To evaluate the prevalence of and factors associated with SARS-CoV-2 infection in general practitioners and nurses from primary care centers and nursing homes in the Healthcare Area of León (Spain).
Materials and methodsCross-sectional study in a convenience sample of professionals from 30 health centers and 30 nursing homes from the primary care management division of the Healthcare Area of Leon. The work center, type of profession, COVID-19 infection, level of exposure, compliance with preventive measures, isolation (if required) and diagnostic tests carried out were collected. The determination of infection was made by differentiated rapid diagnostic test (dRDT), using a finger-stick whole-blood sample. The association of variables with infection was assessed by multivariable non-conditional logistic regression. The true prevalence of SARS-CoV-2 infection was calculated according to two scenarios for RDT (Sensitivity=0.6 and Specificity=0.985; Sensitivity=0.8 and Specificity=1).
ResultsThe true prevalence of SARS-CoV-2 infection was between 4.9% and 11.0%. The observed prevalence was 5.9% and was higher in nursing homes than in primary care centers (9.5% vs. 5.5%). No statistically significant differences were observed by sex, type of professional, level of exposure or compliance with preventive measures.
ConclusionsThe prevalence of SARS-CoV-2 infection in this group is low. A high number of professionals remain susceptible to SARS-CoV-2 infection and therefore protective measures should be taken, especially for professionals working in nursing homes.
Evaluar la prevalencia y los factores asociados a la infección por SARS-CoV-2 en médicos y enfermeras de centros de atención primaria y residencias de ancianos del área de salud de León (España).
Material y métodosEstudio observacional realizado en una muestra de conveniencia de profesionales de 30centros de salud y 30 residencias de ancianos, de la Gerencia de Atención Primaria del área de salud de León. Se recogió información del centro de trabajo, tipo de profesión, infección por COVID-19, nivel de exposición, cumplimiento de medidas preventivas, aislamiento (si fue requerido) y test diagnósticos realizados. La determinación de infección fue llevada a cabo mediante prueba de diagnóstico rápido diferenciado (PDRd), usando muestra de sangre capilar. La asociación de las variables con la infección se evaluó mediante regresión logística multivariable no condicional. La prevalencia real de infección por SARS-CoV-2 fue calculada de acuerdo a dos escenarios para el PDRd (sensibilidad=0,6 y especificidad=0,985; sensibilidad=0,8 y especificidad=1).
ResultadosLa prevalencia real de infección por SARS-CoV-2 se encontró entre el 4,9 y el 11,0%. La prevalencia observada fue del 5,9%, siendo mayor en trabajadores de residencias de ancianos que de centros de salud de atención primaria (9,5% vs 5,5%). No hubo diferencias estadísticamente significativas por sexo, tipo de profesional, nivel de exposición o cumplimiento de medidas preventivas.
ConclusionesLa prevalencia de la infección por SARS-CoV-2 en este grupo es baja. Un gran número de profesionales siguen siendo susceptibles a la infección por SARS-CoV-2 y, por lo tanto, deben adoptarse medidas de protección, especialmente en los profesionales de las residencias de ancianos.
The novel disease known as COVID-19 was detected for the first time in December 2019 in Wuhan, China.1 This is a disease caused by a virus from the Coronaviridae family, SARS-CoV-2 (Severe Acute Respiratory Syndrome-Coronavirus-2),2,3 which affects the eldery most severely.4
Healthcare workers, due to their work in the diagnosis, treatment and care of patients with COVID-19, are particularly exposed to sources of SARS-CoV-2 infection. In the pandemic earlier stages, ignorance of the real significance of the problem, the lack of personal protective equipment or its misuse could lead to significant exposure of healthcare workers to SARS-CoV-2. Altogether, these facts would explain to a large extent that of the total of 250,287 cases of COVID-19 reported in Spain (on May 21, 2020) to the Spanish Network for Epidemiological Surveillance (RENAVE), 16.3% corresponded to healthcare workers.5 The Spanish primary care has been especially affected by all these problems and has been the first barrier against COVID-19.6
The aim of this study is to evaluate the prevalence of and factors associated with the SARS-CoV-2 infection in general practitioners and nurses of primary care centers and nursing homes in the Healthcare Area of León.
MethodologyDesignObservational, descriptive, cross-sectional study.
PopulationGeneral practitioners (GP) and primary care nurses in the Healthcare Area of León, who worked in health centers or nursing homes. The convenience sample obtained in this study was comprised of professionals from 30 health centers and 30 nursing homes who wanted to participate in the study.
Information collectedBy means of a registration sheet, socio-demographic information was collected, as well as information on the work center, type of profession, previous diagnosis or suspicion of COVID-19, level of exposure, compliance with preventive measures, isolation (if required) and diagnostic tests carried out.
The level of exposure to coronavirus and the degree of compliance with preventive measures were recorded using a Likert scale of 0–10, with 0 being the lowest degree of exposure or compliance and 10 the highest.
Diagnosis of COVID-19 infectionInfection status determination: Using a fingerstick whole blood sample, the COVID-19 infection was evaluated with a differentiated rapid diagnostic test (RDT), which classifies IgG and IgM separately (All Test® 2019-nCoV IgG/IgM Rapid Test Casette of Hangzhou All Test Biotech Co Ltd). The result was read 10–15min after the test was carried out.7
TemporalizationThe determination was made during the first two weeks of April 2020.
Ethical aspectsWork center protocols on processing patient information have been followed and the processing of information has been made anonymous.
Statistical analysisWe calculated central and dispersion measures of quantitative variables (mean and standard deviation (SD)) and frequencies with their 95% confidence intervals in qualitative variables. The dependent variable, COVID-19 infection, was considered when the IgG or IgM were positive. The relationship with the collected variables was evaluated by unconditional logistic regression adjusted for all factors analyzed, and the odds ratio (OR) and its 95% confidence intervals were calculated. All analyses were performed with the Stata 14 statistical package.8
Also, the true prevalence was calculated according to two internal validity scenarios for RDP, one with a sensitivity of 60% and specificity of 98.5% and the other with a sensitivity of 80% and specificity of 100%, as described by Rogan and Gladen9 using the application EPITOOLS available on the Internet.10
ResultsApproximately 1000 nurses and doctors were the target population, 676 of whom participated in the study, i.e. two thirds. The average age of the participants was 47.7±12.4 years and 74% were females. Half of the sample were nurses and 88% of the workers were from primary care centers. In relation to exposure and compliance with preventive measures, 44% of the respondents reported high exposure to COVID-19 and 31% high compliance with preventive measures (10 points on the survey).
Out of the 615 participants who answered the question, 5 (0.8%) had been diagnosed with COVID-19 and out of 628, 44 (7.0%) had been isolated due to contact with sick or suspected COVID-19 patients.
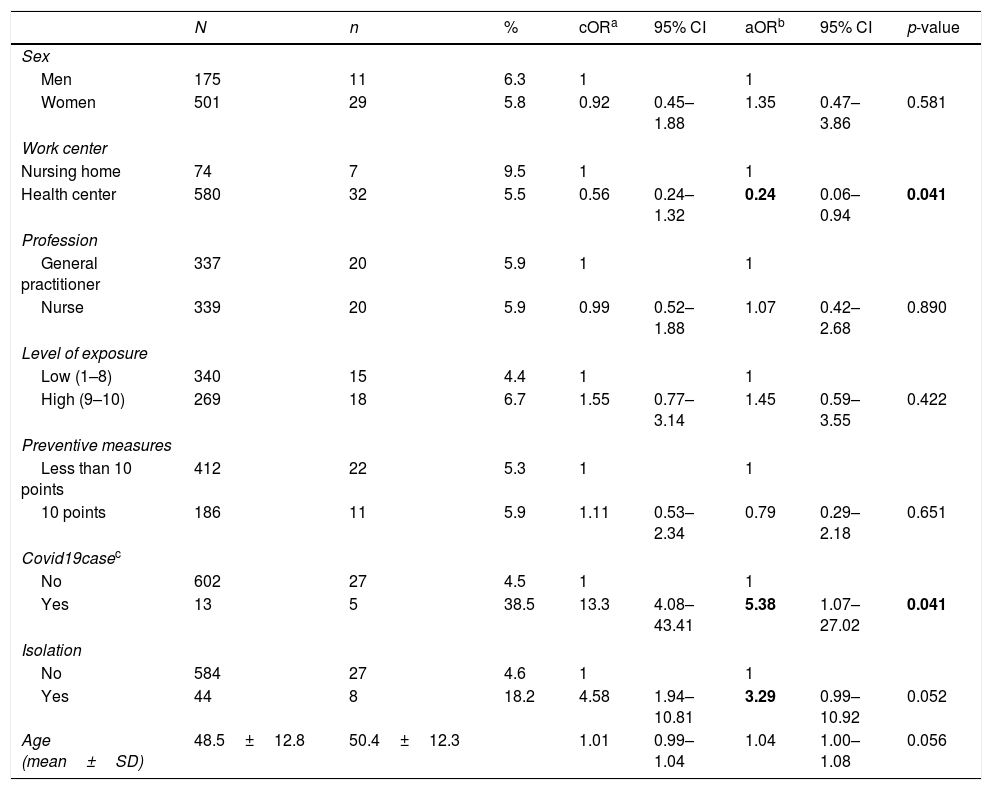
The overall prevalence of positive RDT was 5.9% (40/676), with no statistically significant differences observed by sex, type of professional, level of exposure or compliance with preventive measures. However, the higher prevalence of positive RDTs in nursing home workers compared to those working in health centers is noteworthy (Table 1). On the other hand, 38.5% of the cases of COVID-19 and 18.2% of the people who required isolation had positive in RDTs (Table 1).
Factors associated with SARS-CoV-2 infection in the health professionals studied.
| N | n | % | cORa | 95% CI | aORb | 95% CI | p-value | |
|---|---|---|---|---|---|---|---|---|
| Sex | ||||||||
| Men | 175 | 11 | 6.3 | 1 | 1 | |||
| Women | 501 | 29 | 5.8 | 0.92 | 0.45–1.88 | 1.35 | 0.47–3.86 | 0.581 |
| Work center | ||||||||
| Nursing home | 74 | 7 | 9.5 | 1 | 1 | |||
| Health center | 580 | 32 | 5.5 | 0.56 | 0.24–1.32 | 0.24 | 0.06–0.94 | 0.041 |
| Profession | ||||||||
| General practitioner | 337 | 20 | 5.9 | 1 | 1 | |||
| Nurse | 339 | 20 | 5.9 | 0.99 | 0.52–1.88 | 1.07 | 0.42–2.68 | 0.890 |
| Level of exposure | ||||||||
| Low (1–8) | 340 | 15 | 4.4 | 1 | 1 | |||
| High (9–10) | 269 | 18 | 6.7 | 1.55 | 0.77–3.14 | 1.45 | 0.59–3.55 | 0.422 |
| Preventive measures | ||||||||
| Less than 10 points | 412 | 22 | 5.3 | 1 | 1 | |||
| 10 points | 186 | 11 | 5.9 | 1.11 | 0.53–2.34 | 0.79 | 0.29–2.18 | 0.651 |
| Covid19casec | ||||||||
| No | 602 | 27 | 4.5 | 1 | 1 | |||
| Yes | 13 | 5 | 38.5 | 13.3 | 4.08–43.41 | 5.38 | 1.07–27.02 | 0.041 |
| Isolation | ||||||||
| No | 584 | 27 | 4.6 | 1 | 1 | |||
| Yes | 44 | 8 | 18.2 | 4.58 | 1.94–10.81 | 3.29 | 0.99–10.92 | 0.052 |
| Age (mean±SD) | 48.5±12.8 | 50.4±12.3 | 1.01 | 0.99–1.04 | 1.04 | 1.00–1.08 | 0.056 | |
According to these results, working in a health center is a protective factor, versus working in a nursing home (aOR=0.24) and those previously diagnosed with COVID-19 or who were isolated due to contact with a confirmed or suspected case, presented a higher risk of being RDT positive: aOR=5.38 and aOR=3.29 respectively.
The true prevalence, under the scenario of RDT sensitivity and specificity of 0.6 and 0.985, respectively, is 7.6% (95% CI=4.9%–11.0%), while in the scenario with a sensitivity of 0.8 and a specificity of 1 it is 7.4% (95% CI=5.5%–10.0%).
DiscussionThe true prevalence of SARS-CoV-2 infection in the sample studied is between 4.9% and 11.0% in the scenarios described. The most relevant results of this study indicate that the observed prevalence of SARS-CoV-2 infection in the health workers analyzed is 5.9% (95% CI 4.4%–8.0%), and was higher in nursing home workers than in primary care centers (9.5% vs. 5.5%).
The prevalence of infection found in our results is in line with the 5% reported in a preliminary report of the seroprevalence results in the Spanish general population of the ENE-COVID study. The results obtained in this study for León, indicate a prevalence of 7.0% (95% CI 4.8%–10.0%), slightly higher in women than in men (7.8% vs. 6.2% respectively), which differs from our results (5.8% women vs. 6.3% men). Despite this, the participation rate of ENE-COVID referring to seroprevalence data with RDTs was two thirds, which was the same in our study. If we observe the confidence intervals obtained, there is overlap, meaning there would be no significant differences between the studies.11
Our result is also lower than the 11.2% found in another recent seroprevalence study carried out in health professionals at the Hospital Clinic of Barcelona.12 These differences may be due to the sample studied, given that our study focused on primary care workers and not on hospital workers, and only on doctors and nurses without including other professionals.
The observed prevalence in our study is surprisingly low, for what was originally expected, and can be explained with several reasons: (1) the non-participation of those workers on leave due to COVID-19 (the estimated staff of doctors and nurses at the centers studied is about 500 doctors and 500 nurses which means that two thirds of the possible staff have participated in the study); (2) the implementation of preventive measures, social isolation and confinement had already been initiated before the sample was obtained; and (3) the care measures implemented in Primary Care. It is worrying the there is a high number of respondents who are susceptible to infection in future waves.
The World Health Organization (WHO) has identified several factors associated with SARS-CoV-2 infection in health professionals, including: late recognition or suspicion of patients with COVID-19, working in a high-risk area, longer hours on duty, lack or low use of personal protective equipment (PPE), and inadequate hand hygiene.13
In our results, 44% of the respondents indicated that they had had a high exposure to COVID-19. However, there was no statistically significant association between the level of self-perceived exposure and the prevalence of SARS-CoV-2 infection in our sample (aOR=1.45, 95% CI=0.59–3.55). This could be explained by a possible selection bias, given that there is a third of non-participants in the study who could be on sick leave as a result of the COVID-19.
According to the preventive measures, it is important to note that 31% of those surveyed in our study reported a high level of compliance to these measures and did not find significant association with the prevalence of SARS-CoV-2 infection (aOR=0.79, 95% CI=0.29–2.18). However, this result highlights the high percentage of health care workers that may be vulnerable to infection due to incorrect use or non-compliance. This can be explained with several reasons: (1) the selection bias cited above, (2) the functioning of the containment measures that were active during this study, which decreased the number of circulating sources of infection, (3) the measures that primary care adopted, such as telephone consultation assistance. Despite this, it would be desirable to increase (to 100% if possible) the adequate compliance with preventive measures to reduce the risk professionals, as well as their extension to patients or relatives.
In relation to the workplace, our study shows a higher infection rate among workers in nursing homes (9.5%) compared to those working in health centers (5.5%). This difference can be explained by the conditions of the nursing homes themselves and the particular incidence that the COVID19 has had on them.14
Finally, our results reflect a higher risk of positive RDT in those respondents with a previous diagnosis of COVID-19 (aOR=5.38) or those who were isolated after contact with a confirmed or suspected case (aOR=3.29). These results could be due to a combination of effects: (1) the sensitivity of the tests (between 20 and 40% of false negatives),15 and (2) the inclusion of suspects with non-specific clinical manifestations that may not be COVID-19. As such, this study analyzed the true prevalence in different sensitivity and specificity scenarios of RDT, obtaining a range of 4.9–11%. Although these data are nearly double the observed prevalence, they still highlight the high percentage of health professionals who will be vulnerable to infection in the next waves, and whose protection should therefore be increased.
However, our results need to be analyzed with caution, as there are certain limitations. (1) The descriptive nature of the study and the low rate of infection may influence the statistical power of the findings. (2) The study was conducted at the same time that the confinement and preventive measures were put in place, so the infection may be underestimated. (3) The RDTs have obtained different certifications for their clinical use but they also have sensitivity problems. Despite these limitations, this study highlights the prevalence in primary care and nursing home doctors and nurses, as well as the associated factors, generating evidence that is vital in the fight against COVID-19.
ConclusionThe prevalence of SARS-CoV-2 infection in tested health workers is low, which is similar to other national studies. Our results indicate that a high number of professionals remain susceptible to SARS-CoV-2 infection, meaning protective measures should be taken, both in primary care, as the main contact with the healthcare system, and in nursing homes.
FundingThis research has not received specific support from public sector agencies, the commercial sector or non-profit organizations.
Conflict of interestThe authors declare no conflict of interest.
The authors would like to thank all the workers for their participation in this study. And of course, thanks to the Primary Care Management Division of the Healthcare Area of Leon and the University of Leon, because of their collaboration has been crucial in developing this study.