To compare the effects of physical activity on improving health-related quality of life (HRQOL), six minutes walking test (6MWT), and oxygen consumption (VO2) peak before and during Coronavirus disease (COVID-19) in patients with heart failure.
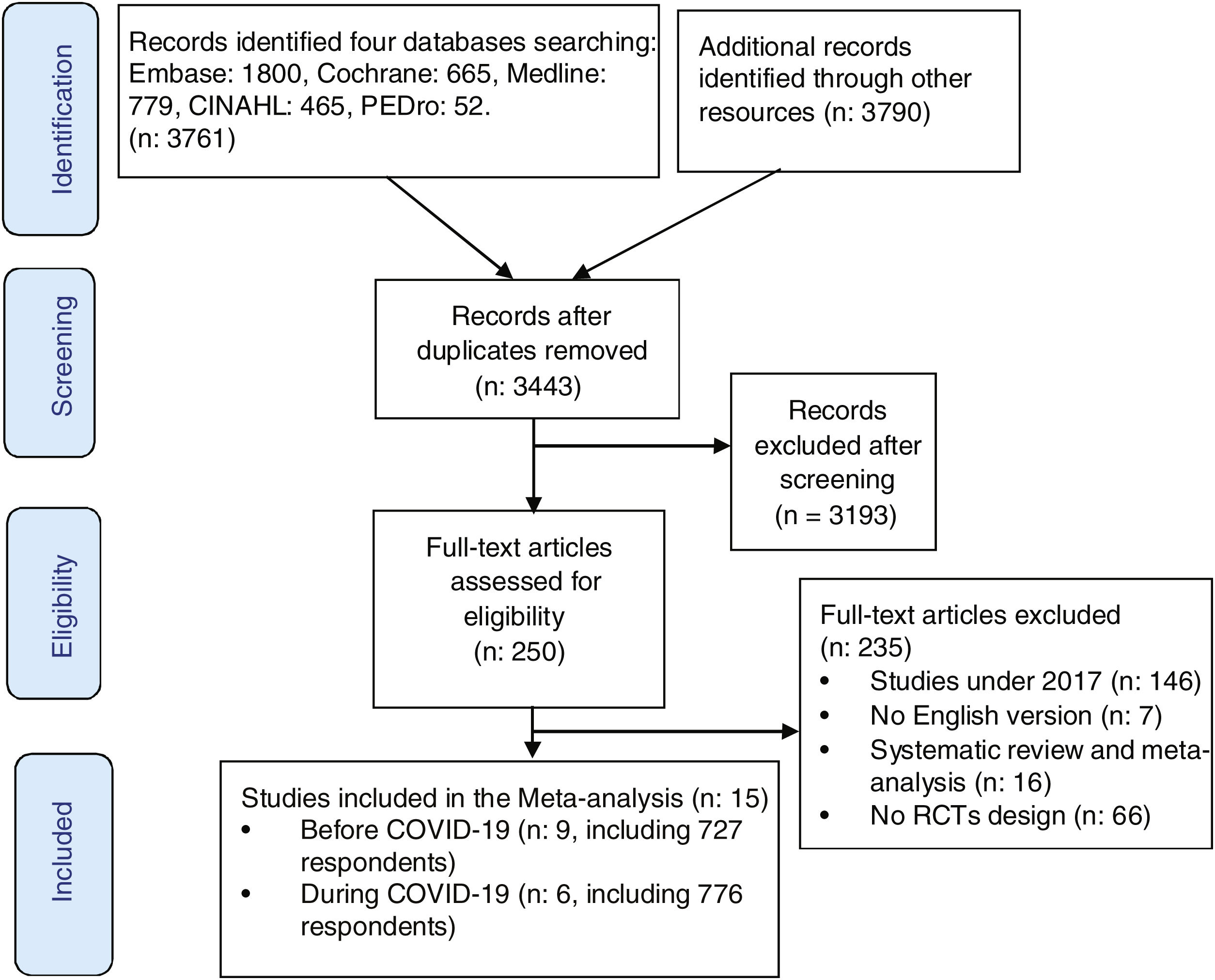
MethodsFollowing PRISMA guidelines, we searched for relevant articles from five databases, including Embase, MEDLINE, CINAHL, PEDro, Cochrane, and additional resources. Study quality was assessed using Joanna Briggs Institution (JBI). RevMan 5.3 software was used to perform the meta-analysis.
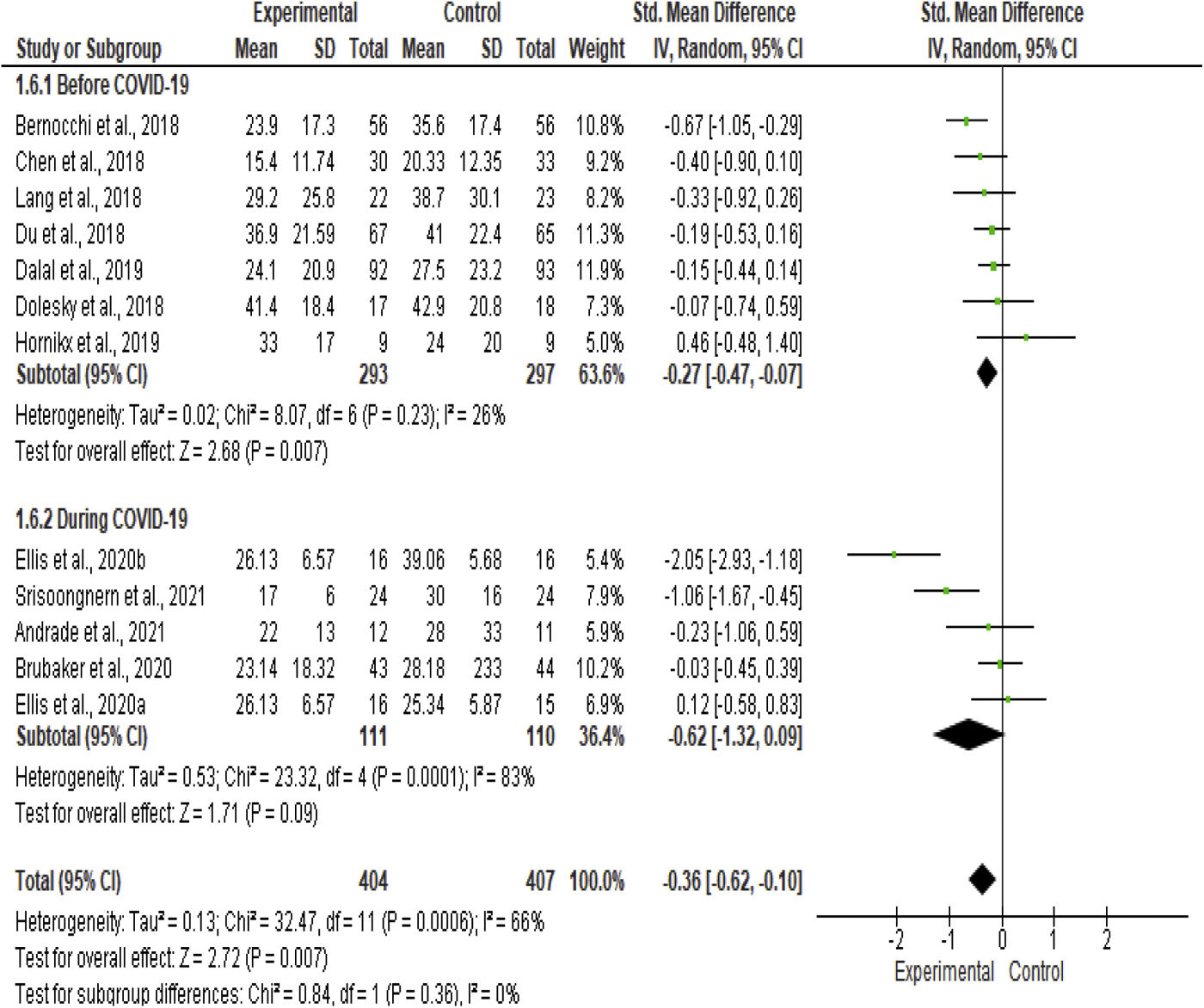
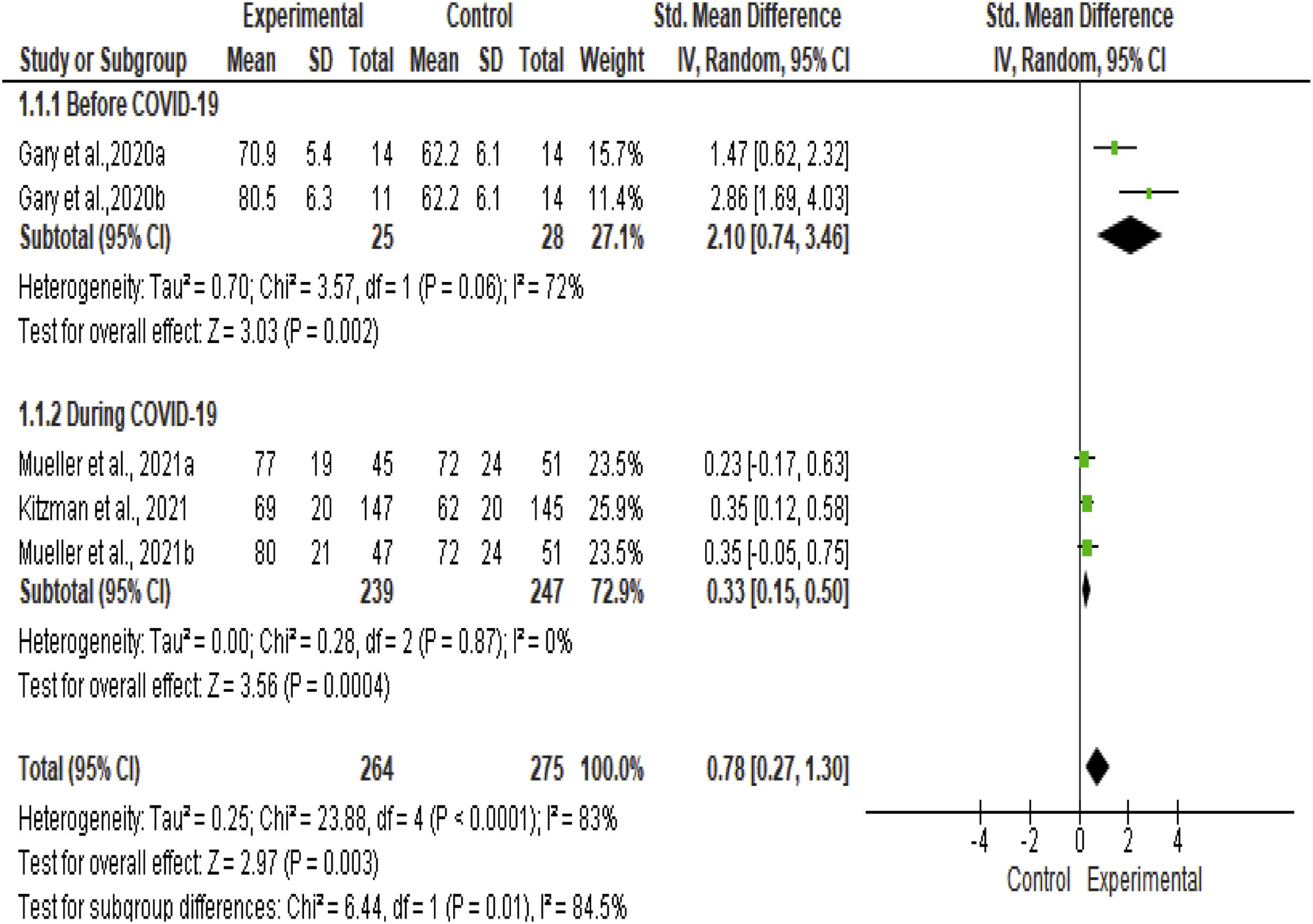
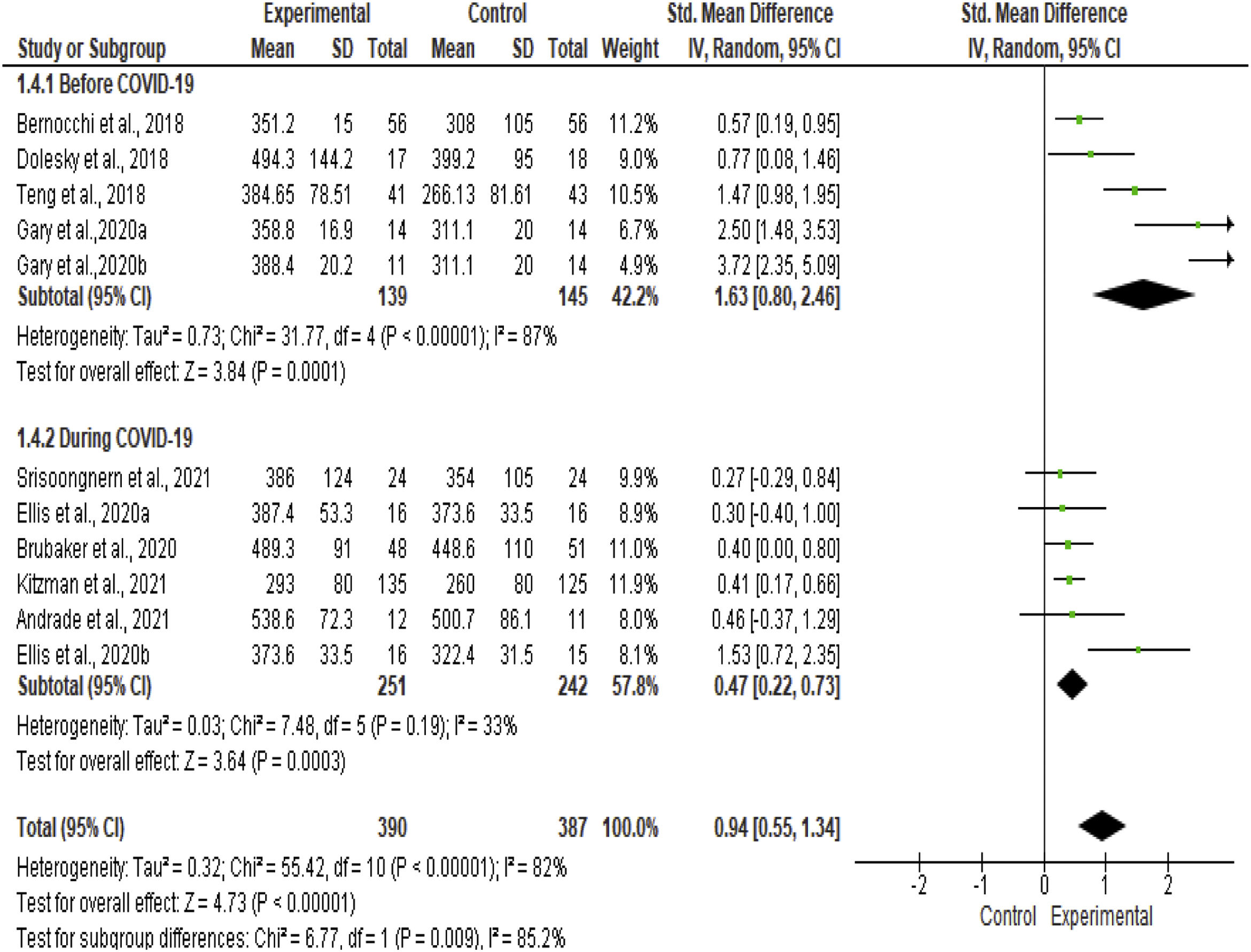
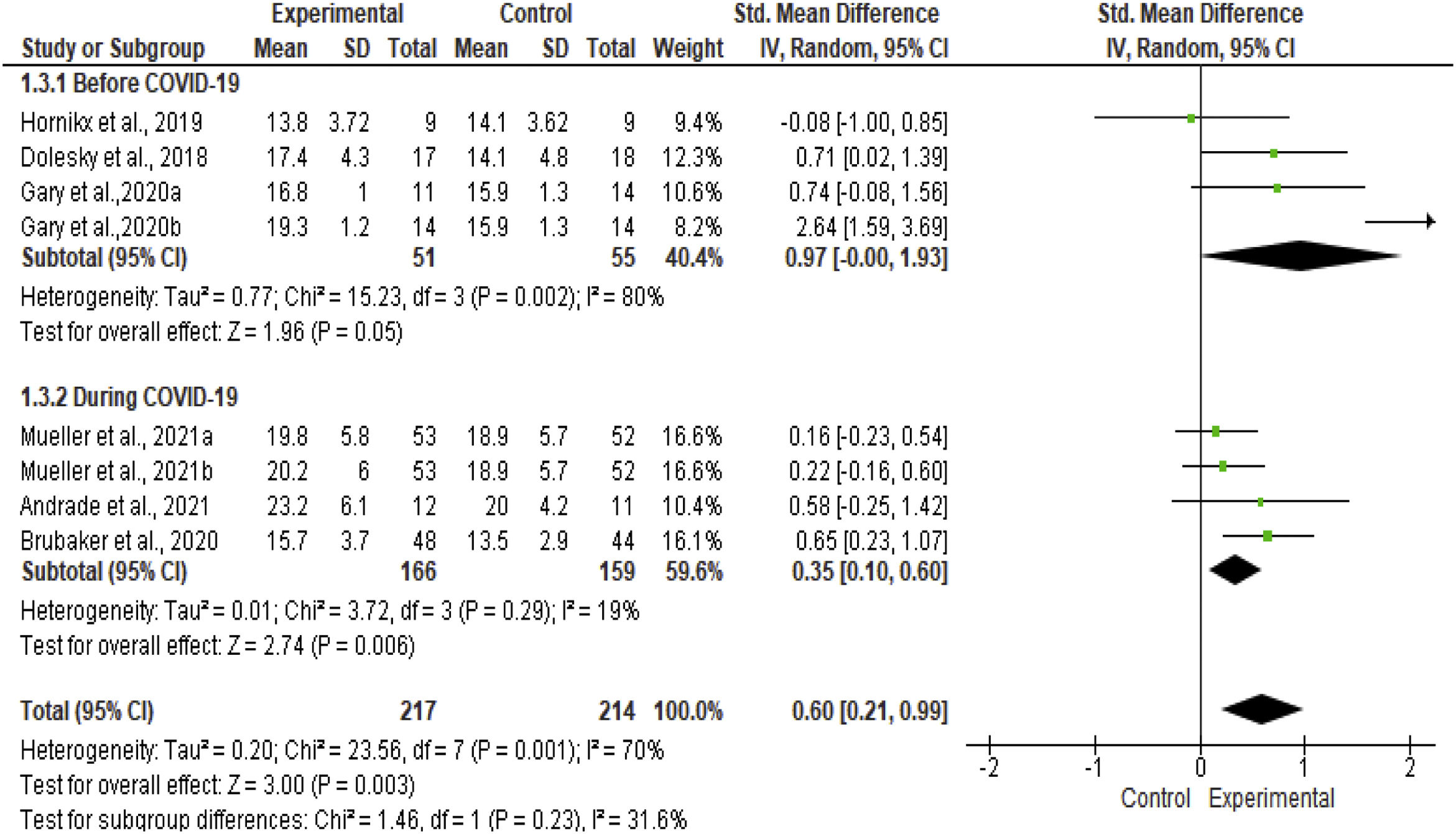
ResultFifteen randomized controlled trial studies met the criteria. Analysis of the subgroup before COVID-19 showed that PA had a significant effect on HRQOL, as measured by MLHFQ (SDM: −0.27, 95% CI: −0.47 to −0.07, n=590), KCCQ (SDM: 2.10, 95% CI: 0.74 to 3.46, n=53), 6MWT (SMD: 1.63, 95% CI: 0.80 to 2.46, n=284), and VO2 peak (SMD: 0.97, 95% CI: 0.00 to 1.93, n=106). Analysis of the subgroup during COVID-19 showed that PA resulted in a significant effect on HRQOL, MLHFQ (SDM: −0.62, 95% CI: −1.32 to 0.09, n=221), KCCQ (SDM: 0.33, 95% CI: 0.15 to 0.50, n=486), 6MWT (SMD: 0.47, 95% CI: 0.22 to 0.73, n=493), and VO2 peak (SMD: 0.35, 95% CI: 0.10 to 0.60, n=325).
ConclusionThe PA could increase HRQOL, 6MWT, and VO2 peak before and during COVID-19, and therefore should be considered as part of daily activities for patients with HF.
Comparar los efectos de la actividad física en la mejora de la calidad de vida relacionada con la salud (CVRS), el 6MWT y el pico de VO2 antes y durante la COVID-19 en pacientes con insuficiencia cardíaca.
MétodosSiguiendo las pautas PRISMA, buscamos artículos relevantes en 5 bases de datos, incluidas Embase, MEDLINE, CINAHL, PEDro y Cochrane, así como recursos adicionales. Para evaluar la calidad del estudio se utilizó el Instituto Joanna Briggs, y el software RevMan 5.3 para realizar el metanálisis.
ResultadoQuince artículos de ensayos controlados aleatorizados cumplieron con los criterios. El análisis del subgrupo antes de la COVID-19 mostró que la actividad física tuvo un efecto significativo en la CVRS, según lo medido por el MLHFQ (DE: −0,27, IC 95%: −0,47 a −0,07, n=590), el KCCQ (DE: 2,10, IC 95%: 0,74 a 3,46, n=53), el 6MWT (DE: 1,63, IC 95%: 0,80 a 2,46, n=284) y el pico de VO2 (DE: 0,97, IC 95%: 0,00 a 1,93, n=106). El análisis del subgrupo durante la COVID-19 mostró que la actividad física tuvo un efecto significativo en la CVRS, el MLHFQ (DE: −0,66, IC 95%: −1,32 a 0,09, n=221), el KCCQ (DE: 0,33, IC 95%: 0,15 a 0,50, n=486), el 6MWT (DE: 0,47, IC 95%: 0,22 a 0,73, n=493) y el pico de VO2 (DE: 0,35, IC 95%: 0,10 a 0,60, n=325).
ConclusiónLa actividad física podría aumentar la CVRS, el 6MWT y el pico de VO2 antes y durante la COVID-19, por lo que debe ser considerada como parte de las actividades diarias de los pacientes con insuficiencia cardíaca.
Heart failure (HF) is a serious health issue worldwide as its prevalence has increased over the past decade.1 The symptoms of HF, such as shortness of breath or dyspnea, fatigue, and edema, can affect the health-related quality of life (HRQOL), physical performance and exercise capacity of patients.2 Cardiac rehabilitation is fundamental to helping patients return to their normal life.
Engagement in physical activity (PA) is one recommendation for rehabilitating patients with HF.3 Furthermore, a routine PA could increase the oxidative metabolism of tissues and benefit the cardiac function in patients with HF.4 However, the emergence of the Coronavirus disease (COVID-19) pandemic has led a large number of governments to impose a nationwide quarantine to contain the spread of the virus,5 which ultimately forces people to do activities in a limited space. As a result, patients may decrease adherence to the routine PA. In Yamada study, community-dwelling older adults exhibited a decline in the frequency of PA and steps/day during COVID-19.6 Researchers have argued that the changes in lifestyle behaviors and engagement in PA during COVID-19 may trigger HF exacerbations. Hence, the potential adverse effect of low PA must be weighed carefully against the possible long-term negative health consequences i.e., cardiovascular risk burden.7
American Heart Association (AHA) guidance recommended routine PA for patients with HF, especially, those who had stable conditions.1,7 On the other hand, several studies found that reduced PA during COVID-19 had a negative impact on the health of patients with HF.8–10 Therefore, it is an important issue to maintain PA for patients with HF. To our knowledge, during the COVID-19 pandemic (2019–2021), no systematic reviews and meta-analyses have been done to examine the effect of PA in patients with HF. Therefore, an evidence-based study is needed to support the benefit of PA on health-related quality of life (HRQOL), six minutes walking test (6MWT), and oxygen consumption (VO2) peak before or during COVID-19. The three indicators are an essential part of assessing the severity of the condition of patients with HF. Likewise, an effective activities prescription should include the element of physical activities including the type of PA, duration of PA, frequency of PA, and intensity of PA. The present study is aimed at comparing the effects of PA on HRQOL, 6MWT, and VO2 peak before or during COVID-19 in patients with HF. In regard to this goal, the first objective of the study was to examine the effect of PA on HRQOL, 6MWT, and VO2 peak; second objective was to analyze the elements of PA before COVID-19 or during COVID-19 compared with the control group for patients with HF. Following the first and second objectives, the study compared the effects of PA on HRQOL, 6MWT, and VO2 peak between the results of the two time-specific groups.
MethodData sources and systematic literature reviewThe Preferred Reporting Item for Systematic Reviews and Meta-Analyses (PRISMA) is the guide in this systematic review11; see Fig. 1. The PICO format: population (P): patient with HF; intervention (I): PA; comparison (C): usual care, low PA, moderate-intensity training (MIT), walking, and meditation; and outcomes (O): primary (HRQOL and 6MWT) and secondary (VO2 peak). Five databases, including Embase, MEDLINE, CINAHL, Central Cochrane library, and PEDro, were selected to find relevant articles. The following keywords and Emtree/MESH terms were used in search of the articles: heart failure, cardiac failure, cardiac incompetence, chronic heart failure, heart backward failure, myocardial failure (related to heart failure); physical activity, “activity and physical” (related to PA); quality of life, health-related quality of life, and HRQL (related to Health-Related Quality of Life); 6min walk test, 6-minute walking test; six-minute walk testing, and six-minute walking test (related to 6 minutes walking test). Moreover, this review employed additional criteria in selecting the articles. The articles selected for systematic review must include patients with HF, employ a randomized control trial design (RCT), be published after 2017, and written in English. The criteria for the control group include usual care and meditation, while the exclusion criteria included systematic review and meta-analysis.
Firstly, we read titles and abstracts to evaluate whether the study used the PA to improve HRQOL, 6MWT (primary outcome), and VO2 peak (secondary outcome) in patients with HF. After the screening process, articles that do not meet the inclusion criteria were excluded. The process ended after the two reviewers investigated the reference lists of the full-text articles and did not identify additional studies that meet the criteria for inclusion in this study. Secondly, we separated the studies based on subgroup analysis. The studies before COVID-19 were conducted under 2019, and the studies during COVID-19 were conducted in 2019 until 2022.
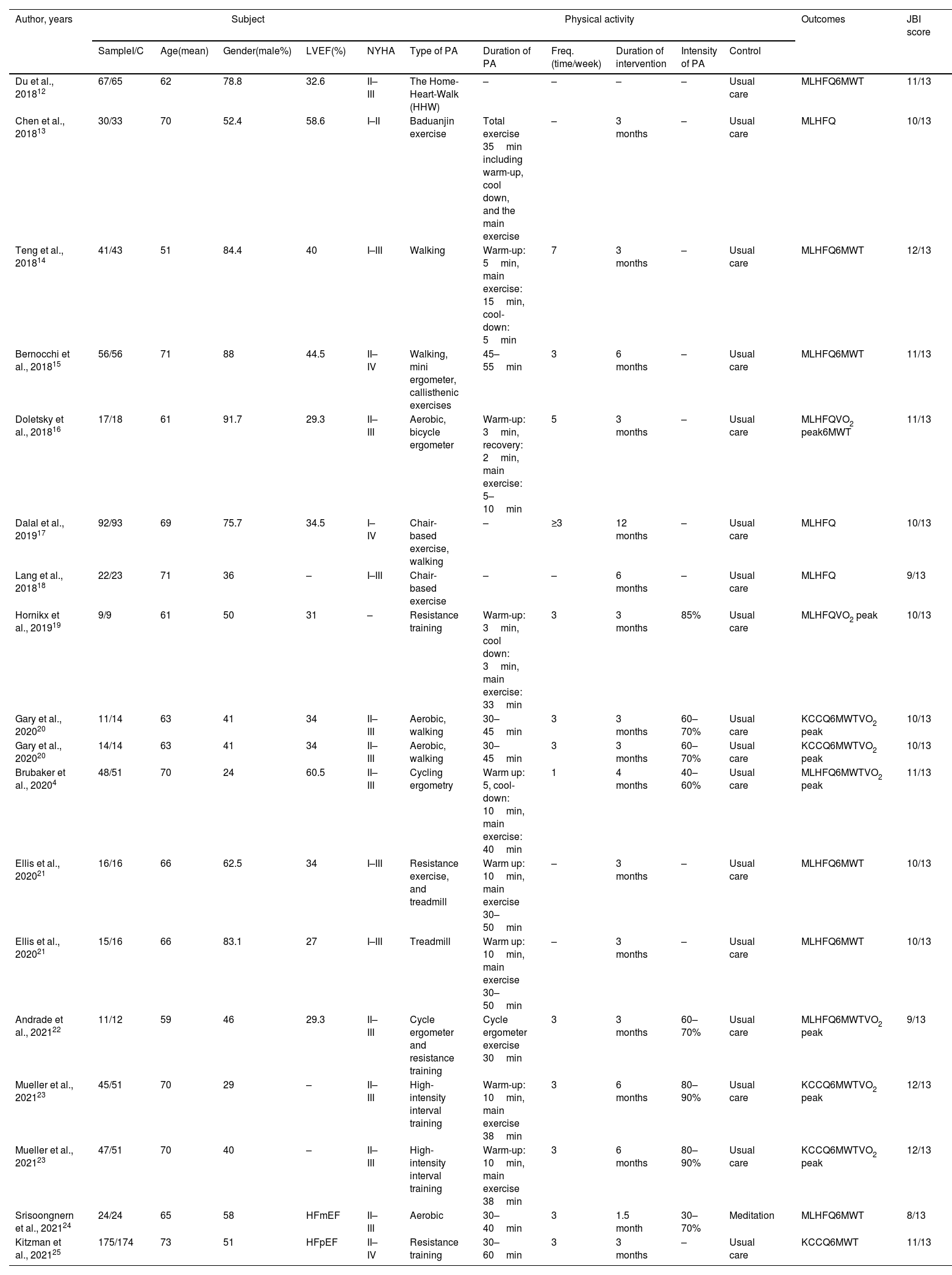
Data extraction and quality assessmentTwo reviewers performed data extraction independently, including the study's design, sample (intervention and control), age (mean), and the New York Heart Association (NYHA) functional classification. The PA components of these studies include the types of PA, duration of PA, frequency of PA (time/week), duration of intervention, the intensity of PA, and the control, while the measurement of the outcome included HRQOL (MLHFQ and KCCQ), 6MWT, and VO2 peak (Table 1). Additionally, the two reviewers independently assessed the methodological quality of the studies using the Joanna Briggs Institution (JBI) (Table 1). On the other hand, the authors designed and analyzed a funnel plot and used the Egger test to investigate possible publication biases for this outcome (Appendices 2–5).
Characteristics of studies.
| Author, years | Subject | Physical activity | Outcomes | JBI score | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| SampleI/C | Age(mean) | Gender(male%) | LVEF(%) | NYHA | Type of PA | Duration of PA | Freq. (time/week) | Duration of intervention | Intensity of PA | Control | |||
| Du et al., 201812 | 67/65 | 62 | 78.8 | 32.6 | II–III | The Home-Heart-Walk (HHW) | – | – | – | – | Usual care | MLHFQ6MWT | 11/13 |
| Chen et al., 201813 | 30/33 | 70 | 52.4 | 58.6 | I–II | Baduanjin exercise | Total exercise 35min including warm-up, cool down, and the main exercise | – | 3 months | – | Usual care | MLHFQ | 10/13 |
| Teng et al., 201814 | 41/43 | 51 | 84.4 | 40 | I–III | Walking | Warm-up: 5min, main exercise: 15min, cool-down: 5min | 7 | 3 months | – | Usual care | MLHFQ6MWT | 12/13 |
| Bernocchi et al., 201815 | 56/56 | 71 | 88 | 44.5 | II–IV | Walking, mini ergometer, callisthenic exercises | 45–55min | 3 | 6 months | – | Usual care | MLHFQ6MWT | 11/13 |
| Doletsky et al., 201816 | 17/18 | 61 | 91.7 | 29.3 | II–III | Aerobic, bicycle ergometer | Warm-up: 3min, recovery: 2min, main exercise: 5–10min | 5 | 3 months | – | Usual care | MLHFQVO2 peak6MWT | 11/13 |
| Dalal et al., 201917 | 92/93 | 69 | 75.7 | 34.5 | I–IV | Chair-based exercise, walking | – | ≥3 | 12 months | – | Usual care | MLHFQ | 10/13 |
| Lang et al., 201818 | 22/23 | 71 | 36 | – | I–III | Chair-based exercise | – | – | 6 months | – | Usual care | MLHFQ | 9/13 |
| Hornikx et al., 201919 | 9/9 | 61 | 50 | 31 | – | Resistance training | Warm-up: 3min, cool down: 3min, main exercise: 33min | 3 | 3 months | 85% | Usual care | MLHFQVO2 peak | 10/13 |
| Gary et al., 202020 | 11/14 | 63 | 41 | 34 | II–III | Aerobic, walking | 30–45min | 3 | 3 months | 60–70% | Usual care | KCCQ6MWTVO2 peak | 10/13 |
| Gary et al., 202020 | 14/14 | 63 | 41 | 34 | II–III | Aerobic, walking | 30–45min | 3 | 3 months | 60–70% | Usual care | KCCQ6MWTVO2 peak | 10/13 |
| Brubaker et al., 20204 | 48/51 | 70 | 24 | 60.5 | II–III | Cycling ergometry | Warm up: 5, cool-down: 10min, main exercise: 40min | 1 | 4 months | 40–60% | Usual care | MLHFQ6MWTVO2 peak | 11/13 |
| Ellis et al., 202021 | 16/16 | 66 | 62.5 | 34 | I–III | Resistance exercise, and treadmill | Warm up: 10min, main exercise 30–50min | – | 3 months | – | Usual care | MLHFQ6MWT | 10/13 |
| Ellis et al., 202021 | 15/16 | 66 | 83.1 | 27 | I–III | Treadmill | Warm up: 10min, main exercise 30–50min | – | 3 months | – | Usual care | MLHFQ6MWT | 10/13 |
| Andrade et al., 202122 | 11/12 | 59 | 46 | 29.3 | II–III | Cycle ergometer and resistance training | Cycle ergometer exercise 30min | 3 | 3 months | 60–70% | Usual care | MLHFQ6MWTVO2 peak | 9/13 |
| Mueller et al., 202123 | 45/51 | 70 | 29 | – | II–III | High-intensity interval training | Warm-up: 10min, main exercise 38min | 3 | 6 months | 80–90% | Usual care | KCCQ6MWTVO2 peak | 12/13 |
| Mueller et al., 202123 | 47/51 | 70 | 40 | – | II–III | High-intensity interval training | Warm-up: 10min, main exercise 38min | 3 | 6 months | 80–90% | Usual care | KCCQ6MWTVO2 peak | 12/13 |
| Srisoongnern et al., 202124 | 24/24 | 65 | 58 | HFmEF | II–III | Aerobic | 30–40min | 3 | 1.5 month | 30–70% | Meditation | MLHFQ6MWT | 8/13 |
| Kitzman et al., 202125 | 175/174 | 73 | 51 | HFpEF | II–IV | Resistance training | 30–60min | 3 | 3 months | – | Usual care | KCCQ6MWT | 11/13 |
Note: I/C: intervention/control; LVEF: left ventricle ejection fraction; HFpEF: heart failure preferred ejection fraction; HFmEF: heart failure middle range ejection fraction; HFrEF: heart failure reduced ejection fraction.
The RevMan 5.4 software was used to extract and pool data synthesis to investigate the effects of PA. The outcome measures were explained as changes from the baseline to the follow-up, and combined data were presented by the standardized mean difference (SMD). We set up the significance level as less than 0.05 with a corresponding confidence interval (CI) of 95%. Heterogeneity was quantified using the I2 test. An increase in HRQOL, 6MWT, or VO2 peak is presented as a positive effect size (ES). A random-effects model was used in this review.
ResultsDescription of selected studiesA total of 7551 articles were collected from five databases and additional sources (Embase: 1800 articles, Medline: 779 articles, Cochrane: 665 articles, PEDro: 52 articles, CINAHL: 465 articles), and additional resources (n: 3790). After removing 4108 duplicate articles, we further excluded 3193 records after screening titles and abstracts, leaving only 250 eligible articles. After the full-text screening, 235 articles were excluded for the following four reasons: studies were conducted before 2017 (n: 146), they were not written in English (n: 7), they were systematic reviews and meta-analyses (n: 16), and they did not use RCT design (n: 66) (see Fig. 1). Fifteen eligible articles were retrieved for the critical appraisal.4,12–25 The JBI score of articles were 8/13 to 12/13.
Participant characteristicsThe fifteen RCT studies were performed by men and women living with HF. The total number of respondents in this review was 1503, of which there were 740 respondents in the intervention group and 763 respondents in the control group. The mean age range of respondents was 51 to 71 years old, and they had NYHA classifications from I to IV. The mean of LVEF was 27–60.5%.
The effect of PA on HRQOL, 6MWT, and VO2 peak in patients with HFBefore COVID-19As shown in Table 2, seven studies involving 785 respondents in the subgroup analysis documented that the PA had a significant effect on improving HRQOL using Minnesota Living with Heart Failure Questionnaire (MLHFQ) (SDM: −0.27, 95% CI: −0.47 to −0.07, I2: 26%) than those in the control group (Table 2).12,13,15–19 Moreover, two studies involving 53 respondents showed that the PA significantly improved HRQOL using the Kansas City Cardiomyopathy Questionnaire (KCCQ) (SDM: 2.10, 95% CI: 0.74 to 3.46, I2: 72%) than those in the control group (Table 3).20 Furthermore, the PA group showed significant improvements in 6MWT (SMD: 1.63, 95% CI: 0.80 to 2.46, I2: 87%) than those in the control group in five studies with 284 respondents (Table 4).14–16,20 On the other hand, a total of four studies involving 106 respondents showed that PA significantly improved the VO2 peak (SMD: 0.97, 95% CI: 0.00 to 1.93, I2: 80%) than those in the control group (Table 5).16,19,20
During COVID-19In the subgroup analysis, including 221 respondents, PA was found to significantly improve HRQOL using MLHFQ (SDM: −0.66, 95% CI: −1.32 to 0.09, I2: 80%) than those in the control group (Table 2)4,21,22,24; moreover, results of three studies including 486 respondents showed that the PA had a significant effect of improving on HRQOL using the KCCQ (SDM: 0.33, 95% CI: 0.15 to 0.50, I2: 0%) than those in the control group (Table 3).23,25 Six studies with a total of 493 respondents showed that PA significantly improved 6MWT (SMD: 0.47, 95% CI: 0.22 to 0.73, I2: 33%) than those in the control group (Table 4),4,21,22,24,25 while four other studies with no less than 325 respondents showed PA had a significant effect on improving VO2 peak (SMD: 0.35, 95% CI: 0.10 to 0.60, I2: 19%) than those in the control group (Table 5).4,22,23
The elements of PABefore COVID-19Regarding the type of PA, six studies used walking, and several studies combined walking and strength/endurance exercise, ergometer exercise, chair-based exercise, and aerobic.12,14,15,17,20 Four studies used only aerobic, cycle ergometer exercise, Baduanjin exercise, and chair-based exercise.13,16,18,19 According to the duration of PA, including warm-up/cool-down and main exercise, six studies reported 20–60min13–16,19,20; however, three studies did not report it.12,17,18 Seven studies reported the frequency of PA of 3–7 times/week14–17,19,20; nevertheless, three studies did not report it.12,13,18 Regarding the duration of intervention, this review found that eight studies reported 3–12 months13–20; however, one study did not report it.12 Additionally, three studies reported that the intensity of PA was 60–85%,13,20 and seven studies did not report it.12–18
During COVID-19Six studies used cycling ergometry, treadmill, aerobic, resistance training, and resistance exercise,4,21,22,24,25 and two studies used high-intensity interval training on the type of PA.24,25 The total duration of PA was 30–60min, including warm-up, cool-down, and the main exercise. The frequency of PA was one to three times/week4,24,25; however, two studies did not report it.21 Eight studies reported 1.5 months to 6 months for the duration of the intervention.4,21,25
The methodological quality and risk of bias of the studyThe JBI was used to evaluate the methodological quality of studies. The results showed that the quality of the articles was moderate to high based on the complete reading of the articles and consensus between two reviewers (Table 1). On the other hand, most studies reported low risk in the random sequence generation, and allocation concealment was good (more than 90%). About 75% of studies presented a low risk in the blinding of participants and personnel. More than 50% of studies were found low risk in the selective reporting and incomplete outcome data; however, less than 50% of studies reported low risk in the blinding of outcome assessment (see Appendix 1). On the other hand, the current study had several publication biases, which the result funnel plot showed from heterogeneity that is due entirely to there being two distinct subgroups of studies, especially in the effect of PA on the HRQOL and 6MWT (Appendices 2–4).
DiscussionThis meta-analysis included 1503 patients with HF. This review found that more patients were doing PA before COVID-19 compared to the during COVID-19 pandemic because they were worried about contracting the virus. Several factors influencing PA during COVID-19 include reduced programs of cardiac rehabilitation and people refraining from going outside. However, the routine PA had benefits in increasing HRQOL, 6MWT, and VO2 peak conducted before or during COVID-19 than the control group. These results support the notion that improving the engagement of PA is one of the recommendations for cardiac rehabilitation for patients with HF.3 PA can increase patients’ physical function and exercise capacity,22,23 which consequently increases their HRQOL.4 Moreover, several studies argued that routine PA had the benefit to increase the cardiorespiratory and metabolic systems of the body.2–4
The element of PABoth groups had different types of PA. Before COVID-19 the PA used were walking, strength/endurance exercise, ergometer exercise, chair-based exercise, Baduanjin exercise, aerobic, and chair based-exercise,13–20 whereas during COVID-19 it comprised of cycling ergometry, treadmill, aerobic, resistance training, and resistance exercise, and walking.4,21–25 Nonetheless, the results of both groups showed a similar effect on increasing HRQOL, 6MWT, and VO2 peak in patients with HF. Most PA before COVID-19 can be done outside, which was difficult to be done during COVID-19. Nevertheless, PA done in both periods had a similar effect on increasing HRQOL, 6MWT, and VO2 peak. Routine PA has the benefit to increase the physical fitness of people living with HF by increasing the power of autonomic function, and endothelial function.26,27 In addition, several studies suggested that regular PA can improve HRQOL and reduce hospitalization of those not having active PA.3,28
The current study found that the frequency of PA before COVID-19 was 3–7 times/week, and this frequency decreased during COVID-19 (1–3 times/week). Yamada's study reported that the total PA time per week significantly decreased by 26.5% during the pandemic. Moreover, the total PA time per week decreased by 65min in older adults.6 Even though Kato's study suggested that the resumption of routine and the increase of PA might improve their functional capacity during COVID-19.9
On the other hand, this study found that the intensities of PA were slightly different before and during COVID-19. The group before COVID-19 had moderate intensity (60–85%) while the other group had a high intensity of PA. Yet, the intensity of PA in both groups showed that similar effect on improving HRQOL, 6MWT, and VO2 peak for patients. Ultimately, it is therefore suggested that the moderate and high intensity had a similar effect to increase oxidative metabolism for physical fitness patients with HF.
Relevance in clinical practicePA is essential for cardiac rehabilitation in patients with HF, moreover, low PA was a potential effect that must be weighed carefully against the possible long-term negative effects on health.4,26 Furthermore, regular PA increased the HRQOL, 6MWT, and oxygen consumption for patients with HF.4,12–25 Nevertheless, this systematic review and meta-analysis had several limitations. Firstly, only articles written in English were included in this review. Secondly, this review showed minimal publication bias. We found that some articles not reporting blinding of outcome assessment, incomplete outcome data, and selective reporting. However, the existence of two independent authors, a comprehensive search in five databases, and specific methods for the analyses were carried out to minimize the review biases. Thirdly, the forest plot and funnel plot showed high heterogeneity in the results of the various studies, showing that factors other than those observed in stratified analyses might be a contribution. We assumed that some studies had a small sample size. Furthermore, some part related to the heterogeneity is likely the subject variety of the observed populations (variable age, gender, LVEF, and NYHA classification), as well as the incompatibility in the levels of PA, type of PA, and duration of PA. Fourthly, several studies in the during COVID-19 sub-group did not include the date of the study. Therefore, we assume that the studies that had been reviewed were conducted on the year of the COVID-19 epidemic occurrence. Hence, further exploration, through future research, is needed to determine whether our findings can be replicated or confirmed.
ConclusionThis review found that PA is beneficial for patients with HF. Before or during COVID-19 groups included moderate and high-intensity of PA, and both groups were similar in the duration of PA. Nevertheless, before COVID-19 had a longer time frequency of PA compared with during COVID-19. Likewise, there were differences in the type of PA in both groups, however, having demonstrated the available RCTs, our review suggested that before or during COVID-19, any type of PA had a similar effect on increasing HRQOL, 6MWT, and VO2 peak. Thus, PA should be considered a promising cardiac rehabilitation; doing PA regularly can improve the health status of patients with HF. These findings can guide future research by providing data and information about PA.
Conflict of interestNo conflicts of interest.