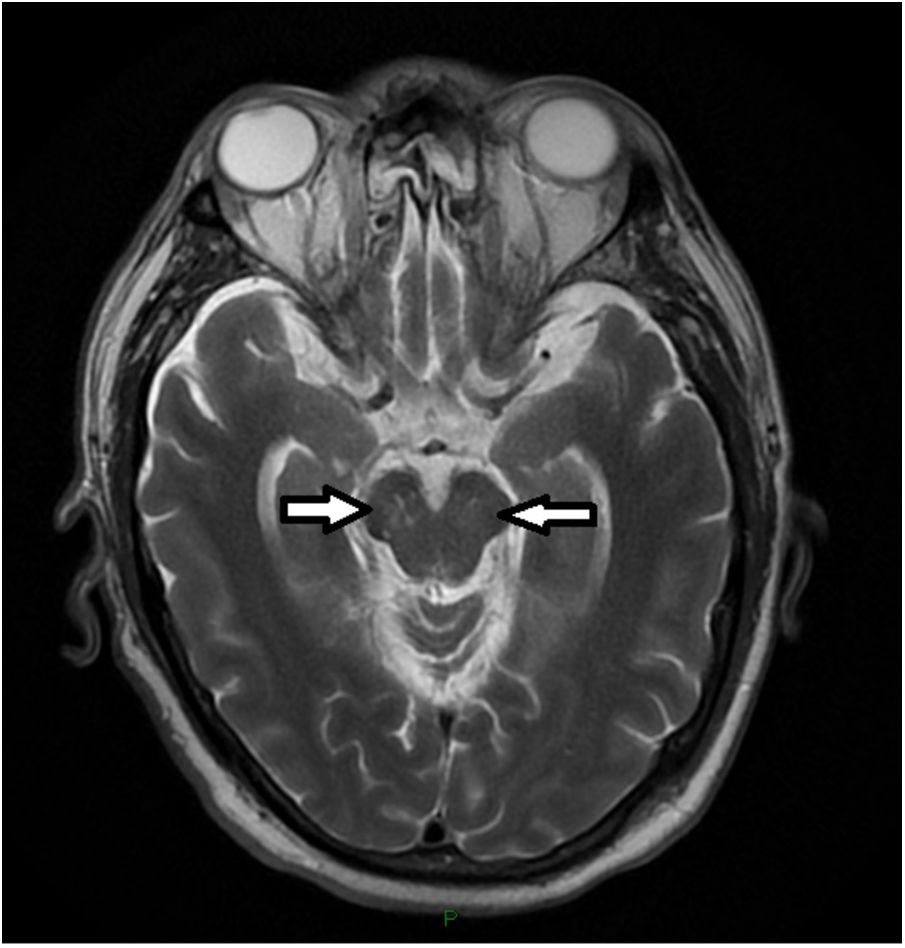
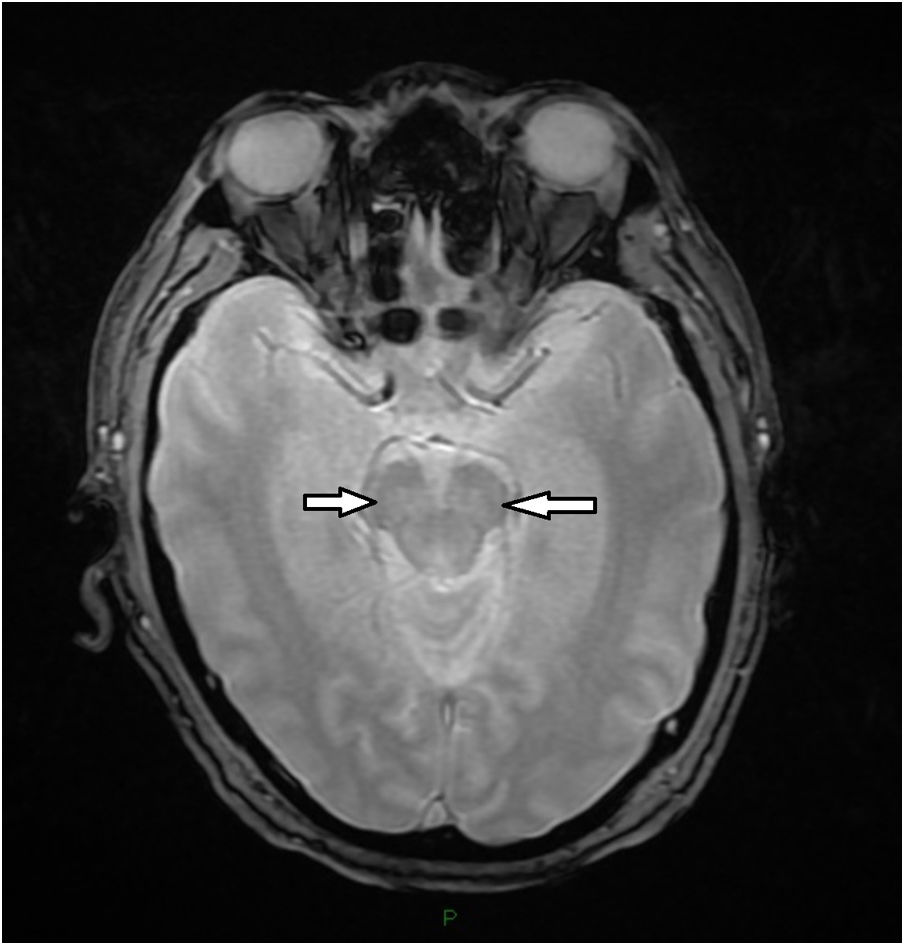
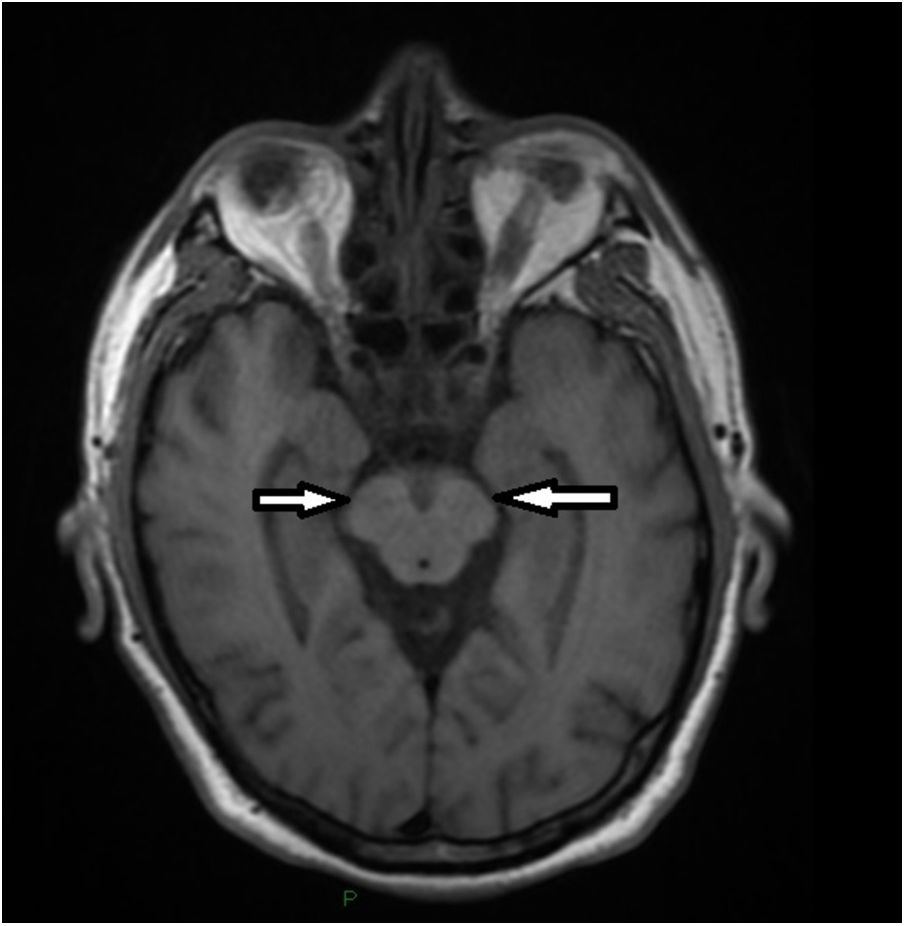
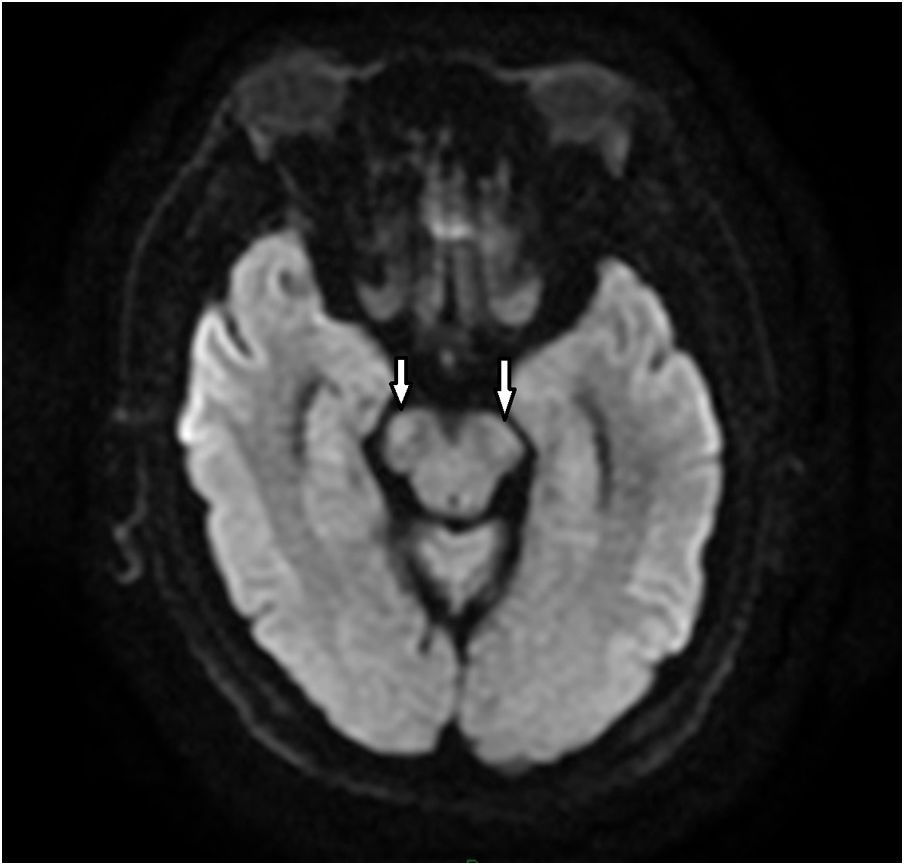
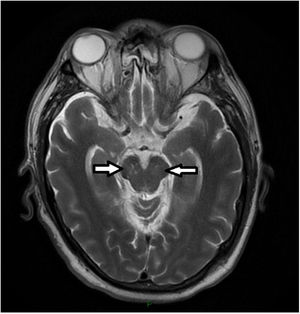
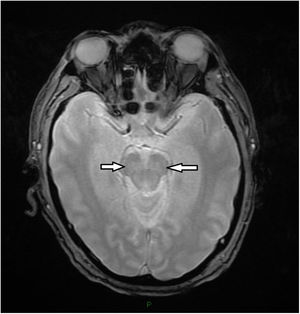
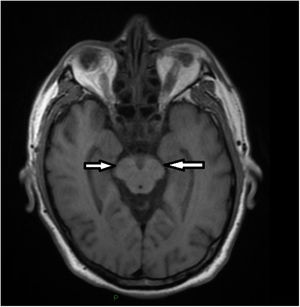
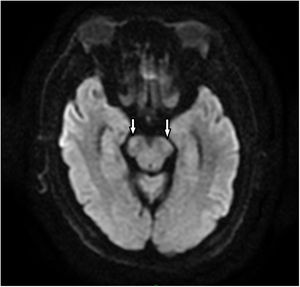
A 59-year-old male was admitted to emergency room after 4 days of flu-like syndrome, 2 days later presented bilateral ascendant weakness in lower limbs then in upper limbs. He was received with anisocoria, ophthalmoparesis and consciousness impairment. Tracheal intubation was performed and he was monitoring in ICU. We performed an MRI showing multiple lesions in midbrain white substance in T2 (Fig. 1), GRE (Fig. 2), T1 (Fig. 3) and DWI (Fig. 4). Nerve conduction study was performed, with moderate impairment in 4 limbs with axonal impairment with secondary demyelinating damage and lumbar punction showed mild hyperproteinoraquia mild pleocytosis and PCR negative for Epstein-Barr virus, Citomegalovirus, adenovirus, herpes simplex 1 and 2, varicella-zoster virus, enterovirus, paraechovirus, herpes virus 6 and 7 and parvovirus B19. Suspecting Bickerstaff encephalitis (BE) plasma exchange started with consciousness improvement after fourth session. After 7 days the patient was discharged by ICU, with slow but good recovery then managed as outpatient.
BE diagnosis used to be consider in a Guillain Barre Syndrome (GBS) context, it is common that BE, Miller-Fisher and GBS overlap to each other making a difficult challenge to diagnosis. Blood-brain Barrier disruption leading into pathologic antibodies cross into brainstem and damage this structure had been proposed to explain either clinical features and MRI white matter changes. Treatment is the same to GBS. Ophthalmoparesis and weakness may persist for weeks as a severe GBS would evolve.
FundingNone.
Conflicts of interestNone.