To determine the association between flexibility of the ischiotibial muscles, function and pain in patients with knee osteoarthritis (OA).
MethodsA total of 33 patients of both genders with an age greater than or equal to 40 years, clinically diagnosed with osteoarthritis in one or both knees with radiographic evidence of the disease, were recruited and evaluated. Participants underwent the WOMAC questionnaire, along with measurements of flexibility using a Lafayette flexometer and the Back Saver Sit and Reach test. The correlation between the WOMAC questionnaire and its three components (pain, stiffness and functional limitation) was recorded. Total flexibility was obtained from the mean measurement of both knees.
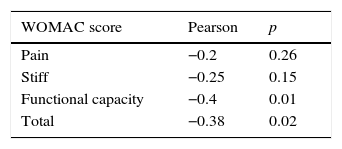
ResultsA statistically significant correlation between the global WOMAC score and flexibility was found (−0.38, p=0.02). When the components were analyzed separately, a statistically significant correlation between total flexibility and functional limitation (−0.40, p=0.01) was evident; however, this was not so with the components of pain and stiffness.
ConclusionsGreater ischiotibial flexibility reduces pain, stiffness, and significant functional limitation in patients with knee OA. These results show that it is important to prescribe flexibility exercises during physical therapy in these patients.
Osteoarthritis (OA) affects 60% of men and 70% of women over the age of 70. The prevalence of OA has been increasing, and it is now one of the 10 leading causes of total disability in Mexico.1,2 The most affected joints are the knee and hip.3
The prevalence of knee OA has been estimated to affect from 4 to 30% in adults depending on gender, age, and physical activity.4,5 About 85% of the population over the age of 60 has radiographic evidence of OA.6 This high predilection for the knee is mainly due to joint loading, which makes it susceptible to wear and tear under pressure.7
The clinical manifestations of the disease include pain, decreased range of motion, quadriceps muscle weakness, and impaired proprioception.8 Multiple studies report a condition beyond the cartilage that affects muscles, tendons, ligaments, synovial capsule, and bone.9
Knee OA pain affects approximately 10–30% of adults, and of these, 25% are severely disabled owing to difficulty in performing the activities of daily living due to muscle spasms or weakness.10–13
There is a clear association between decreased range of motion – secondary to decreased flexibility, weakness, and muscle spasms – and disability.13
Exercise and physical therapy have an important role in the treatment of knee OA, with the main objectives being to reduce pain and inflammation, increase muscle strength, and finally, maintain or improve range of motion.14,15
Enhancement of range of motion, especially knee extension, has been associated with improvement in pain and muscle function.16,17 Despite this, it is not always considered a priority to work on flexibility.
Onigbinde (2013) found a difference by comparing measures of flexibility between subjects with knee osteoarthritis and same-age subjects chosen as controls, concluding that ischiotibial flexibility was significantly lower in the affected subjects. It is unknown whether this decrease in ischiotibial flexibility in people with knee osteoarthritis has an impact on patients’ performance of activities of daily living.
Material and methodsThis was a cross-sectional, observational correlation study. We recruited participants who were attending consultation and/or physical therapy at a sports medicine and rehabilitation outpatient clinic. We included patients of both genders with an age greater than or equal to 40 years, who were clinically diagnosed with osteoarthritis in one or both knees with radiographic evidence of the disease (recent or under one-year-old weightbearing anteroposterior knee radiographs).
We excluded patients with lumbar pathologies, or who were diagnosed with a neurological disorder and/or with incomplete knee extension (>15° flexion) that may alter the flexibility test due to pain or impossibility of making an adequate lumbar flexion. Patients with poor technique when performing the flexibility test or who did not complete the questionnaires were eliminated. A sample of 30 patients was calculated using a simple correlation formula with a zα value of 1.96 and a significance level of 95% for a two-tailed test, and a zβ value of 0.84 with a power of 80% with a minimum expected correlation of 0.5.
A Lafayette flexometer was built according to the specifications in the Fitnessgram®/Activitygram® test administration manual,18 using a 46cm tape gradiated from −23 to 23cm, with 0 set parallel to the face of the box where the patient's foot was located.
The general questionnaire recorded data, such as age, sex, the Kellgren and Lawrence system for ostheoarthrosis classification, knee or knees affected, time since diagnosis, dominant leg, treatment received, and flexibility measures. The Spanish version of the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) v. 3.1 was used to assess pain, stiffness, and physical function.
The study was approved by the Research Ethics Committee of our institution. Patient consent was obtained after verbally explaining and showing the procedure. The general questionnaire and the WOMAC were applied prior to the BSSR test. In case of doubt or difficulty understanding the text, help was provided. Afterwards, the BSSR test was applied to obtain flexibility measurements.19 The subjects sat on a hard surface, shoeless, with the box in front and their foot flat against it. Patients were asked to flex the knee that was not going to be measured and place the sole of that foot on the floor in line with the other knee or just below. We verified that the hip of the unmeasured knee was flexed at 90° and that the measured knee was at 0° or less than 15° of flexion. With their back and arms straight, and with hands overlapping, they were asked to inhale and exhale, then reach forward with their fingertips. The distance was measured and the process was repeated 3 times for each knee. Results were recorded by the physician. At the end of the test, patients were asked for a second signature, validating their participation and agreement to use their results for the purposes of this research.
We used the statistical program SPSS version 20 (SPSS Inc., Armonk, NY) to conduct data analysis.
Pearson's correlation was used to determine the relationship between mean flexibility and the WOMAC index results.
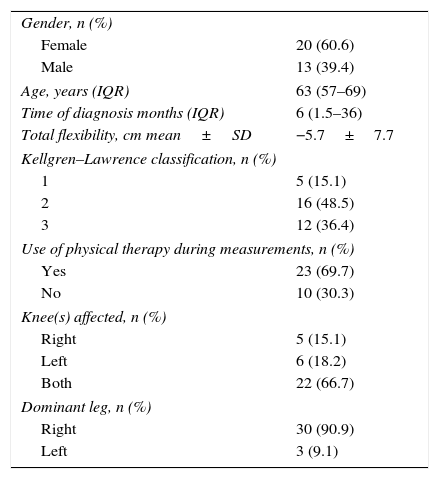
ResultsA total of 33 patients were included in this study. Of these, 20 were women and 13 were men. The median age was 63 years, with a dispersion (IQR) of 57–69 years (Table 1). Using the Kellgren–Lawrence classification, 48.5% of the subjects were grade 2; 69.7% of the patients were receiving physical therapy at the time of the study. Both knees were affected in most patients (66.7%), and 90.9% were right leg dominant. The mean flexibility measure was −5.7±7.7cm.
General characteristics of the study population.
| Gender, n (%) | |
| Female | 20 (60.6) |
| Male | 13 (39.4) |
| Age, years (IQR) | 63 (57–69) |
| Time of diagnosis months (IQR) | 6 (1.5–36) |
| Total flexibility, cm mean±SD | −5.7±7.7 |
| Kellgren–Lawrence classification, n (%) | |
| 1 | 5 (15.1) |
| 2 | 16 (48.5) |
| 3 | 12 (36.4) |
| Use of physical therapy during measurements, n (%) | |
| Yes | 23 (69.7) |
| No | 10 (30.3) |
| Knee(s) affected, n (%) | |
| Right | 5 (15.1) |
| Left | 6 (18.2) |
| Both | 22 (66.7) |
| Dominant leg, n (%) | |
| Right | 30 (90.9) |
| Left | 3 (9.1) |
IQR, interquartile range; SD, standard deviation; cm, centimeters.
A statistically significant correlation between the global WOMAC score (−0.38, 95%CI: −0.68; −0.08, p=0.02) and measuring flexibility was found (Table 2).
When the components were analyzed separately, a statistically significant correlation (−0.40, 95%CI: −0.7; −0.08, p=0.01) was found between total flexibility and functional limitation; however, there was no correlation between pain and stiffness.
There was a significant difference between groups divided by gender and the mean flexibility, age, and Kellgren–Lawrence classification. While this study presented a disparity in gender distribution, our sample resulted in homogeneity when comparing gender to the other variables. There was no correlation between the affected knee and the dominant leg.
DiscussionThe sample of this study was small, yet the results correlate to those – albeit scarce – found in literature.
Our current findings showed that the mean ischiotibial flexibility of our subjects (Table 1) is considerably lower than the age and gender-appropriate measures recommended by the American College of Sports Medicine in healthy subjects, and thus concordant with previously published evidence.7,20,21
Several studies have pointed out the relation between flexibility and musculoskeletal dysfunction. However, there is no published evidence that qualitatively demonstrates that the loss of isquiotibial flexibility affects quality of life and function in activities of daily living.13,16,17
In this study, we found a relationship between WOMAC score and flexibility: the lower the flexibility of the ischiotibial muscles, the greater the pain, stiffness, and functional limitation.
Of the three separate fields the WOMAC test evaluates, there was specifically a significant relation with flexibility and functional limitations, i.e., ischiotibial flexibility has a greater impact on functional limitation, and even though it has a correlational tendency with pain and stiffness, it was not statistically significant.
While it was not the purpose of this study, we found some interesting data: the greater the Kellgren–Lawrence classification, the greater the pain and functional limitation. Mean flexibility was also more impaired in those with a grade 3 in the Kellgren–Lawrence classification than those with grades 1 and 2. Stiffness was also greater in grade 3 knee osteoarthritis, however it does not obey the descendant order previously found. These results may be affected by the unequal distribution between the grade groups. Even though the majority of the patients said they were right-leg dominant, there was no correlation between this and the WOMAC score or measured flexibility.
This study did not account if patients were actively enrolled in physical therapy, and if they were, if it involved flexibility exercises. Some patients referred to an improvement in flexibility posterior to physical therapy sessions, yet this could not be corroborated due to a lack of control subjects and tracing, as this was not our main objective. Also, although the WOMAC questionnaire evaluates some very specific situations and activities that can cause pain, stiffness and functional limitation, it is not capable of inferring a judgment on the quality of life; it would be interesting to assess if there is a relation between the Kellgren–Lawrence classification, functional limitation, pain, and quality of life.
ConclusionIn conclusion, greater ischiotibial flexibility is associated with less pain, stiffness, and functional limitation. However, its main impact was in functional limitation: greater flexibility resulted in a better performance in activities of daily living.
It would be appropriate to take these results as a substantiated suggestion to provide greater importance to prescribing flexibility exercises during physical therapy in these patients, creating a more integral treatment.
Even so, it is suggested to conduct a study with a larger population of patients that takes accounts physical therapy and quality of life into account as variables.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
FundingThis research was financed with resources from the Sports Medicine and Rehabilitation Department of the Hospital Universitario “Dr Jose Eleuterio Gonzalez”, of the Universidad Autonoma de Nuevo Leon.
Conflicts of interestThe authors do not have any conflict of interest to declare.
The authors would like to thank Sergio Lozano-Rodriguez, M.D. and Alejandro Quiroga-Garza, M.D. for their help in the translation and editing of this manuscript; and Nery Alvarez, M.D. for his knowledge and help in statistical analysis.