This study has been carried out to test the clinical hypothesis of personal smell as a hint to the diagnosis of narcoleptic patients.
MethodsSweat samples from narcoleptic and healthy controls were tested independently by two trained dogs and their positive or negative detection compared to the gold standard diagnosis for narcolepsy. Neither trainer nor dog knew the source of the sample selected or its placement in the search device.
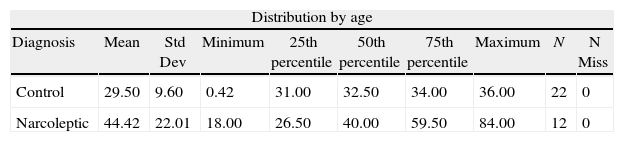
Twelve narcoleptic patients, both sexes and various ages, recruited from April 2011 to June 2012 and diagnosed according to standard criteria, through their clinical records and nocturnal polysomnography plus multiple sleep latency test, made up the patient group. The control group was made up of 22 healthy volunteer without sleep disorders, both sexes and various ages.
Sweat samples from both patients and controls were collected following the same protocol to avoid contamination, and tested independently by two trained dogs.
ResultsEleven narcoleptic were detected positive by the dogs while only three controls.
ConclusionIt seems that narcoleptic patients have a distinct typical odor that trained dogs can detect. The development of olfactory test could be a useful method in the screening of narcolepsy while opens a new research area.
El propósito de este estudio es probar la hipótesis de un olor corporal característico en narcolepticos como indicador de diagnóstico.
MétodosSe testan muestras de sudor de 12 narcolepticos y 22 controles sanos de forma independiente por dos perros entrenados y su detección, positiva o negativa, se compara con el diagnostico “gold standard” de narcolepsia. Ni adiestrador ni perros conocían el tipo de muestra seleccionada o su emplazamiento en el dispositivo de búsqueda.
12 pacientes con narcolepsia, de ambos sexos y distintas edades, reclutados entre abril de 2011 y junio de 2012, y diagnosticados de acuerdo a criterios estándar, a través de su historia clínica y polisomnografía nocturna seguida de test de latencia múltiple del sueño, conforman el grupo de pacientes. El grupo control está formado por 22 voluntarios sanos, de ambos sexos y distintas edades, sin trastorno del sueño.
Las muestras de sudor, tanto de pacientes como de controles, se recogieron siguiendo el mismo protocolo para evitar contaminación y fueron testadas de forma independiente por dos perros entrenados.
Resultados11 narcolepticos son detectados positivamente por los perros frente a solo 3 controles sanos.
ConclusiónParece que los pacientes con narcolepsia tienen un olor corporal típico que perros entrenados pueden detector. El desarrollo de un test de olfato para el diagnostico de narcolepsia abre nuevas áreas de investigación.
Narcolepsy is a primary sleep disorder characterized by excessive daytime sleepiness, sleep attacks, cataplexy, and sleep paralysis with hypnagogic hallucinations. REM sleep and sleep continuity variables are also disturbed in narcoleptic patients1. The etiology of narcolepsy in humans is unknown, although it gives great importance to the role of the orexin/hypocretin system, both in animals and humans2,3. The prevalence of narcolepsy is 1/2000 in the general population4 and the diagnosis is based on clinical data and polysomnographic studies. There are also some reports of narcolepsy symptoms associated to organic lesions such as mid-brain tumors, pontine gliomas, hypothalamic gliosis5,6, and Down syndrome7.
Various members of our team perceived that the narcoleptic patients have a different characteristic personal smell. Odors have been used as indicators of diseases dating back to traditional medicine8,9, evaluating different organic secretions. In 1837 the production of benzaldehyde was identified in microorganisms10. In 1876 the odor from infected wounds was correlated with laboratory anthrax culture11. In 1923 were demonstrated odors associated with cultures of Pseudomonas aeruginosa and Mycobacterium tuberculosis12. The use of olfactory senses as a diagnostic tool has been used for many years in pathologies like hepatic failure, uremia, ketonemia, metabolic diseases in children, typhus, acromegaly, ingestion of chemical products, schizophrenia, and phenylketonuria13,14.
Smell is the primal sense that allows most organisms to detect predators, food, mate, and so to perpetuate the species. Through smell most organisms create an internal representation of the external world by mechanisms to recognize sensory information of the environment15. The sensory olfactory input is very well defined by chemicals with a precise molecular structure16. Odors contain various complex combinations of volatile chemical products in the urine, breath, blood, vaginal secretions, and sweat16,17. Dogs can be trained to detect any odorous substance even in the presence of other interfering odours18. The dogs can detect the smallest quantity of substances with very different forms, molecular sizes and molecules with very small stereoisomeric differences19,20. The olfactory capacity of dogs is superior to all mammals and is possibly a million times superior to humans.
Actually there is an increasing use of trained dogs for detection, recognition, and localization of odors. The ability of the dogs is influenced by environmental, behavior, and genetic factors18, being the handler's opinion fundamental for good scent detection21. Numerous clinical studies based on scent detecting have been done with tumors and infections with a level of sensibility and specificity near 100% in melanomas22, in lung and breast CA23, in ovaries24, in the screening of colon cancer25, and other tumors26.
Based on the capacity of trained dogs to detect different odors and with the clinical impression that narcoleptic patients have a different odor, this study has been carried out to test the clinical hypothesis of personal smell as a hint to the diagnosis of narcoleptic disease.
MethodsFollowing the criteria of the American Academy of Sleep Medicine27, the patients were diagnosed through their clinical records and nocturnal polysomnography followed by the Multiple Sleep Latency Test (MSLT). The control group was made up of healthy individuals, both sexes and various ages, who completed a sleep questionnaire to rule out sleep disorders, suspicion of narcolepsy, or other sleep pathologies. Patients were enrolled in the study from April 2011 to June 2012. All the patients and control group participants signed an informed consent.
Sweat collectionThe samples from both patients and controls were collected according the following protocol: wash the hands and forearms for 30s with non-perfumed soap (water, vegetable glycerin, coconut, corn syrup soap, alcohol, citric acid, vegetable vitamin E, nothing else); rise hands and forearms in water for 2min; air dries the hands for 2min; rub the palms of the hands on the forearms for 5min; while walking for 10min, rub gauze in the palms of the hands, forearms and arms; introduce the gauze into the vial and close with the septum; identify the sample (sex, age, date of collection) and keep the sample refrigerated at 5°C until resend for the test provided in the course of 24h.
To avoid contamination, only the patients and controls came into contact with materials used to take the sample (vial, septum, tweezers, and gauze). Before taking the sample the candidates had to avoid the use of perfumes, fragrances, deodorants, tobacco, or any source of external contamination. Sterile surgical cotton gauzes were used.
Dogs and trainingTwo four-year-old dogs, one male named “Kuns”, and one female “Coca”, Labrador retrievers, were chosen for the detection instead of just one, as were done in other published clinical trials, in order to obtain greater accuracy in the odor identification. We thought agreement between dogs would help to further generalization of the dogs’ tests results.
Both dogs belong to the Civil Guard, an armed institution of military nature whose main mission is to ensure the full exercise of rights and freedoms and to vouch for public safety28. Its Cynological Service (SECIR) was created in 1951 for the training and use of dogs in searching for missing persons, intervention in disasters, location of drugs or explosives, mountain rescues, and so on. This service conducted all the dogs training and completed the detection test for all samples submitted.
Coca was trained in drug detection (active detection) and Kuns in the detection of explosives (passive detection). In active detection Coca detects a specific odor and moves, using paws and nails waiting to receive her reward. In the passive detection Kuns, in front of a specific sample demonstrates an inhibition in arousal and movements, and adopts a seated position to receive his reward.
The training method for the detection of the suspected specific odor in narcoleptic patients was as follows: breeds of medium size retrievers (Kuns and Coca) with strong olfactory senses and socialized to adapt to the intervention locations. The dogs were exposed to the odor of narcoleptics (the two first) using gauze soaked in their sweat until the dogs associated the rewards with the odor and demonstrated they could discriminate between other samples of odorants and sweat soaked gauze from the healthy control group. The dogs were trained to search and identify odors, utilizing a guide with a leash or away from the guide without a leash.
To improve the procedure a vertical cabinet with eight boxes was designed to contain the sweat soaked gauzes of patients, healthy control group and other substances to dogs for identification. One positive sample was provided among seven others used as controls, each in a separate box. For each particular testing the samples were changed and each box was cleaned with alcohol prior to their use. Neither dog nor handler knew the location of the sample.
The dogs worked in a 6m× 9m room. The cabinet was made of formic lined agglomerate panel that measures 366cm× 91cm and 2cm thick hanging perpendicular to the floor on metal legs. It has four holes, 7.5cm in diameter, which are separated by 88cm and are 57.5cm from the floor. The division of the last hole at the end of the panel is 44cm, which can be linked to the other panel to maintain the distance (88cm) with the other holes. In the back of the panel there are four boxes with lids. Their placements coincide with the holes on the other side. The panels are attached by wooden screws and measure 30cm wide×20cm deep×20cm tall. As already mentioned, active and passive detection was used, each dog used a specific method. The dogs training were completed during March and April 2011.
TestsThe tests were performed between April 2011 and July 2012. New samples, from patients and the control group, were used for each test. The dogs would pass by the boxes only once. A maximum of two tests were done daily with different samples. It was a double blind test (neither trainer nor dog knew the type of samples selected nor its placement in the search device), with a double test by the dogs (each sample was analyzed independently by each dog) using two different approaches of detection (active and passive). The dogs were always under veterinary supervision, in perfect health and injury free.
Statistical analysisDescription is made of the distribution of the variables of age, gender and tobacco habit among patients and controls. A change corrected index of change corrected agreement between the two raters (dogs) was undertaken through Kappa coefficient (CI 95%).
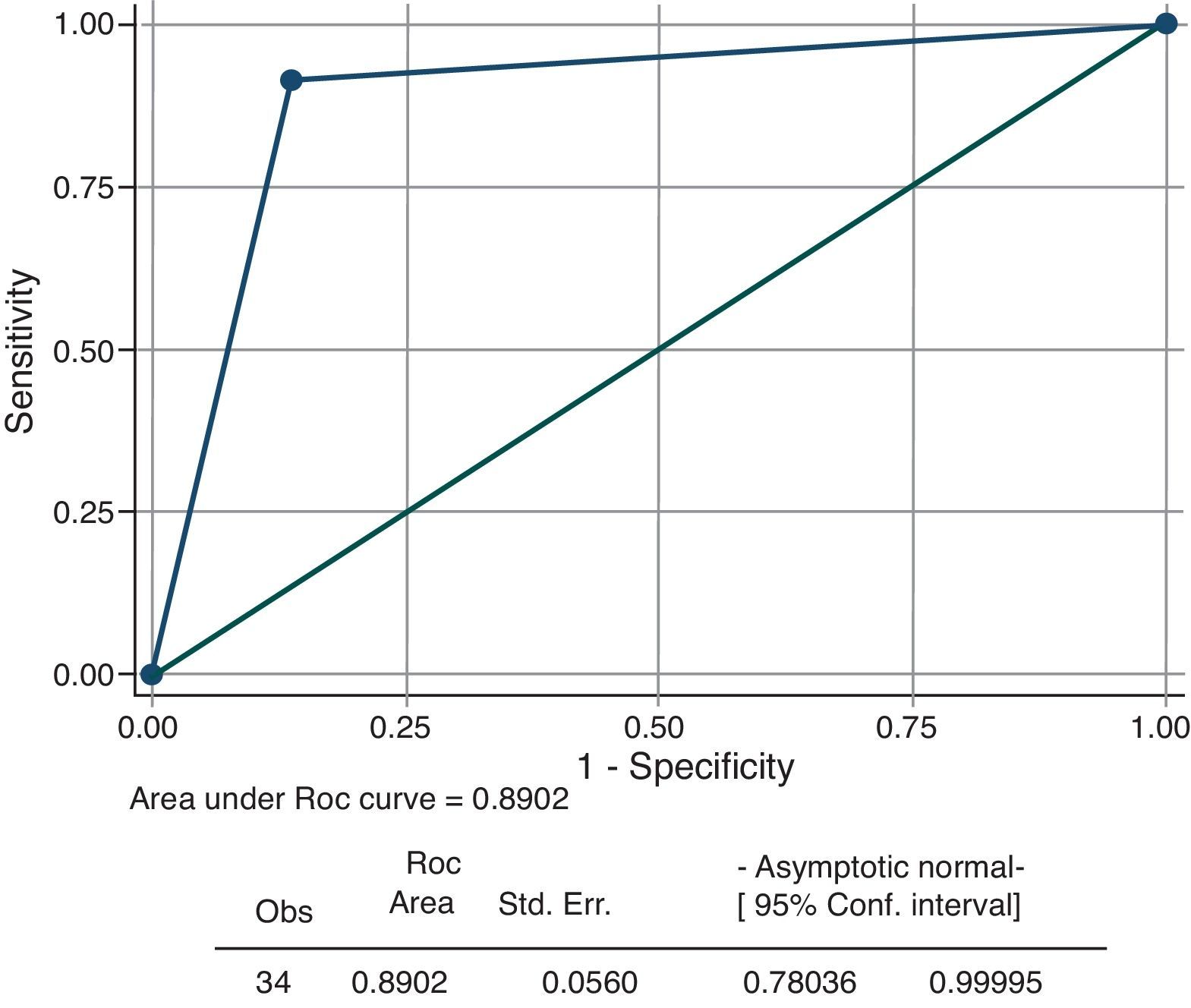
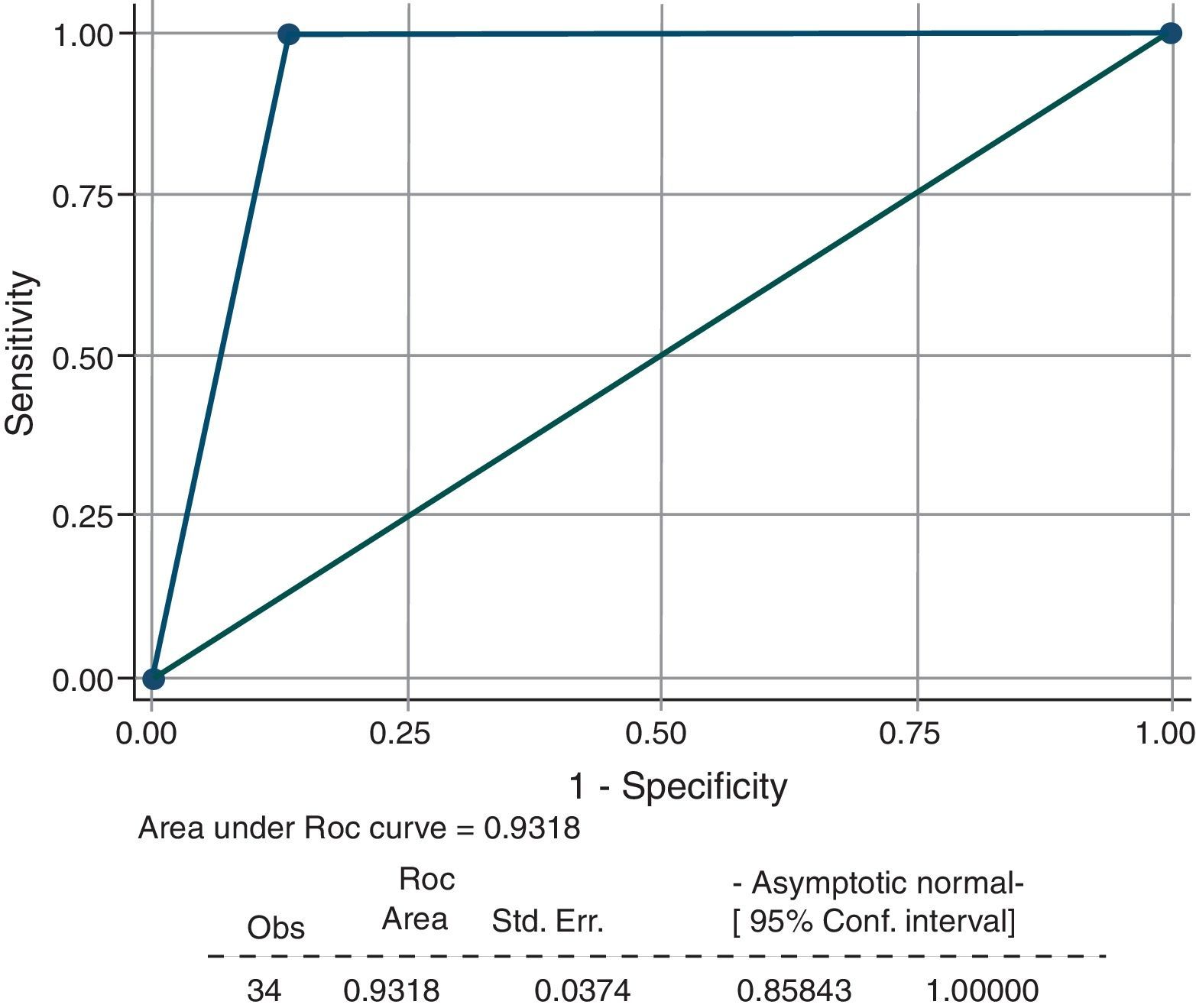
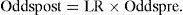
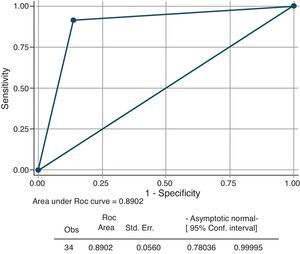
Since both tests, problem (detection by dogs) and reference (gold standard diagnosis) have a binary distribution, analysis of the operational characteristics of the problem diagnosis test are to be conducted by using a 2×2 matrix. Estimates on sensitivity (Se), specificity (Sp), and positive and negative predictive values (PPV, NPV), with 95% confidence intervals, will be performed. A joint evaluation of the behavior of Se and Sp will be performed by means of a ROC curve, whose area below the curve represents the likelihood that, when applying the test to two subjects taken at random, one patient and another a control, may be suitably identified.
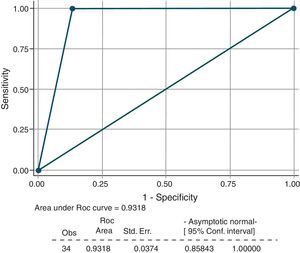
In order to control the effect of the prevalence of narcolepsy in the series studied and to generalize the results of the diagnostic estimators in different clinical situations, the likelihood ratios (LR) will be calculated as an alternative way to describe the performance of a diagnostic test. The LR− can be used to calculate the probability of disease after a positive or negative test. The LR+, likelihood ratio of a positive result [Se/(1−Sp)], express how many times more likely a positive test result is to be found in narcoleptics compared with controls. The LR−, [(1−Se)/(Sp)], express how many times less likely a positive test result is to be found in narcoleptics compared with controls. The initial clinical probability (pre-test probability, pPre) heuristically established by the doctor (extent of clinical suspicion) is modified (post-test probability, pPost) depending on the efficacy of the diagnostic test in accordance with the function:
Odds is a ratio of two probabilities and a convenient way of expressing probability (p) for certain mathematical calculations. The two can be interconverted using simple formulas: Odds=[(p/1−p)] and p=[Odds/(1+Odds)].
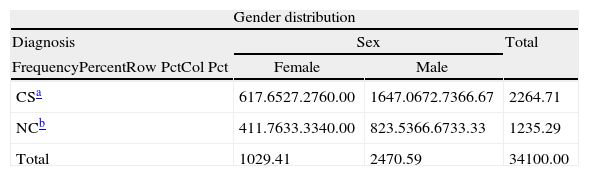
ResultsThirty-four subjects have been studied, 12 narcoleptic and 22 healthy controls. Median age of the series was 33.36 in patients and 33 in controls. 68% of cases were men, which was distributed as 62% in patients and 73% in controls. The frequency of smokers in series, and in cases and controls, was 26, 23, and 31%, respectively. For more details, see Tables 1 and 2.
The Kappa index was 0.94 (0.83–1.00 CI 95%).
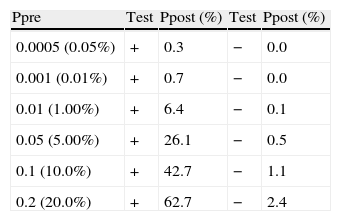
The basic operational diagnostic characteristics obtained in the experiment (CI 95%) are: sensitivity 0.92 (0.72–1.00), specificity 0.86 (0.70–1.00), PPV 0.79 (0.54–1.00) and NPV 0.95 (0.83–1.00). The area under the ROC curve (Receiving Operator Characteristic Curve) is 0.89 (0.78–0.99 CI 95%). The likelihood ratio of a positive test and negative test is 6.72 (2.32–19.51) and 0.10 (0.01–0.63) respectively. Table 3 shows an analysis of sensitivity of the post-test probabilities obtained for positive and negative results in the test, in different situations of clinical suspicion (pre-test probability). The first line shows the estimated population prevalence of narcolepsy in the European general population.4 If the test result is positive, the initial probability estimates that the patient observed may in fact have narcolepsy increases up to 0.3, 0.7, 6.4, 24.6, 26.1, 42.7 and 62.7%, respectively. If the test proves negative, this decreases to 0.0, 0.0, 0.1, 0.5, 1.1 and 2.4%, respectively (Figs. 1 and 2).
Analysis of sensitivity of the post-test.
| Ppre | Test | Ppost (%) | Test | Ppost (%) |
| 0.0005 (0.05%) | + | 0.3 | − | 0.0 |
| 0.001 (0.01%) | + | 0.7 | − | 0.0 |
| 0.01 (1.00%) | + | 6.4 | − | 0.1 |
| 0.05 (5.00%) | + | 26.1 | − | 0.5 |
| 0.1 (10.0%) | + | 42.7 | − | 1.1 |
| 0.2 (20.0%) | + | 62.7 | − | 2.4 |
Ppre: Pre-test probability; Test: test result; Ppost: post-test probability.
The results obtained in the study show that the patients with narcolepsy give off a specific odor that can be detected by animals with a high olfactory ability that have been duly trained.
The diagnostic indices are high, although due to the limited size of the sampling, broad confidence intervals are noted. The study results point to a high discriminatory capacity of the test, particularly when the result is negative. When detection by smell is negative, the post-test probability that the patient has narcolepsy decreases to clinically irrelevant values. When detection by smell is positive, the probability that the patient has narcolepsy increases, but not to clinically sufficient levels such that the diagnosis needs to be confirmed by other means, in accordance with gold standard criterion.
Out of the 22 healthy controls, 3 cases of false positives were detected for narcolepsy. Clinically re-evaluated and tested with polysomnography, narcolepsy was discarded. This false positive might be due to environmental, physiological or pathological situation in said controls, unknown at the time.
In clinical practice, it is not easy to achieve well-trained dogs to give a diagnosis of a specific pathology based on their olfactory capacity, in view of the time taken up in training each dog in a given smell. In the study, attention is focused on the high consistency in detecting a specific smell found between the two dogs, thus showing their excellent capacity for targeted training, although their duration over time is limited by their biological status. For these reasons, it is necessary to develop a method able to identify specific volatile organic compounds (VOCs) deriving from the narcoleptic patient, by means of electronic sensors able to substitute dogs ability29,30. Once narcolepsy VOCs had been identified by chemical analysis, they would have to be compared using dog detection.
The strengths of the study reside in the fact that this is a prospective design with the consecutive compilation of cases, where the diagnosis of narcolepsy is made in accordance with the current clinical standards and is reproducible, since both dogs behave in a similar manner as to their ability to discriminate. Patients have been recruited in common clinical practice and express the full spectrum of the disease, as in any Sleep Medicine center. Selection and work-up biases are dismissed, since the diagnosis of the disease is prior to performing the problem test (detection by smell). Indeed, there is a relative weakness in the study based on the size of the sample. Future replications with larger samples of narcoleptic patients would help to examine the robustness of the current results.
The diagnostic use of the test would be important in the initial differential diagnosis in the study of hypersomnias, since their negativity would avoid more costly studies. It would be important as a means of screening for studying populations or groups requiring diagnosis of narcolepsy. Its application is interesting in cases where hypersomnia could be hazardous, as in the case of drivers, pilots and in professions involving risk. It may be a useful means for making a differential diagnosis of narcolepsy with other sleep related pathologies, such as type 1 myotonic dystrophy (Steinert's disease)31,32. For all that, the hypothesis that the odor test could be used to screen individuals or groups suspected of narcolepsy or hypersomnia, with the provision that accessibility to the test and the cost would allow this, needs to be further validated.
In summary, diagnosis with the olfactory tests is a useful method for diagnosing narcolepsy and opens up a new future for researching the disease with the use of VOCs. This diagnostic technique would reduce costs and would help to make a better selection of patients that should be studied with more complex tests. Furthermore, it would be a useful means of screening for the study of narcolepsy in risk populations. These initial findings can open up the way for developing new, broader based studies that would improve the knowledge of narcolepsy.
Conflict of interestThis was not an industry-supported study. All the authors have indicated no financial conflicts of interest. Neither the authors nor their institutions have financial or personal relationships with other people or organizations that could inappropriately influence their actions. All the authors here state that there is neither conflict of interest nor financial interest.
The authors would like to thank the Civil Guard in general and specially to the Cynological Service for his contribution regarding the dog's training and completion of the detection test for all the samples submitted. They have made this study possible.