Functional dyspepsia is a highly prevalent disease worldwide. Its symptoms are manifested as pain (burning or not) in the upper abdomen and early satiety, postprandial fullness, bloating, nausea and belching. For its study and treatment, it is divided into 2 syndromes: epigastric pain, which is meal unrelated, and postprandial distress, which as the name suggests, are meal related symptoms. These 2 syndromes frequently overlap.1
The term functional dyspepsia implies a patient with upper digestive symptoms whose endoscopy reveals a normal stomach and duodenum or with minimum changes, the Rome III criteria diagnoses this disease; nevertheless, recent studies suggest the need to modify the temporality criteria. categorizing patients into 2 syndromes has therapeutic implications, which are based on pathophysiological mechanisms, considering that patients with epigastric pain may have hypersensitivity or a Helicobacter pylori (H. pylori) infection, while patients with postprandial distress may suffer fundic-relaxation or gastric emptying issues.
Within the therapeutic approach of functional dyspepsia, there are important pharmacological and non-pharmacological measures, including:
Non-pharmacological measures
a. Diet
We suggest avoiding foods such as: soft drinks, coffee, tea, chocolate, mint, peppermint, garlic, onion, tomato, pepper, gum, spices and citrus, as well as excessive amounts of fruit and vegetables, especially when symptoms suggest problems with gastric emptying. once the patient improves, these foods should be re-introduced in an orderly fashion to test tolerance.
b. Upper gastrointestinal (GI) endoscopy
It is necessary for a functional dyspepsia diagnosis, yet not for all patients. Indications include: recent onset dyspepsia in people older than 50, weight loss, nocturnal symptoms, and evidence of anemia or digestive hemorrhage. patients with dyspepsia benefit from the endoscopy, because this has proved to reduce anxiety rates by ruling out cancer or a peptic ulcer.
c. Avoid alcohol, tobacco and non-steroidal anti-inflammatory drug (nsaIDs)
These are unarguably dyspepsia generators and are associated with peptic ulcers. We suggest avoiding them due to their GI toxicity.
d. Psychoeducation and psychotherapy
Prevalence of depression and especially of anxiety is high in patients with dyspepsia. It is important to detect such diseases and treat them, since these may increase the perception of symptoms. In our experience, symptoms such as nausea are associated independently with anxiety and the degree of anxiety is positively correlated with the intensity of the symptoms.2
We strongly recommend the use of tools like the in hospital anxiety and Depression scale survey (validated in Me- xico) as well as the Rome psychosocial alarm survey for anxiety and depression detection in patients with dyspepsia.
Pharmacological measures
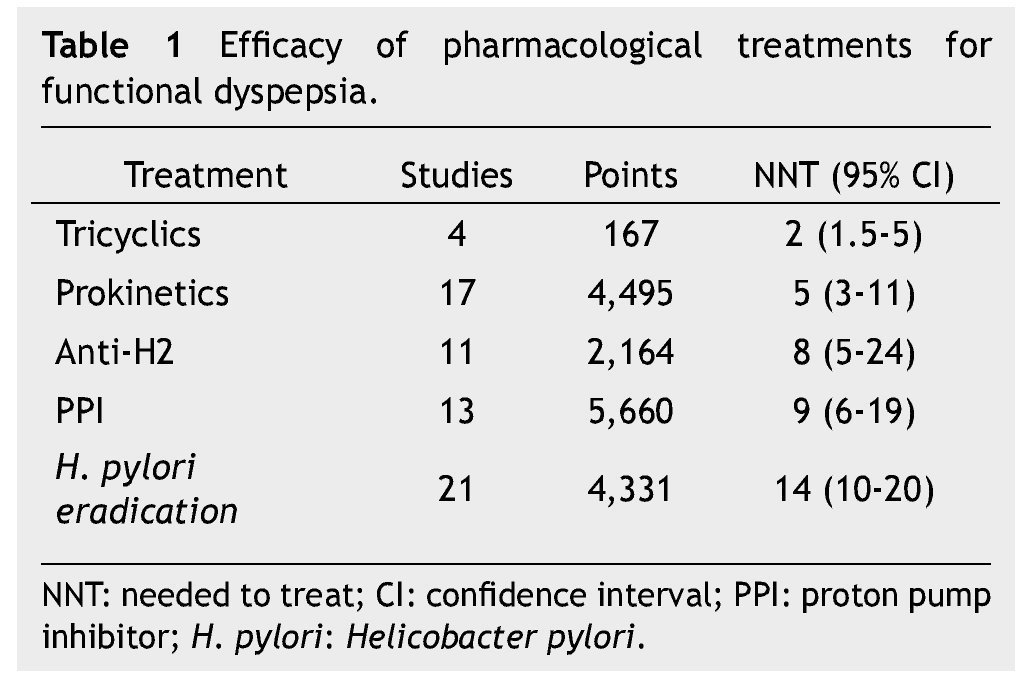
Finding pharmacological measures that function better than the placebo is definitely a hard task in functional disorders, because placebos have a very high effect to control dyspepsia, from 30% up to 70%. In case of functional dyspepsia we must remember that we are dealing with 2 diseases instead of just one (epigastric pain and postprandial discomfort), which may coexist. Thus, we must examine patients for the presence of each and every one of the symptoms, which will tell us the pathophysiological aspect involved, and enable us to treat the patient based or their symptoms. Most of the published clinical trials about functional dyspepsia treatment evaluate for both types of dyspepsia; hence, the results must be carefully interpreted. The efficacy of different pharmacological treatments for functional dyspepsia is variable (table 1).
Available pharmacological treatments for dyspepsia:
• H. pylori eradication treatment: one of the patient’s biggest fears about dyspepsia is having H. pylori, the patients show a major concern caused by a microorganism, which may have been in their stomachs for a long time already. Eradication treatment has an effectiveness measured as a number needed to treat (nnt) of 14, which in specialty care is not too effective. nevertheless, a recent clinical trial shows that it is a good strategy in primary care medicine as well as in places of high prevalence like our county. some patients benefited by this treatment are those who manifest pain.
• Anti-secretory drugs: Both type-2 anti-histaminergic pharmaceuticals (i. e. ranitidine) as well as proton pump inhibitors are medications of moderate efficacy with an nnt of 8 and 9, respectively. patients who may be benefited by the use of these medications are those with burning pain, overlapping with gastroesophageal reflux (frequent in our population, up to 50%). however, it is important to know that the patients who benefit the least are those with postprandial distress, considering that gastric emptying studies have proven that proton pump inhibitor (ppI) reduces solids rate and this could worsen the symptoms.
• Prokinetics: these are useful medications in the treatment of postprandial distress syndrome; however researchers in Us forget them because its therapeutic dosage approaches the level of dosage which causes adverse effects. nevertheless, when these are used wisely, it gives dyspepsia patients a major benefit with an nnt of 5. It is important to highlight that there is a considerable amount of prokinetics available in Mexico, but we must chose the one that, in addition to being effective, has an acceptable safety profile.
• Antidepressants: highly effective medications in the treatment of dyspepsia since they work as visceral analgesics. It is important to highlight that the use of these medications is for pain management. however, we must evaluate the presence of subjacent anxiety or depression for their treatment.3
Selective serotonin receptor inhibitors have only proved to have a positive effect over quality of life but not in pain. A recent study showed preliminary results demonstrating that amitriptyline is better than a placebo for dyspepsia management, yet not escitalopram. Tricyclic antidepressants are modulators of the perception of pain; their prescription in the treatment of dyspepsia should follow the concept of “low and slow”: effective dosages in dyspepsia tend to be lower than those for depression and their therapeutic effects tend to be noticed sooner than in depression. This treatment’s effectiveness is proven with an nnt of 2. It is important to consider that before the prescription of a tricyclic, organic diseases must have been ruled out because these medications have been demonstrated to be effective for pain management in general and it could be masking other causes. We must emphasize and consider that if we want to treat anxiety or depression there are other medications with better results, thus my suggestion would be to refer to a specialist for its management and maintain the tricyclic’s minimum effective dosage. Recent studies have demonstrated that amitriptyline can manage pain, as well as nausea4 (regardless of the fact that one of its effects is to delay gastric emptying) and even can be found in the american college of Gastroenterology gastroparesis management guide because of its effect over this problematic symptom.
Regarding dyspepsia treatment duration the suggestion is 3 months; however, the use of tricyclic as an option can be considered up to 6 months (there is not a well-established time).
Functional dyspepsia is more complex than we think and therapeutic development seems to be stagnant for some years now. Management guidelines are different based on prokinetic availability; always consider H. pylori eradication as a first choice. They suggest subdividing the patient into 2 groups (epigastric pain or postprandial distress); however, it is very frequent that the patient suffers both (up to 50%). Therefore my recommendation is to consider the fact that symptoms are the key to establishing a treatment plan, because they can explain whether the patient is hypersensitive and requires a tricyclic, if the patient has gastric relaxation or emptying issues where a prokinetic would be ideal, or if acid is casual and an anti-secretor would be the best option. Even though we must consider that the best option is probably the combination of 2 or more medications based on the symptoms.
Received: May 2014;
accepted: May 2014
* Corresponding author:
Gastroenterology and Digestive Endoscopy Service,
Social Mexicali Hospital. 1300 Francisco Sarabia Street, Zacatecas,
Z.P. 21070, Mexicali, B. C., Mexico.
E-mail address: floresrendon.md@gmail.com (Á. R. Flores-Rendón).