Objective: Determining the effectiveness of infiltration versus instillation with 7.5% ropivacaine in reducing the intensity of postoperative pain in patients undergoing a radical mastectomy.
Material and methods: Clinical, prospective, and comparative analytical study in a sample of 20 female patients between 20 and 60 years of age, ASA I and II, weight 50-90 kg, who were divided into 2 groups (10 patients each). In Group 1 infiltration with ropivacaine 7.5% (20 ml) was applied prior to closure of the surgical wound, meanwhile in Group 2 ropivacaine 7.5% (20 ml), was instilled into the surgical wound. Pain intensity was assessed by a visual analog scale (VAS) upon extubation. The need for rescue medication and the incidence of nausea and vomiting were measured from 0 to 30 minutes postoperatively and at 2, 4, 8 and 12 hours.
Results: There was no statistical difference between the groups (only the group managed through infiltration required rescue medications), but the infiltration group had a lower perception of pain.
Conclusions: This study reported the same efficacy of preventive treatment of postoperative pain in patients who underwent radical mastectomy for instillation and infiltration with 7.5% ropivacaine and little need for rescue medication postoperatively.
Introduction
Preventive analgesia was described by Crile in 1913 as an option to prevent alterations in the autonomic nervous system resulting from postoperative pain, based in regional blocks with local and general anesthetics.1 Initially, preventive analgesia for postoperative pain treatment was not well accepted, due to controversial results in experimental and clinical research work; however, nowadays its use is being reconsidered.2-5
Underestimated postoperative pain by medical personnel as well as lack of knowledge and adherence to a multimodal analgesic management, are factors accounting for an inadequate therapeutic management of postoperative patients. This has a direct impact on the patient's optimal recovery, in addition to allowing the development of chronic complications following the surgical procedure. Studies published in recent years show a prevalence of moderate to unbearable pain of 11% (in a hospital with an acute postoperative pain unit), and in 70% of the patients who have undergone surgery during the first 24 to 48 hours; nevertheless, prevalence has always exceeded 30%.6
There are surgical procedures such as mastectomies in women, which besides producing pain may cause diverse emotional reactions.7 Breast cancer is one of the 2 most common malignancies in women worldwide and the main treatment for this pathology is surgery.7-10
Despite different therapeutic approaches with several analgesics and routes of administration to avoid pain, the desired analgesic effect is not accomplished in some patients; a reason for this could be the route of administration used or the fact that the strength of the medication may be insufficient.
Radical mastectomy is an extensive and disfiguring procedure, which causes acute postoperative pain due to soft tissue injury of the anterior wall of the thorax. During dissection, tissue traction takes place producing damage to the axons of the intercostal nerves and brachial plexus emergence. There are several anesthetic strategies; some of the most commonly utilized are intercostal nerve blocks, preoperative thoracic epidural block, thoracic paravertebral block, local infiltration blocks, and direct instillation.11-13
Instillation is the introduction of a liquid (by pouring or injection), drop by drop over mucous membranes or the skin. It is a very commonly used method. Postoperative infiltration (direct administration of the analgesic into the surgical area), as a strategy for pain management in this pathology has not been studied extensively and is underconsidered regarding patient management, hence this study. We carried out a comparison between these 2 local analgesic administration techniques by means of a pain scale and the use of rescue medication; by doing so, we attempted to decrease the endocrine response caused by pain and the side effects in the cardiopulmonary and immunology functions that patients with postoperative pain suffer.14
Material and methods
We included female patients scheduled for radical mastectomy at "Dr. José Eleuterio González" University Hospital of the Universidad Autónoma de Nuevo León (UANL), Mexico. The patients agreed to participate in the study by signing an informed consent form. We obtained demographic variables such as age, weight and relevant background. Patients were divided into 2 groups; in Group 1 infiltration with ropivacaine 7.5% (20 ml) was applied prior to closure of the surgical wound, while in Group 2 ropivacaine 7.5% (20 ml) was instilled into the surgical wound. Inclusion criteria required patients to be between 20 and 60 years of age, to have a weight between 110 and 198 lb (50-90 kg), ASA I or II, to be scheduled for radical mastectomy, and have preoperative test results within normal limits. Patients with a history of coagulopathy, radiotherapy, neurological alterations, and previous analgesic or antiinflammatory treatment were excluded. Subsequently, we assessed blood pressure, heart rate, respiratory rate, and pain using a visual analogue scale (VAS) in both groups; in addition the presence of nausea and/or vomiting was measured from 0 to 30 minutes postoperatively and 2, 4, 8, and 12 hours afterwards.
Data was inputted into a database created in Excel® 2010 and analyzed using IBM® Statistic 21; for the quantitative variables, traditional descriptive statistics, measures of central tendency, dispersion and position, as well as the observed frequencies in the qualitative variables were calculated. The values were verified by group through hypothesis tests for median and proportion, according to each variable type (quantitative and qualitative respectively) with a reliability of 95%.
Results
Average age was 49.7 ± 7.8 years for Group 1 (infiltration) and 43.8 + 12.5 years in Group 2 (instillation); there was no significant difference in both groups (p = 0.2234). Average weight was 71.4 kg ± 9.7 for Group 1, and 65.4 ± 14.3 for Group 2; we did not find significant differences between the groups (p = 0.2863).
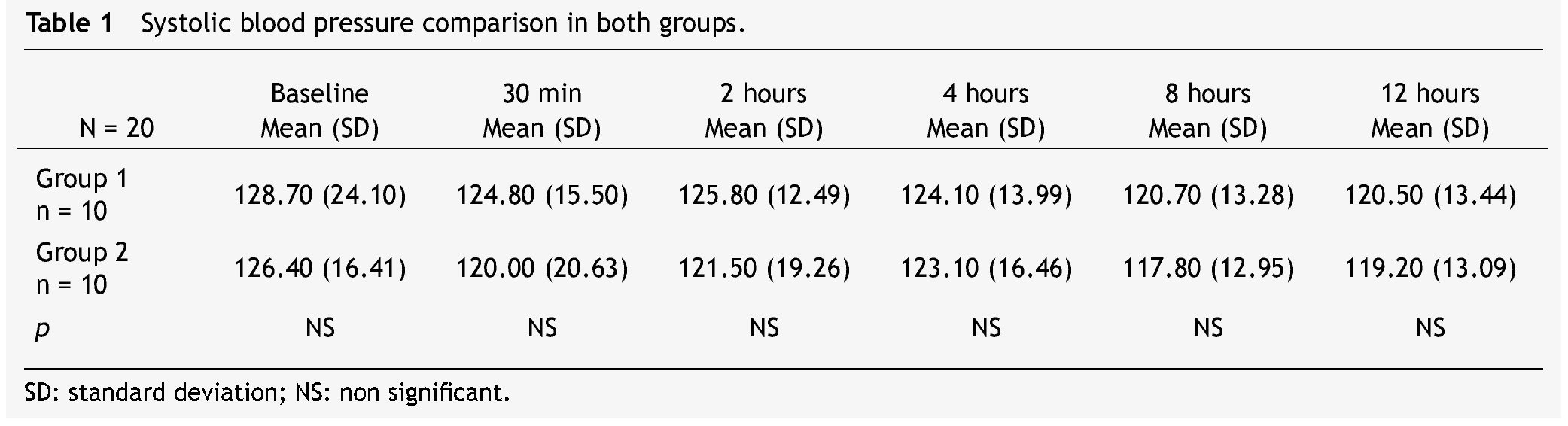
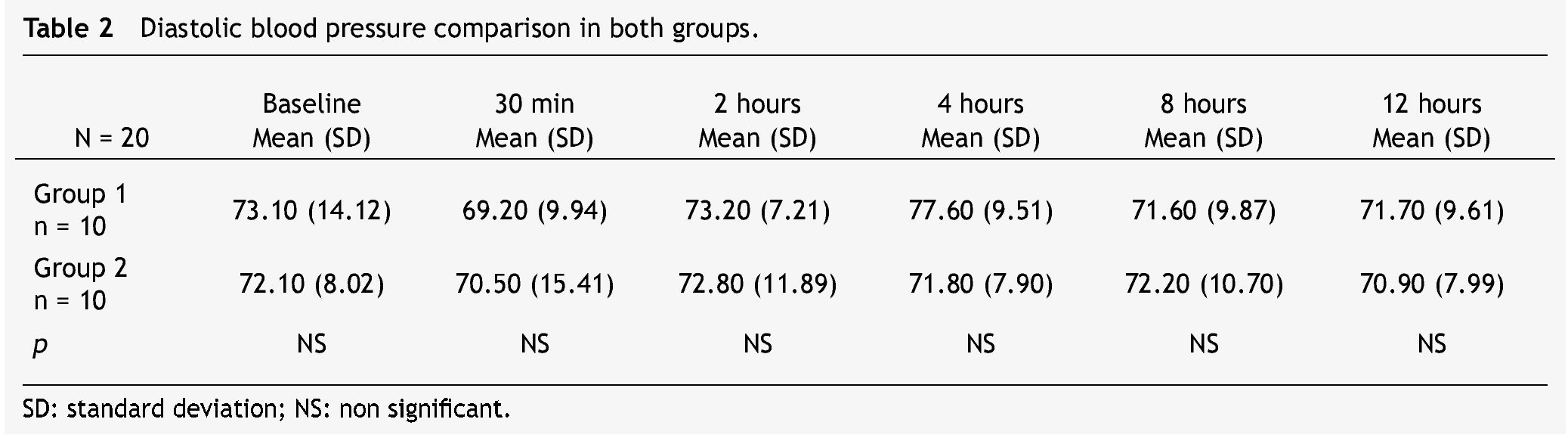
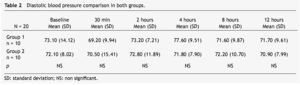
Regarding ASA classification, 50% of the patients in Group 1 and 60% in Group 2 presented with ASA I; the rest of the patients in both groups were ASA II. We did not observe a statistically significant difference regarding vital signs in either group (Tables 1 and 2). No presence of nausea in either group was observed.
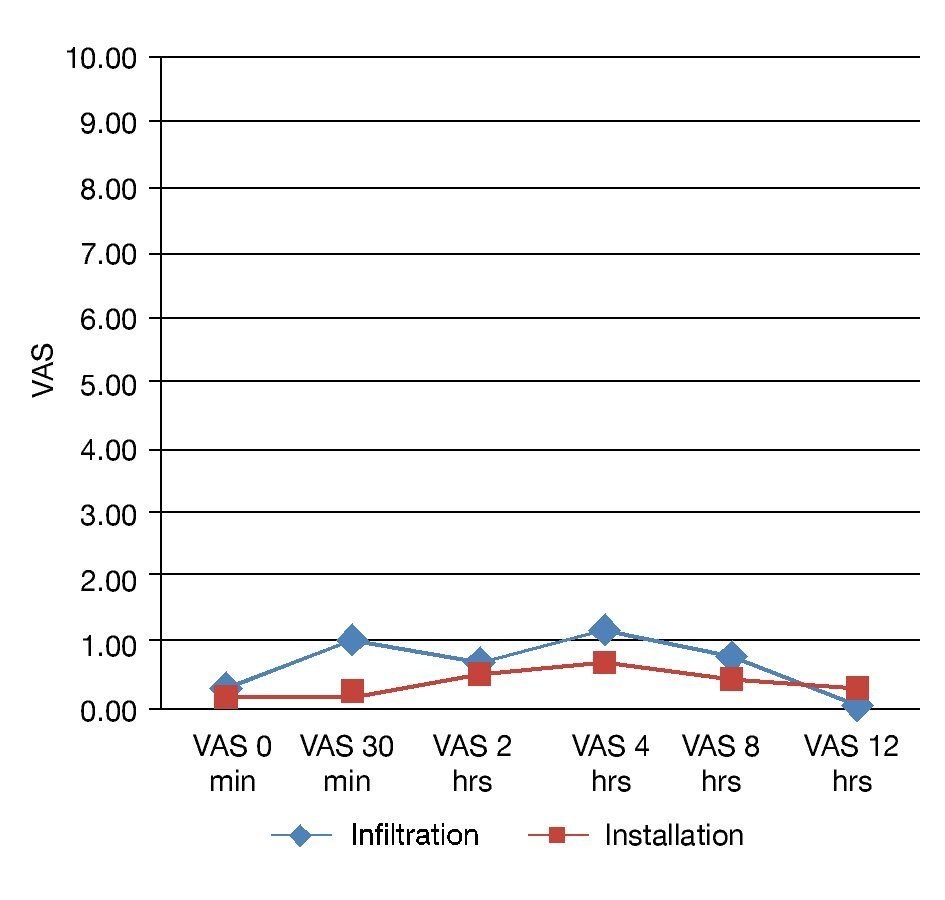
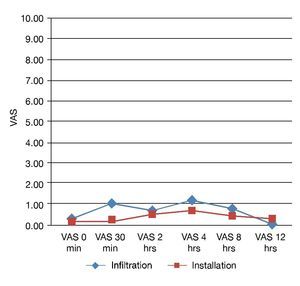
Regarding the VAS results, Group 2 showed better results in all of the evaluation periods, except at 12 hours when results were better in Group 1; however, such differences did not prove to be statistically significant (Fig. 1). A higher number of rescue medication (dexketoprofen 50 mg intravenously [IV]) for Group 1 at 30 minutes and 4 hours was required. In addition, 1 patient from Group 1 required buprenorphine as rescue medication, as she failed to show a decrease in pain. Neither group showed side effects.
Figure 1 Visual analog scale.
Discussion
When cross-referencing both groups, no differences were seen; in both cases the behavior of the variables was the same statistically, mainly concerning pain, except for the group managed with infiltration requiring rescue medication. Despite advances in the knowledge of pain and the constitution of Algology as a new specialty, postoperative pain is frequent in patients after a surgical procedure; if avoided; side effects may be prevented.15-18
Most clinical research studies on preventive analgesia in patients who undergo radical mastectomy refer to spinal blocks. Epidural anesthesia has also been evaluated as anesthesia and management of acute pain during the performance of the mastectomy; yet in the present study we decided not to use it for anesthetic purposes, given the fact that it must be placed in the metamers between C VII y D IV. The puncture of the intervertebral spaces in this region is technically difficult and the position the patient must assume in order to place it may increase the anxiety that involves a morbidity risk due to ventilation problems; this increases if there is a need to sedate the patient.19
Infiltration of the wound and instillation of local anesthetics is another simple and effective technique providing pain relief during the early postoperative period following surgical procedures. There are studies indicating that ropivacaine infiltration on the surgical wound after surgery reduces pain intensity, reducing the requirement of postoperative analgesics and inpatient days. In addition, the amount of applied anesthetics and its absorption through the peritoneal surface provide an additional mechanism of analgesia.
Multiple studies have been performed in order to demonstrate the clinical safety of ropivacaine in animals as well as in humans (5 mg/ml IV infusions).19 The literature reports few studies on instillation and infiltration of ropivacaine 7.5%; thus, having found similar results with this route of administration in the present study, it is recommended as an alternative for optimal postoperative analgesia in patients who undergo radical mastectomy. Incidence of nausea and vomiting, if any, is low.
We found that ropivacaine infiltration or instillation in the surgical wound prior to skin closure showed no significant difference on postoperative pain (except for the necessity of using rescue medication in the infiltrated analgesic group); this was proven when cross-referencing VAS recordings at 2, 4, 8 and 12 postoperative hours between each group (p > 0.05 in every crossing); however, when looking at the numerical behavior, lower values of pain in the "infiltration" group were found. Nevertheless, this could also be caused by the use of rescue medications; in addition, the patient's resistance to the analgesic can also be a variable presented at random. Consequently, the use of a larger sample for future related studies should be the next step, with the purpose of increasing the statistical value in search of establishing whether or not there is a significant difference.
Conclusions
No statistical difference was found between the use of ropivacaine 7.5% infiltrated or instilled in patients undergoing radical mastectomy.
Conflicts of interest
The authors have no conflicts of interest to declare.
Funding
No financial support was provided.
Received: June 2013;
Accepted: October 2013
* Corresponding author:
Department of Anesthesiology,
University Hospital "Dr. José Eleuterio González".
Francisco I. Madero, Mitras Centro, Z.P.
64460, Monterrey, N. L., Mexico.
Telephone: (+01) 8389 1136.
E-mail address: albamillan@hotmail.com, blancaprieto2002@yahoo.com.mx (B. I. Yolanda-Prieto).