Background
Percutaneous endoscopic gastrostomy (PEG) is the procedure of choice for in-patients who need long-term tube-feeding support. Different complications have been described for this procedure. Bleeding is a rare but severe complication. It has been estimated to occur in 0.2 to 2.5 % of cases.1,2 In our previous experience with 223 consecutive PEG procedures performed using the Ponsky technique only one patient developed a gastric wall hematoma after a puncturing of the gastric cavity, requiring surgical treatment. Different endoscopic hemostasis methods exist. Thermal therapy, injection therapy, regional spray methods, and mechanical hemostatic methods have been described.3 This report describes the use of hemo-clips in treating a spurting active bleeding from gastric wall vessel injury during a PEG procedure.
Case report
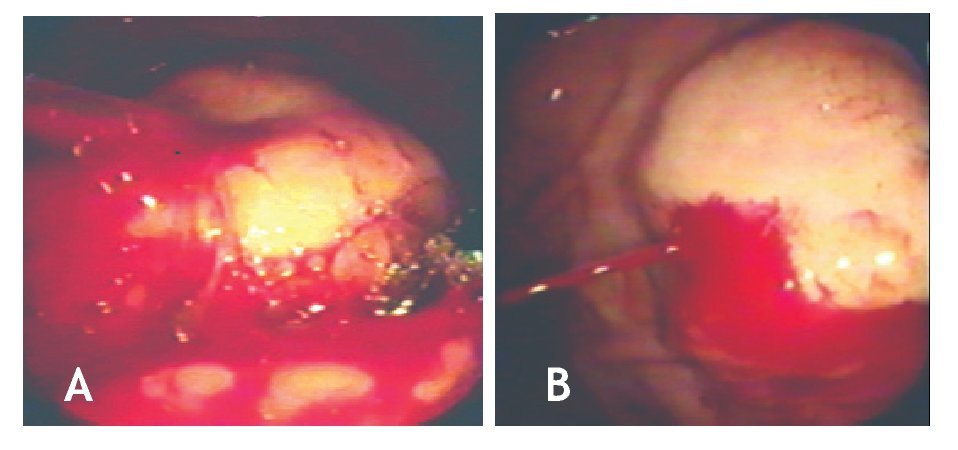
An 80-year-old man with dysphagia secondary to cerebrovascular ischemic disease was submitted to PEG procedure using the Ponsky technique. Complete upper GI endoscopic procedure was normal. After previous asepsis of the abdominal wall, the gastric cavity was fully distended. Transillumination and indentation point in the anterior gastric wall was localized and its correlation with the abdominal wall site was noted. A 1 cm skin incision was performed. Under endoscopic vision and using a 14 gauge needle, the stomach was easily punctured and a guide wire was passed to the stomach grasped and retrieved. With the guide wire in place and prior to passing the gastrostomy tube, bright red blood was noticed in the patient´s mouth. The endoscope was passed again and arterial spurting bleeding was observed in the gastric puncture site (Figure 1).
Figure 1.A: Active bleeding and the guide-wire. B: spurting arterial bleeding.
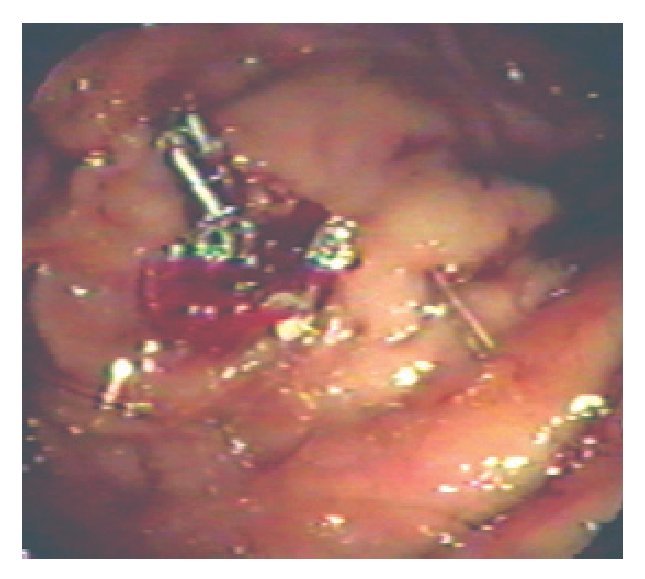
The Teflon needle´s sheath and the guide wire were retrieved. At this time, we decided to treat our patient with hemoclips. We used an Olympus HX-6UR-1 hemoclipping device and type MD-59 hemoclips. Five hemoclips were applied at the bleeding point. Water irrigation was done until complete hemostasis was observed (Figure 2). Ranitidine infusion was indicated and during the first 24 hours no rebleeding occurred. After 72 hours of the procedure a new endoscopy was performed showing the five hemoclips in place and no bleeding stigmata or gastric ulcer. One week later a PEG procedure using the Ponsky technique was performed without complication. After three months the patient is doing well without gastric bleeding or tube feeding problems.
Figure 2. Hemostasis and five hemoclips in place.
Discussion
Different studies have proven the utility and safety of the PEG. Immediate complications such as bleeding and perforation are rare during PEG procedure, and surgery may be needed for most of these complications.4
Active gastrointestinal bleeding is an emergency and remains a common cause of morbility and mortality. With the advance of new endoscopic hemostasis methods the necessity of surgery has been reduced.5 Different methods for endoscopic hemostasis have been described in bleeding lesions of the gastrointestinal tract. Hayashi in Japan, first described the mechanical method such as hemoclip, since 1988 it has been widely use in clinical practice.6,7
The hemoclips function by grasping, compressing and ligating the bleeding vessels. An immediate hemostatic effect is noted and is expected to be permanent if the bleeding vessel is properly grasped. several clips can be used without serious complication.8 In our case, we choose to use hemoclips because we had a good viewing position and considered the probability of a large gastric submucosal vessel injury (≥ 1mm diameter). We are aware that hemostasis for vessels of this size is difficult in most cases.9
Other hemostasis methods may be considered for this kind of complication such as thermal therapy, in this regard, we were concerned about the risk of perforation of the gastric wall after the application of heat.
Given the suspicion of damage to a large gastric submucosal vessel, the banding procedure could have been a good option, but we were afraid of the risk of early dislodgment or late banding ulcer complication. At the third and seventh days after clipping, five and three hemoclips were in place, respectively. No rebleeding or ulcer complication was noted in our patient after three months of follow up. Active bleeding due to gastric vessel puncture during PEG is a very rare complication but represents a high morbility. Most of the time emergency surgery is considered. To our knowledge, this is the first case report about the use of hemoclips to stop bleeding from a gastric wall vessel injury during a PEG procedure.
Corresponding author: Dr. José Alberto González González.
Centro Regional para el Estudio de las Enfermedades Digestivas. Servicio de Gastroenterología. Facultad de Medicina y Hospital Universitario Dr. José Eleuterio González de la UANL. Edificio Dr. Rodrigo F. Barragán 2º Piso. Avenida Francisco I. Madero y Gonzalitos s/n Colonia Mitras Centro C. P. 64460 Monterrey, Nuevo León, México. Telephone: (+52 81) 8348 6068, 8333 3664.
E-mail:joseagonz@yahoo.com
Received: november, 2009. Accepted: november, 2009.