Objective: Apply dual X-ray absorptiometry (DXA) to determine the amount of fat mass, lean mass, and bone mineral density in Mexican schoolchildren with and without obesity.
Material and methods: We performed an observational, analytical, comparative, cross-sectional study of 80 Mexican schoolchildren who attended the Nutrition Clinic of the Pediatric Medical Center in Monterrey, Mexico during the period of January to April 2005. Body mass index (BMI) was determined to classify the participants according to the growth charts of the Centers for Disease Control and Prevention. Two groups of 40 children each (with and without obesity) were formed and DXA was carried out on each individual. Cronbach’s Alpha was used to determine instrument reliability and the Kolmogorov-Smirnov test was used to test the normality of numerical variables. Means were compared using Student´s t test.
Results: Statistically significant differences were found in fat mass (p≤0.001) and lean mass (p≤0.001), but not in bone mineral content (p=0.051) between both groups.
Conclusions: Differences exist in fat mass and lean mass in both groups, but not in bone mineral content between both groups. A significant positive correlation was found between fat mass, determined by DXA, and BMI in schoolchildren with and without obesity.
Introduction
The prevalence of obesity is increasing in children and adolescents in developed and developing countries and has become a health problem of great importance.1 According to the National Health and Nutrition Survey, the combined national prevalence of obesity in 2012 in school-age children, using the World Health Organization (WHO) criteria, was 34.4% (19.8% and 14.6%, respectively).2 Although the body mass index (BMI) remains the most widely used method for clinical diagnosis of obesity, it is not a measure of body composition because it only provides information about global changes in the body, without specifying the components that are specifically affected in situations of malnutrition and/or obesity.3,4
There are several ways to indirectly measure adipose tissue. Among these are 2 kinds of impedance analyses: single frequency and multi-frequency, which both calculate lean body mass; however, their accuracy varies with hydration and the presence of body fluids, although they have the advantage of being non-invasive and accessible. Likewise, there are other more sophisticated methods to assess body composition: dual X-ray absorptiometry (DXA), computerized tomography (CT), and magnetic resonance imaging (MrI), with the latter 2 being used for research purposes. Although various methods are available, some have a number of disadvantages, such as low precision and a need for the individual’s cooperation. This makes it necessary to find an easy, reliable, and economical method that can be used in professional clinical practice.
DXA is a method commonly used to determine bone mineral density, but it also accurately estimates fat mass and fat-free mass.5,6 It is relatively fast and safe, providing high accuracy and requiring little patient cooperation.7 Thus DXA has some advantages over MrI, such as the relative ease of access and simplicity of measurements.8,9
This highlights the importance of this study for clinical application in children with and without obesity with respect to body composition by DXA, relating this to BMI and associating the latter with metabolic abnormalities related to excess adipose tissue.10 The purpose of this study is to use DXA to determine whether there is any difference in the content of fat mass, lean mass, and bone mineral density in Mexican schoolchildren with and without obesity.
Material and methods
We developed an observational, cross-sectional, analytical and comparative study. The participants were selected by convenience and incidental sampling. The study included 80 Mexican children (6-12 years), who attended the Nutrition Clinic of the Child Medical Center in Monterrey, Mexico, during the period of January to April 2005. All patients included in the study were sedentary and were divided into 2 groups: one group of 40 non-obese schoolchildren with a BMI < 85th percentile only within the normal weight range and another group of 40 obese students with a BMI ≥ 95th percentile. Female students who presented their menarche, both male and female patients with onset of puberty, patients taking corticosteroids and patients with conditions such as Prader-Willi, Brader-Biedl, Ahlstrom, and Cohen syndrome were excluded. The study was approved by the research Ethics Committee of the “Dr. José Eleuterio González” University Hospital of the Universidad Autónoma de Nuevo León (UANL, by its Spanish acronym). Patients older than 8 years provided assent and parents of all patients signed an informed consent before entering their children in the study.11
Prior to the DXA study, a complete pediatric medical examination was performed and the patient’s weight was obtained with a scale with a 100 g precision (Health-O-Meter®, McCook, IL, USA). Height was measured using a stadiometer to the nearest 1 mm (SECA model 242, Hammer Steindam, Hamburg, Germany). With these results, BMI (weight/ height2) was obtained.
Body composition analysis was performed by DXA (QDr, Hologic Inc., Bedford, MA, USA), which provides measurements of the following variables: fat mass in grams, lean mass in grams, and bone mineral content. Data were tabulated using Microsoft Excel®. Cronbach´s Alpha coefficient was used to obtain the reliability of the instrument and the Kolmogorov-Smirnov test was used to determine the normality in the numeric variables. Frequencies and percentages are used for descriptive statistics, as well as measures of central tendency (mean, median) and standard deviation (SD). Finally, Student´s t test was used for comparison of data.
Results
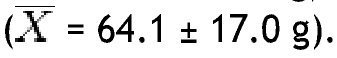
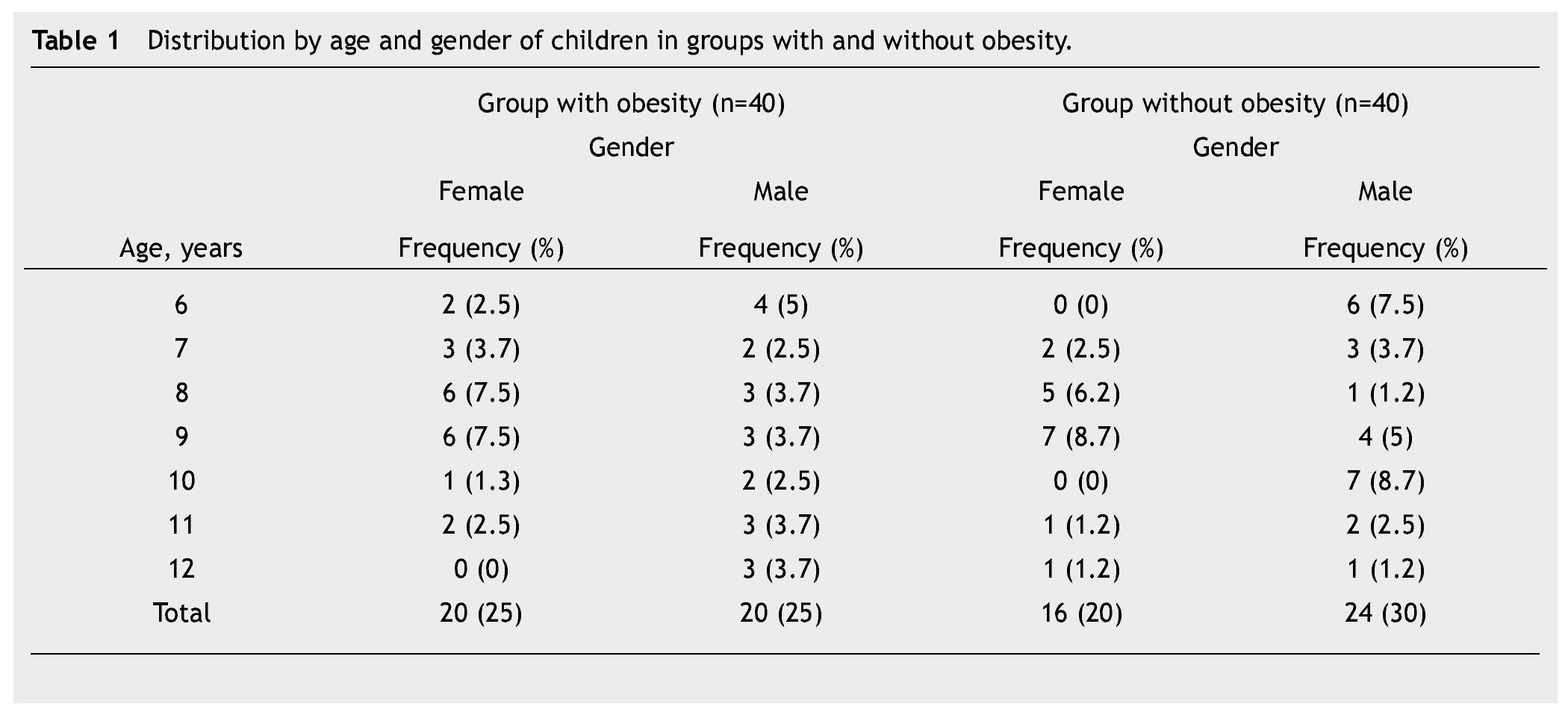
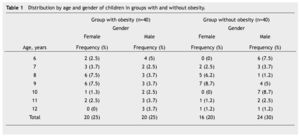
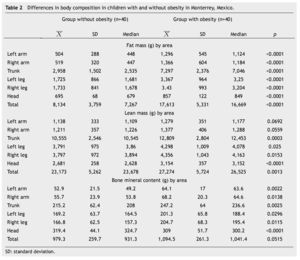
In this study, BMI was determined in 80 schoolchildren who were classified as obese and non-obese, according to the Centers for Disease Control and Prevention growth charts and divided into 2 equal groups. Children of different ages were included and the median age for both groups was determined; in the non-obese group the median was 9 years, and in the obese group it was 8.5 years. The demographic characteristics of the groups are shown in Table 1. Regarding BMI, the girls in the non-obese group (n=16) had a mean of 17.27 Kg/m2 and the boys (n=24) 18.45 Kg/m2; in the obese group, girls (n=20) had a mean of 24.49 Kg/m2 and boys (n=20) 25.14 Kg/m2. Fat mass in grams, lean mass in grams, and bone mineral content were determined in both groups, obtaining the mean, median, SD and p value for the different parts of the body, and as a whole (Table 2). With regard to the analysis of fat mass in grams in the different parts of the body, the non-obese group showed that the greatest amount was located in the trunk
, while the lowest value was found in the left arm
In the group with obesity, for fat mass in grams according to the different parts of the body, the trunk was also the area with the highest value
with the head scoring the lowest
In the non-obese group, lean mass in grams was greater in the trunk
and lowest in the left arm
When lean mass in grams was determined in different areas of the body, in the obese group it was observed that the trunk had the greatest amount
and the left arm the lowest
Analysis of bone mineral content in grams in the non-obese group showed a greater amount in the head
and the lowest in the left arm
In the obese group, the bone mineral content in grams was greatest in the head
with the lowest content in the left arm
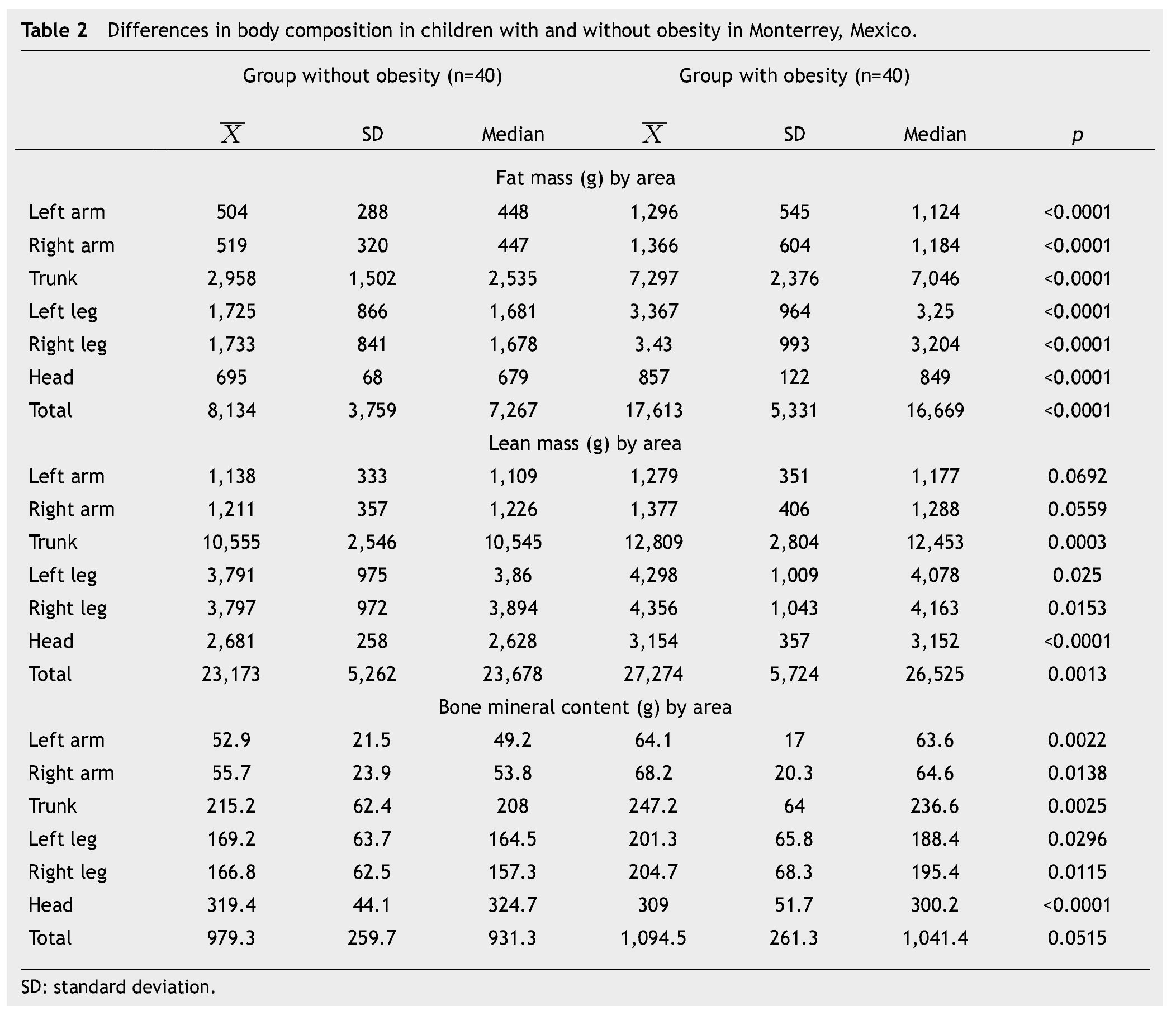
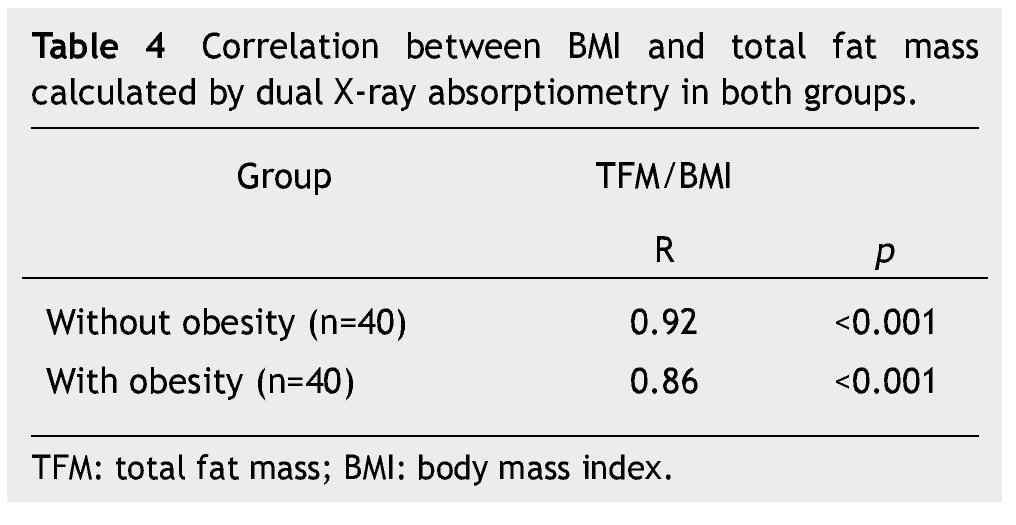
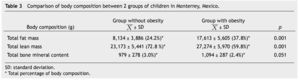
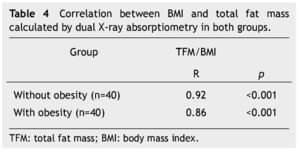
Moreover, body composition as a percentage of total fat mass, lean mass and bone mineral content were determined in both groups. When comparing the means of both groups, significant differences in fat mass and lean mass were found. In the obese group a mean bone mineral content of 1,094 was found and in the non-obese group of 979, which, although it was not statistically significant (p=0.051) showed a trend toward increased bone mineral content in obese children, which is probably due to dietary and environmental factors (Table 3). A significant positive correlation was found between BMI and total fat mass in grams calculated by DXA (Table 4).
Discussion
Although a consensus on the clinical parameter with the most discriminative ability to detect and quantify excess body fat has not been reached, most agree that the most suitable method for estimating body fat should be based on anthropometric measures because of its accessibility, simplicity and reproducibility, harmlessness, and low cost. The BMI is an indicator of body fat, but the relationship between BMI and percentage of body fat varies among individuals. Therefore, it is important to distinguish whether the excess weight is truly due to fat or muscle since we must not forget that children who are overweight but do not have excess fat do not have an increased health risk.12-15
DXA is becoming an extremely useful tool for assessing changes in bone mass, muscle mass, and especially fat mass not only in adults but children and adolescents.
Haroun et al.16 analyzed body composition in obese and non-obese Ukrainian children analyzing lean mass. Their study showed that lean mass is different in obese and non-obese children. Body water and mineral content are higher in obese children. These results are consistent with our data regarding the analysis of lean mass, where we also found statistically significant differences between the 2 groups. Again, as with fat mass, the trunk had the greatest percentage of lean body mass in both groups. Likewise, boys had the highest amount of lean mass.
The trunk was the area where the greatest amount of fat was found in both groups; this amount showed statistically significant differences between children with and without obesity. These results are consistent with data published in medical literature in studies using the same method to assess body composition.17 We found that boys in both groups showed more body fat than girls, while female patients with obesity often have early, accelerated and rapidly progressive puberties compared to their non-obese peers, leading to an earlier presentation of pubertal changes in body composition, the group of female patients in our study had not yet presented pubertal changes. The distribution of fat mass is clinically important because these deposits in the thoracoabdominal region could be predictive in children with diseases such as diabetes and hyperlipidemia, among others.
We found a positive and statistically significant correlation between BMI and fat mass in both groups of Mexican schoolchildren, making it possible to conclude that this index can also be applied to the Mexican population. The results of our study show that BMI is an indicator of adiposity and it correlates with fat mass determined by DXA. These results are consistent with those described in other publications. Pietrobelli et al.18 found a correlation between BMI and percentage of body fat measured by DXA in ranges of 0.85 and 0.89 for children 5 to 19 years of age.
Leonard et al.19 mentioned in their research that obesity during childhood and adolescence is associated with increased bone density and body mass. It is also known that estrogen plays a role in female patients who have already submitted their menarche and likewise in pubertal male patients; aromatase converts testosterone to estrogen, and these play an important role in bone mass gain. However, this was not the case in our study as none of the patients had onset of puberty. In our study, the determination of bone mineral content showed no statistically significant difference between the 2 groups. These data do not agree with what is described in medical literature,20-22 although it is probably due to dietary and environmental factors as described by Jurimae23 in Estonia, who conducted a study on the factors affecting bone density and bone mineral content. These factors include age, since 90% of bone mass is reached at age 18 for women and 22 years for men, making those the best ages for evaluation; nutritional status, which should be taken into account since obese patients often have accelerated bone mineralization, with advanced bone age and size above the familiar; and physical activity, with the latter playing an important role in bone density development. Likewise, there are other rare diseases that affect bone mineral density, namely Turner syndrome, Noonan syndrome, Klinefelter syndrome, Kallman syndrome and others associated with hypogonadism, congenital adrenal hyper-plasia, Cushing’s endogenous syndrome, rickets, renal tubular acidosis, deletions of 22q11, hypo and hyperthyroidism disorders, hormone deficiency and growth resistance, parathyroid disorders, kidney disorders, inactivating and activating mutations of GNAS, use of loop diuretics, bone dysplasias and rheumatic diseases.
By using DXA, we were able to assess its application in children. One of its main advantages is its low radiation dose, plus the pediatric patient is at an age to cooperate comfortably during the procedure, therefore there is no need for sedation and it is very quick. It would be desirable in the future to expand the sample size and classify patients by pubertal stage to establish baseline reference values. It is important to continue studies involving DXA, so that it becomes a useful tool for assessing changes in fat mass, lean mass, and bone mineral content in childhood, to unify reference values.
Conflicts of interest
The authors have no conflicts of interest to declare.
Funding
No financial support was provided.
Received: February 2014;
Accepted: May 2014
* Corresponding author:
Pediatrics Department,
“Dr. José Eleuterio González” University Hospital.
Francisco I. Madero and Gonzalitos Avenue,
Mitras Centro, Z.P. 64460, Monterrey, N.L., Mexico.
Telephone: (+52 81) 8348 5421.
E-mail address: delaocavazos@yahoo.com (M. E. de la O-Cavazos).