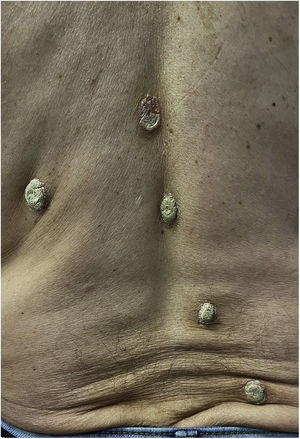
A 58-year-old male without any relevant personal nor family history presented to our department with several scaly, hyperkeratotic, adherent, plaques sharply demarcated on his back, with no other accompanying signs or symptoms (Fig. 1). The lesions appeared two years before, and had progressively increased in size and number acquiring the typical cone-like scale in a limpet shell appearance. The differential diagnosis included other types of psoriasis, like ostraceous psoriasis (defined by a characteristic concave surface), secondary syphilis, drug-reactions, disseminated histoplasmosis and Norwegian scabies. The patient was repeatedly tested negative for syphilis antibodies, and refused a biopsy. Given the lack of epidemiological background or other clinical findings supporting the aforementioned diseases, rupioid psoriasis was thus considered the definite diagnosis. He was started on acitretin 25mg a day orally and a topical combination of betamethasone and salicylic acid in ointment. After three months of treatment the lesions had greatly improved, and acitretin was stopped due to side effects. The patient continued using topical corticosteroids and vitamin D derivatives until resolution. It is of the utmost importance to interrogate about the intake of certain medications during the anamnesis, such as hydroxychloroquine, β-blockers and lithium, and rule out conditions like HIV and syphilis.1,2
Written informed consent was obtained from the patient for publication of his case details.
FundingThis article has no funding source.
Conflict of interestThe authors have no conflict of interest to declare.