Since 1999 we have been studying and treating patients with suspected inherited and/or acquired thrombophilia. Some of them have been referred to us by other specialists, mainly ophthalmologists and neurologists, but interestingly, most of them have come to our clinic referred to by friends or relatives, this being most likely, to our regret, a reflection of the importance that other specialists place on this condition.
Diagnosis
Inherited thrombophilia is a rather common condition which explains several cases of thrombosis. An inherited thrombophilic condition should be suspected in cases of: Thrombosis in individuals of less than 45 years, thrombosis in unusual sites, thrombosis without other triggering conditions, resistance to antithrombotic treatments, recurrent miscarriages and a family history of thrombosis. Most cases of thrombosis in these persons present themselves when exposed to other acquired thrombophilic conditions, the most frequent ones being estrogen treatment, puerperium and prolonged immobilization.
In the vast majority of cases, patients coming to our clinic have been studied incompletely by other physicians and given empirically antiplatelet drugs, anticoagulants or both. Many of these patients have been frightened by their physicians about having a potentially mortal disease at a young age.
a) Thrombophilic screening
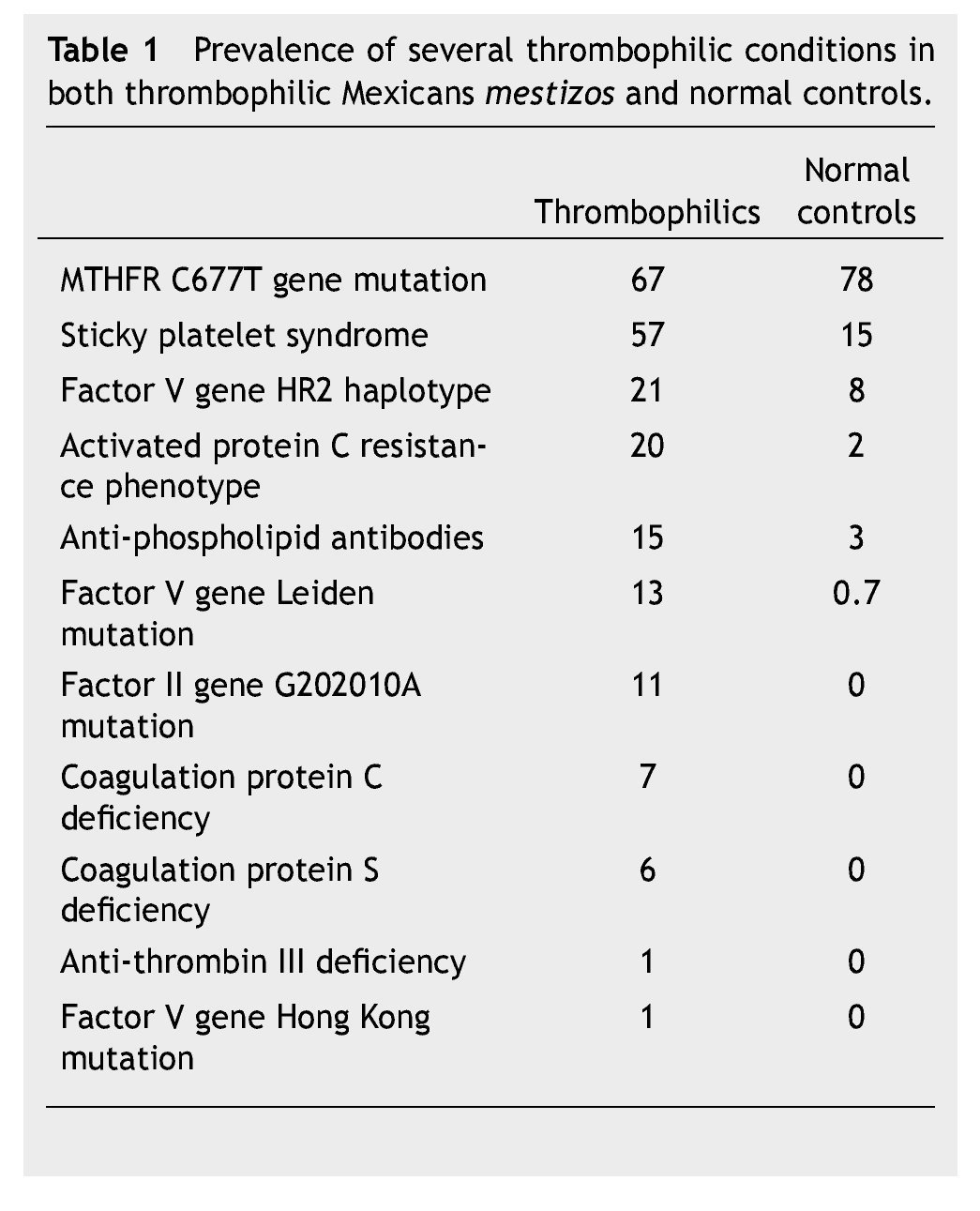
Stemming from our studies of more than 15 years, we have designed 2 thrombophilic screening sets of studies in Mexican patients being studied for thrombophilia. Table 1 shows the salient inherited thrombophilic conditions which we have identified in Mexicans and which were used to design these 2 thrombophilic profiles:
1. Full thrombophilic screening profile: MTHFR C677T gene mutation, investigation of the sticky platelet syndrome, activated protein C resistance aPCR phenotype, factor V Leiden mutation, HR2 haplotype of the factor V gene, anti-phospholipid antibodies, factor II G20210A gene mutation, protein C levels, protein S levels, antithrombin III levels, PnH phenotype in red and white blood cells, JAK-2 V617F gene mutation, and lupus anticoagulant
2. Limited thrombophilic screening profile: MTHFR C677T gene mutation, investigation of the sticky platelet syndrome, aPCR phenotype, and anti-phospholipid antibodies.
We encourage all patients to have the full laboratory workup done, since the chances of identifying the thrombophilic conditions are above 90%, provided all the workup is done. We reserve the limited profile for patients who are unable to defray the cost of the full workup. Before ma- king the set of studies, we instruct the patients to stop both antiplatelet drugs and/or anticoagulants, and to switch into low molecular weight heparin 5-7 days before drawing the blood samples. Most of the times we identify 2 or more inherited thrombophilic conditions which coexist with another acquired thrombophilic state in order to develop a full blown thrombotic episode.
Treatment
Once the diagnosis is done, employing the above mentioned studies, we make the following recommendations to the patients:
a) Sticky platelet syndrome (SPS)
This inherited condition leads into both arterial and venous thrombosis and, until recently, its true importance in medical literature had been neglected. Patients with the SPS rethrombose when given oral anticoagulants; they must be treated with antiplatelet drugs. Aspirin (100 mg/day) is adequately tolerated by more than 90% of patients; the rest are to be given clopidogrel or other antiplatelet drugs. The test to define SPS must be repeated 4 weeks after starting aspirin; if the aggregation profiles normalize it must be kept indefinitely; less than 10% of individuals need other antiplatelet drugs to reverse the platelet hyperaggregability. SPS patients, adequately treated, have a less than 5% chance of re-thrombosing.
b) MTHFR C677T gene mutation
This genetic condition probably is not, by itself, enough to create thrombophilia, but added to other ones, it may have significance. On the other hand, the prevalence of this mutation in the normal population in Mexico is extremely high. Since this mutation may lead into hyperhomocystinemia which may be aggravated by folic acid deficiency, we recommend folic acid, 5 mg/day, indefinitely to individuals displaying this gene mutation and having suffered a thrombotic episode.
c) Activated PCR aPCR phenotype
This condition can be either inherited or acquired. In Mexicans mestizos the acquired forms (antiphospholipid antibodies, increased factor VIII levels) are considerably more frequent. Patients with inherited forms of aPCR who have had a thrombosis probably need an anticoagulant indefinitely. We tend to use the new oral anticoagulants (NOACs) more than vitamin K antagonists and prefer rivaroxaban which is used once a day. Individuals with acquired forms of aPCR need the anticoagulant at least while the laboratory phenomenon is present.
d) Oother inherited conditions
Protein S deficiency, protein C deficiency and anti-thrombin III deficiency, all of them very infrequent in Mexicans mestizos, probably need lifelong anticoagulation. Again, we tend to use the NOACs more than vitamin K antagonists and prefer rivaroxaban which is used once a day. NOACs are significantly more expensive than vitamin K antagonists, but in the long turn, needing no laboratory control and being less related to severe hemorrhages, may be a good option.
Conclusion
With a full laboratory workup, we are now able to identify inherited and acquired thrombophilic conditions in more than 90% of individuals having a clinical marker of thrombophilia. These studies should ideally be done in persons studied and treated by cardiologists, angiologists, gastroenterologists, neurologists, gynecologists, ophthalmologists and other specialists dealing with either arterial or venous thrombosis, in order to properly identify the conditions and prevent future re-thrombotic episodes. Even hematologists still consider these studies and treatments as experimental or non-evidence-based. As a result of studying these conditions in more than 500 Mexicans mestizos, we have been able to define thrombophilic profiles, which could be used to both identify these diseases and define the more adequate treatment.1-16
Received: April 2014;
Accepted: June 2014
* Corresponding author:
Center for Hematology and Internal Medicine.
3710 8B Sur Street, Z.P. 72530, Puebla, Pue., Mexico.
Telephone: 01 (222) 243 8100. Fax: 01 (222) 243 8428.
E-mail address: gruiz1@clinicaruiz.com (G. J. Ruiz-Argüelles).