A 66-year-old woman presented to her Family Doctor with a few weeks’ history of chest pain (mostly right side), dyspnea during medium efforts and fatigue. She denied other symptoms including gastroesophageal reflux symptoms.
Past medical history included arterial hypertension, dyslipidaemia, obesity, systemic lupus erythematosus, depression and pulmonary emphysema. Her chronic disease medication included omeprazole 20mg, losartan 50mg, lercanidipine 10mg, furosemide 40mg, rosuvastatin 50mg, hydroxychloroquine 400mg, prednisolone 20mg, cyclosporine 100mg, fluoxetine 20mg, quetiapine 25mg and alprazolam 0.5mg.
Due to the described symptoms, an electrocardiogram, an echocardiogram, a chest X-ray and blood tests were requested.
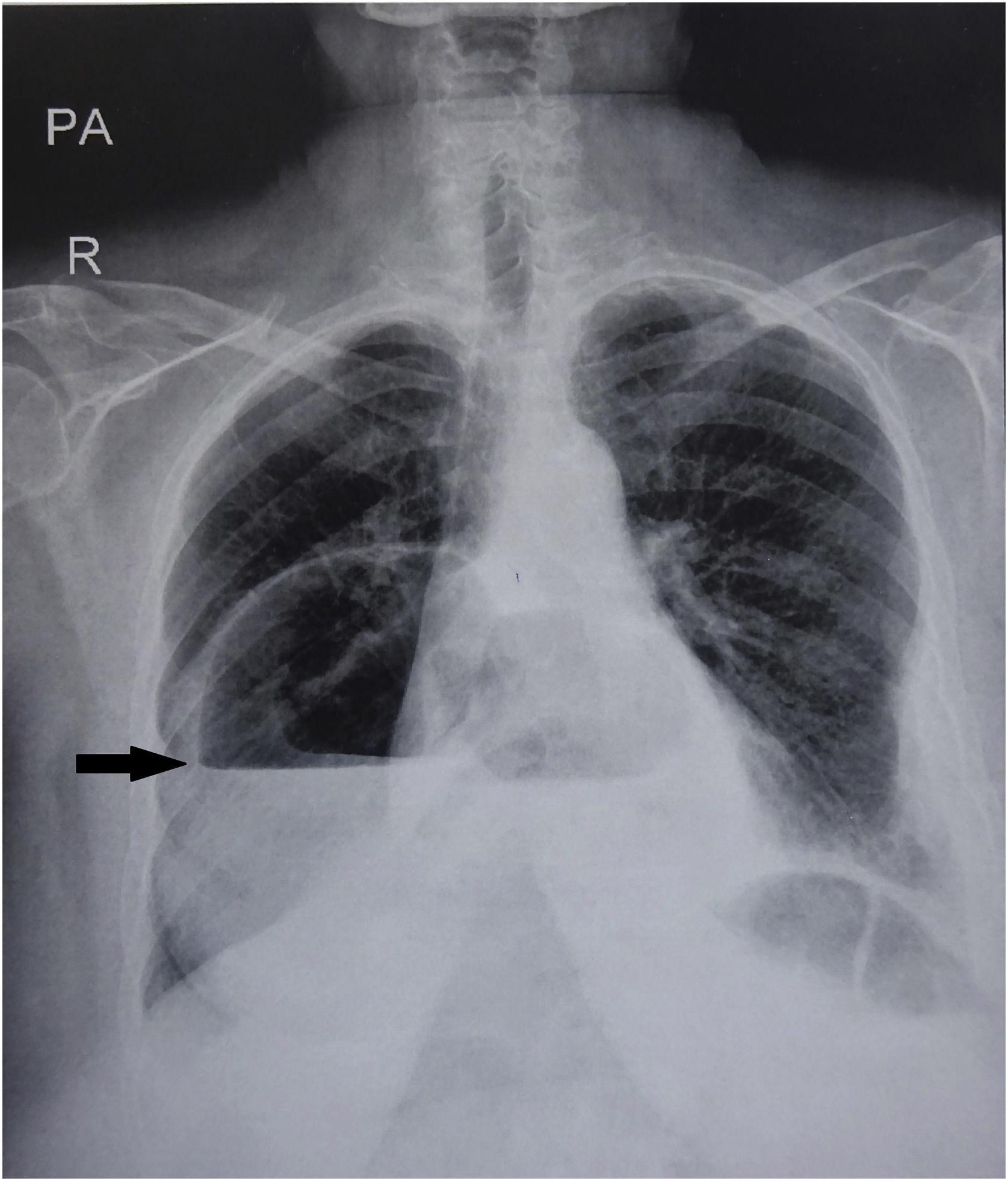
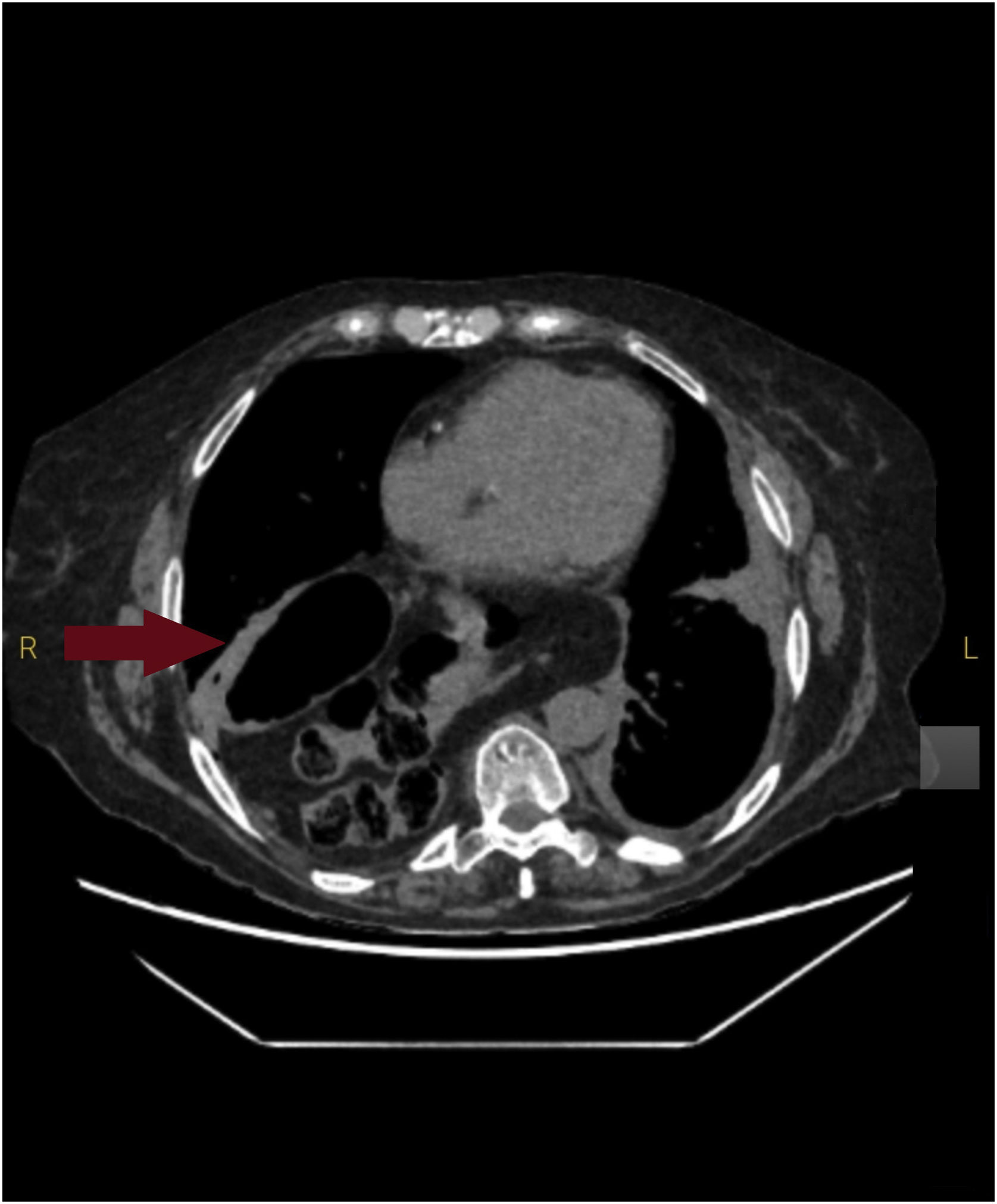
The electrocardiogram, echocardiogram and blood tests were normal. The chest radiography requested showed a large hypotransparency on the right hemithorax with an air–liquid shadow in retrocardiac position (Fig. 1). Computed tomographic scan confirmed a large hiatal hernia, containing the stomach and part of the transverse colon in posterior–inferior position of the right hemithorax, with right lower lobe atelectasis (Fig. 2).
The patient underwent laparoscopic surgery for reinforced diaphragm closure. Clinical improvement was noted after the procedure.
Hiatal hernia involves herniation of the contents of the abdominal cavity, through the diaphragm into the mediastinum.1 Cases of complete stomach herniation plus transverse colon are uncommon.2 This condition is usually associated with typical gastro-oesophageal reflux symptoms such as heartburn (described as a painful burning feeling in the chest, often after eating), regurgitation of food or liquids into the mouth, postprandial fullness, halitosis or difficult swallowing.1,3 Chest/abdominal pain and shortness of breath have also been described.
In the present case, the stomach and part of the transverse colon were located in the mediastinum, so the clinical presentation included rarer symptoms such as dyspnea and fatigue. Although the causes of hiatal hernia are not known, there are major risk factors: over 50 years old and obesity.1,3
In this case, it was documented in previous health center records that a hiatal hernia had been identified, however, clinical images were not available for consultation. Moreover, information regarding the size or more specific details about this hernia were not written in previous medical records.
Due to the patient's clinical history of lupus erythematosus, she has been treated mostly in hospital consultations: Autoimmune Diseases, Pulmonology and Psychiatry. Regarding her clinical history of pulmonary emphysema, she went previously to specific pulmonary emphysema consultations, nevertheless, she lost follow-up after the COVID-19 pandemic. Besides going to consultations at the public reference hospital, this patient also has access to private health care, which she uses frequently. In either case (reference hospital or private hospitals), the Family Doctor has very limited access to those records or diagnostic tests using the health center informatic system. This explains why recent X-rays were not accessible to her Family Doctor and the lack of access to hospital information could be considered a limitation in the initial management of this case.
With that being said, it is possible that this giant hiatal hernia had already been image documented at hospital X-rays, however it was not given much importance to explain the patient's symptoms, always attributed to her pulmonary emphysema and lupus disease. Point out that the absence of typical symptoms such as heartburn or regurgitation could be explained by the fact that the patient takes proton pump inhibitors daily (no formal indication was found in her medical records).
In this case, we believe that the Family Doctor played an important role by listening to this patient's symptoms and seeing her as a whole, considering alternative diagnosis.
This clinical case aims to draw attention to an atypical presentation of hiatal hernia and to reinforce this hypothesis into the differential diagnosis.
Ethical considerationsInformed written consent was obtained.
FundingNo funding was received for this work.
Conflict of interestThe authors declare that they have no competing interest.