Introduction: Maternal mortality (MM) is a reflection of the quality of care given to pregnant women. However, it does not reflect many illnesses and medical complications of women at risk of death, who do not die. Severe obstetric morbidity (SOM) refers to women who are "pregnant or recently postpartum, very ill, who would have died if not for the good health care received".
Objective: to review the incidence of MM and SOM at the Obstetric Service of the University Hospital, Universidad Autónoma de Nuevo León (UANL) in the years 2007-2011.
Material and methods: Observational, cross-sectional, retrospective study, at the Obstetric Service of the University Hospital, UANL.
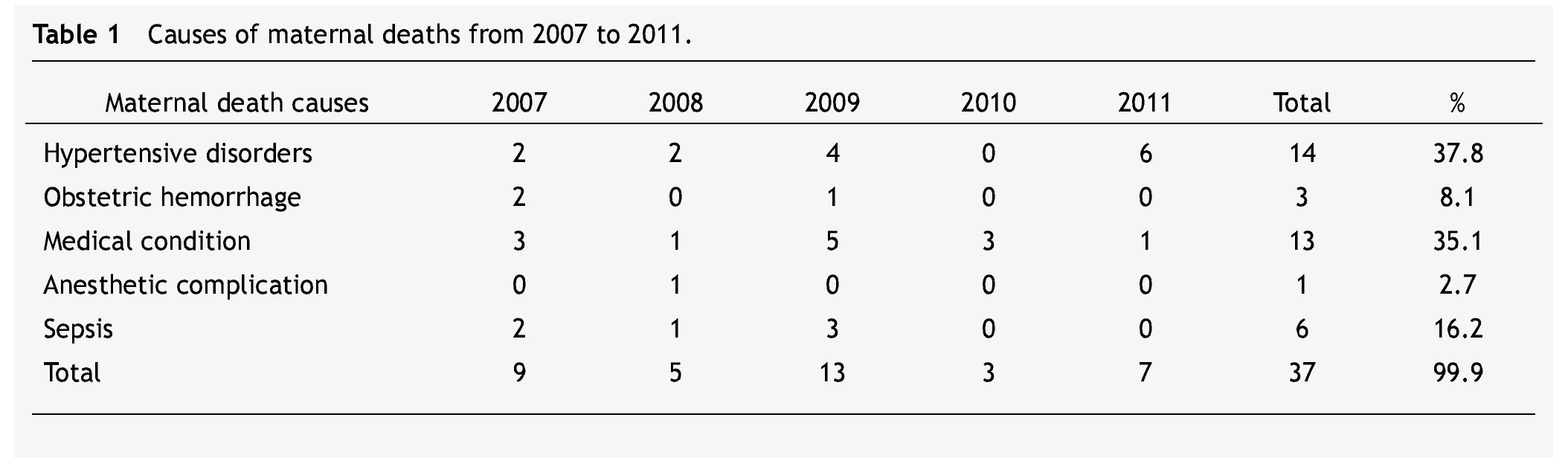
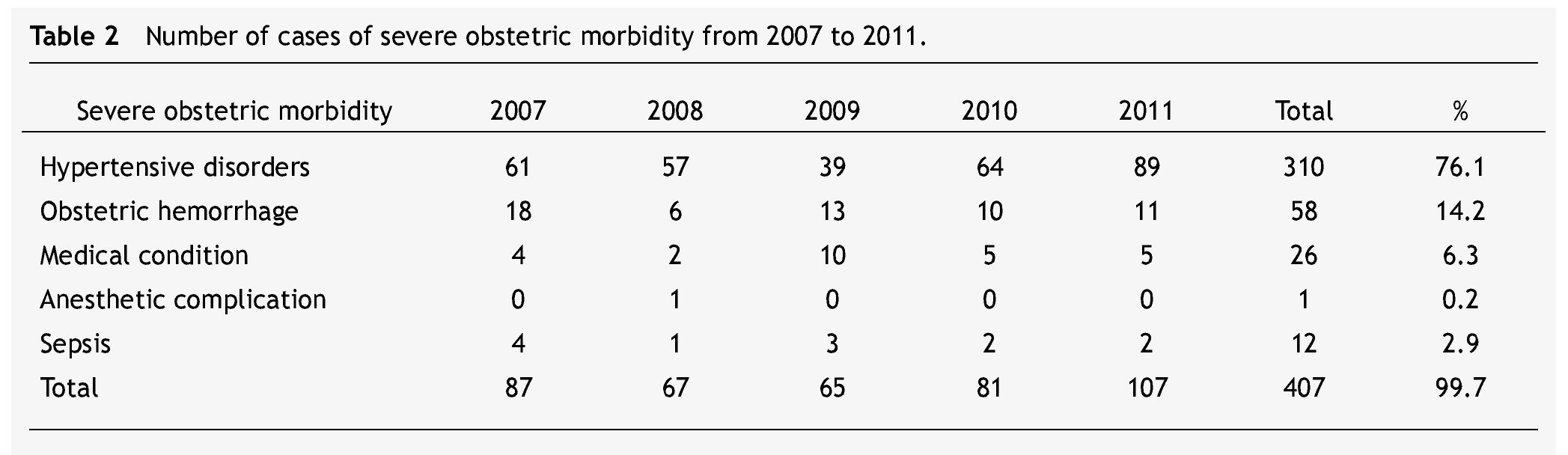
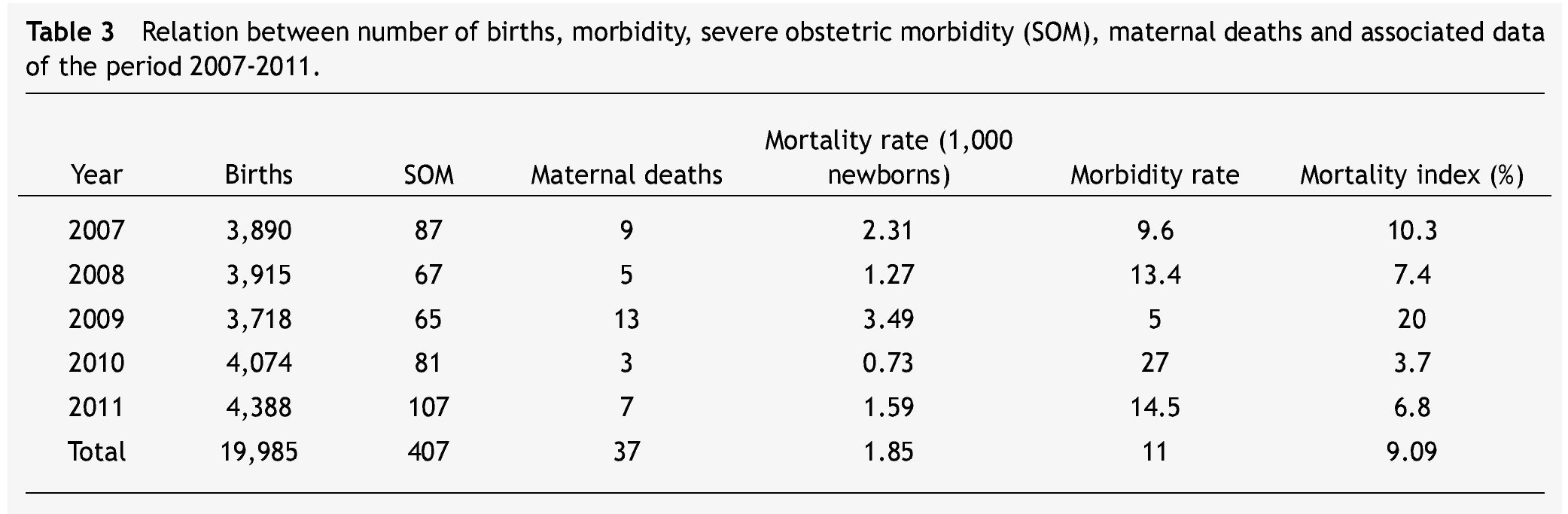
Results: We attended 19,985 births; there were 37 maternal deaths: 14 due to hypertensive disorders (37.8%), 3 due to hemorrhage (8.1%), 13 (35.1%) due to medical complications, 1 (2.7%) due to an anesthetic problem, and 6 due to sepsis (16.2%). Twenty-three (62.1%) maternal deaths were catalogued as direct and 14 (37.8%) as indirect. Of 407 cases of SOM, 310 (76.1%) were due to hypertensive disorders, 58 (14.2%) to obstetric hemorrhage, 26 (6.3%) to medical complications, 1 (0.2%) to anesthetic complication, and 12 (2.9%) to sepsis. The MM rate was 1.85 per 1,000 live births; the incidence of MOS was 81.4 per year, with 1 death per every 11 cases.
Conclusions: the MM and the SOM provide more reliable data on the prevalence of serious complications in obstetrics. This allows us to take preventive measures, offer better medical care, and improve the allocation of resources.
Introduction
Maternal mortality (MM) is an occurrence which reflects the quality of the healthcare system. The World Health Organization defines maternal death as "the death of a woman while pregnant or within 42 days of termination of pregnancy, from any cause related to or aggravated by the pregnancy or its management but not from accidental or incidental causes". Direct maternal death is the result of a complication of the pregnancy, delivery or management of the 2 while an indirect maternal death (IMD) is a pregnancy-related death in a patient with a preexisting or newly developed health problem unrelated to pregnancy. The standard indicator is the MM rate which is defined as the relationship between the numbers of maternal deaths for every 1,000 births.1
Severe obstetric morbidity (SOM) refers to "a pregnant or postpartum patient, very ill, who if not treated appropriately, would result in death".2 It is safe to assume that the same disease processes which cause SOM are closely related to the ones which cause MM. It is possible to study the circumstances surrounding women with SOM, therefore we are able to implement a better surveillance on maternal care.3
In medical literature, different inclusion criteria are used in the selection of SOM cases such as acute organ system dysfunction,4 severe obstetric complications between the 28th week of gestation and 42 days of puerperium,5 admissions to the intensive care unit,6,7 patients receiving a blood transfusion,8 and anesthetic accidents.9
The MM rate and other indexes have been created as a result of the study of such data. These indexes provide a better understanding of the medical problems surrounding pregnant women. Mortality rate represents the number of deaths in accordance to the number of SOM cases, morbidity rate expresses the relationship between SOM cases for every maternal death, and SOM incidence indicates the number of very ill women who are attended per year.10-13
The objective of this study was to review the main causes and incidence of maternal death, as well as SOM at the "Dr. José Eleuterio González" University Hospital of the Universidad Autónoma de Nuevo León (UANL), between 2007 and 2011. Another objective was the analysis of medical and social factors related to the care and attention of obstetric complications and maternal deaths.
Material and methods
In this retrospective, transversal, analytic study, files of patients classified as maternal death, and those who met the criteria for SOM between January 2007 and December 2011 were reviewed.
According to the literature, we considered as SOM pregnant women with severe preeclampsia, eclampsia and HELLP syndrome (a life-threatening pregnancy complication usually considered to be a variant of preeclampsia, named after its characteristics: hemolysis, elevated liver enzymes, and low platelet count); women who had hemorrhage before, during or after delivery higher than 500 ml and who required a blood transfusion; severe medical diseases complicating pregnancy (cardiomyopathy, nephropathy, AIDS, thrombocytopenic purpura, etc.); women admitted to the intensive care unit who underwent an obstetric hysterectomy, laparotomy or pelvic packing, as well as anesthetic accidents and puerperal sepsis cases.4-9
In order to obtain a better data analysis of MM and SOM, we divided the patients into 5 groups: hypertensive disorders, obstetric hemorrhage, medical conditions, anesthetic accidents, and sepsis.
The studied variables were: discharge diagnosis, number of surgeries practiced, blood transfusions, age, schooling, marital status, prenatal care (5 visits or more), gestational age, days of overnight stay, admittance to the Neonatal Intensive Care Unit (NICU -UCIN in its Spanish acronym) and newborn conditions (NB). We calculated the MM rate (number of maternal deaths over the number of live births and stillbirths per 1,000),10 the mortality rate (maternal deaths over the number of SOM cases times 100)11,12 morbidity rate (number of SOM cases divided by the number of maternal deaths) and SOM incidence (number of SOM cases over the sum of periods of time).13,14 We performed descriptive statistics of frequency.
Results
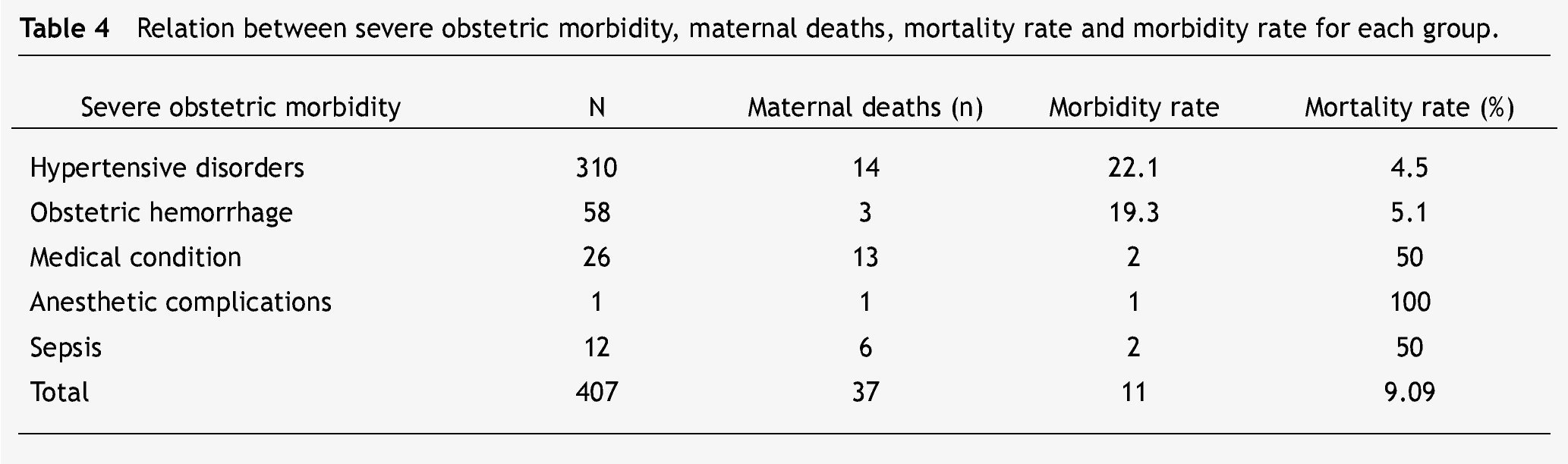
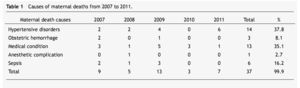
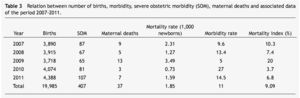
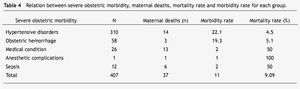
During the 5-year reviewed, 19,985 births took place and 37 maternal deaths were registered (0.18%). The causes of death were as follows: 14 corresponded to hypertensive disorders (37.8%), 3 to hemorrhage (8.1%), 13 to medical complications (35.1%), 1 to an anesthetic problem (2.7%), and 6 to sepsis (16.2%) (table 1). In 23 of the cases (62.1%), maternal death was classified as direct and in 14 (37.8%) as indirect. Maternal death rate was 1.85 per 1,000 born alive and dead. We gathered 407 SOM cases: 310 (76.1%) hypertensive disorders, 58 (14.2%) with an obstetric hemorrhage, medical complications in 26 (6.3%), 1 case (0.2%) with anesthetic complications, and 12 (2.9%) with sepsis (table 2). Mortality rate was 9.09% and morbidity rate resulted in 1 death for every 11 SOM cases (table 3). SOM incidence was 81.4 cases per year. After measuring mortality and morbidity rates within each of the SOM pathology groups, we found that for hypertensive disorders, morbidity rate resulted in 1 death for every 22.1 cases and mortality was 4.5%; in the hemorrhage cases, morbidity rate resulted in 1 death for every 19.3 and mortality was 5.1%; regarding medical complications and sepsis, morbidity rate resulted in 1 death for every 2 and mortality was 50%; for anesthetic complications, morbidity rate was a single case which resulted in death with a mortality rate of 100% (table 4).
Sixty patients underwent hysterectomy (14.7%) and 56 files were reviewed. Background of a previous C-section occurred in 34 cases (60.7%). The diagnosis corresponded to placenta accrete in 30 cases (53.5%), uterine atony in 12 (21.4%), cornual and cervical ectopic pregnancy in 3 (5.35%), uterine myomatosis in 3 (5.35%), uterine perforation in 3 (5.35%), and 3 (5.35%) cases with sepsis. In 2 patients a carcinoma in situ diagnosis was established. In 52 patients (92.8%) blood transfusion was required, ranging from 1 to 25 blood packs with an average of 4.3; fresh frozen plasma was applied in a range between 1 and 40 with an average of 3.8; platelets concentrates were applied in a range between 1 and 33 with an average of 4.4.
Admittance to the NICU occurred in 132 cases (32%) as follows: 80 due to hypertensive disorders (19.6%), 20 due to hemorrhage (4.9%), 24 due to a medical condition (5.8%) and 8 due to sepsis (1.96). Hospital stay ranged from 5 to 90 days, with an average of 10 days.
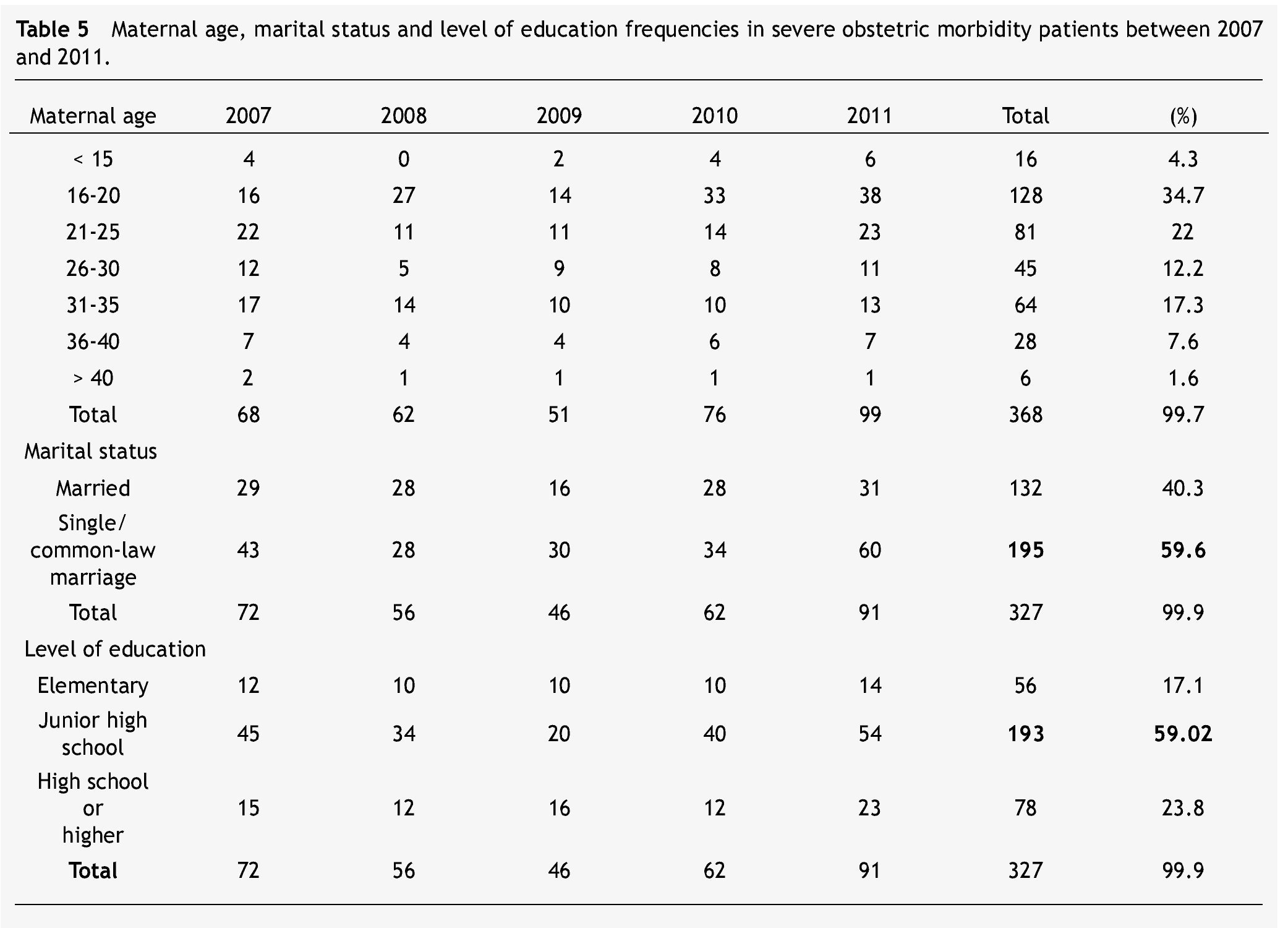
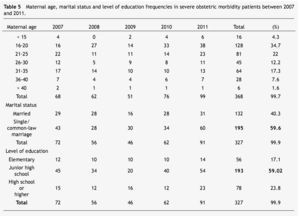
Maternal age was analyzed in 368 cases and ranged from 14 to 42 years, with an average of 25.3. The most frequent age group was under 20 years with 128 cases (34.7%), followed by 21 to 25 years with 81 (22%). As for marital status, the distribution of the 327 cases was as follows: 195 single or in common-law marriage (59.6%) and 132 married (40.3%). Schooling for the 327 cases was: 56 with elementary school completed (17.1%), 193 with junior high school completed (59.02%), and 78 with high school or higher education completed (23.8%) (Table 5). Distribution by gestational age in weeks at the moment of admission was, out of the 327 SOM patients: of 43 cases with 25-30 weeks of age; 93 cases between 31-35 weeks (28.44%); 181 between 36-40 weeks (55.35%), and 10 cases with 41 weeks or more (3.05%). Prenatal care in 327 files was considered positive in 233 cases (71.2%) and negative in 94 (28.7%). Obstetric care in 354 reviewed cases was of 3 uterine curettage (0.84%), 38 deliveries (10.73%) and 313 C-sections (88.41%).
Discussion
Maternal mortality is the result of a series of events which reveal a lack of action to improve the conditions and the exclusion conditions which many women in Mexico live in. Behind every maternal death there is a series of severe socioeconomic problems such as a high child morbidity/mortality rate, malnutrition, orphanage, schooling drop-outs, and a premature start for children in the workforce.15 MM is a reflection of the quality of care given to pregnant women. However, this parameter does not show the frequency of many of the pathologies of women who were close to dying but survived. The undeniable benefits of this knowledge allow us to know what is really happening in the obstetric units, while MM provides us with limited information. Around 1% of pregnant women suffer some sort of event which puts their lives at risk and there is an estimate of 120 events for every direct MM, most of which are related to hypertension and hemorrhage. Severe maternal morbidity is quantifiable and can be the best way of measuring the improvements in health care.15,16
In Mexico, 90% of maternal deaths occur in hospitals or medical units. This is why the hospital MM rate is so high, compared to the general population.17 In Nuevo Leon for this period of time, the average MM rate was 9.9 per 100,000 born alive. When we compare our MM rate of 1.85 per 1,000 births with that from other hospitals, it is below the 2.46 and 2.48% reported by the Hospital Materno Perinatal del Estado de México during 2007 and 200818 and by Peru (11.25 per 1,000 births).19 A common problem in concentration hospitals is the admittance of severe maternal complications, which are referred very tardily. In our MM group we found that 25 patients (67.5%), were referred in a bad condition. The relation is as follows: of the hypertensive disorders, 12 out of the 14 fatal cases (85.7%) were referred to our hospital with brain hemorrhage; the 3 fatal cases resulting from hemorrhage were treated in other hospitals and then sent here; of the 6 fatal cases due to sepsis, 5 (83.3%) were treated in other hospitals and then sent here; of the 13 fatal cases from medical complications, 5 (19.2%) were admitted to our department being very ill.
The pattern of the main obstetric causes of morbidity and mortality has remained unchanged in the last decades; however, the frequency of all the causes have risen. The 5 main causes worldwide are complications of abortion, postpartum hemorrhage, high blood pressure, antepartum hemorrhage and pre-existing medical conditions.20,21 the 407 SOM cases represent 2.03% of total births, i.e., 1 SOM case for every 49 births. Obstetric morbidity and MM have a direct or close relationship. In our review, there were 37 maternal deaths and the 3 main reasons were: Hypertensive disorders (37.8%), medical conditions (35.1%), and sepsis (16.2%). In the same period of time, SOM incidence was as follows: hypertensive disorders (76.1%, hemorrhage 14.2%, and medical conditions 6.3%). There was only one difference in the hemorrhage cases: they occupied the second place in obstetric morbidity, while they appear in 4th place as a cause of maternal death with only 3 cases (table 1).
When we applied the rates to all of the 5 groups of SOM cases, a greater relationship with the severity of the illness comparative with the number of cases (table 4) was seen. Therefore, among hypertensive diseases there was 1 death for every 22 cases (4.5%) with hemorrhage, 1 for every 19.3 cases (5.1%) with medical complications and 1 death for every 2 cases of sepsis (50%); there was also only 1 anesthetic complication which resulted in death (100%). These results were positively correlated with the admittances to NICU: 19.6% from hypertensive disorders, 4.9% hemorrhage, 92.3% medical conditions, and 66.6% sepsis.
The age group with the highest number of SOM were teenagers with almost 35%; 60% were single or in common-law marriage. Eighty-two percent had finished junior high school or higher (table 5). Becoming pregnant at an early age marks the beginning of long-term economic and social responsibilities, as most of these mothers have low income and limited work options, favoring a vicious cycle of poverty. This situation worsens with the inter-generational repetition of teenage pregnancy, increasing the risk of complications.22,23 Being single or living in common-law marriage favors social exclusion and reduces economic expectations as well as medical care for women.24 In our study all of the patients were low income and did not have medical care services.
Obstetric care in 354 reviewed cases was of 3 uterine curettages (0.84%), 38 deliveries (10.73%) and 313 C-sections (88.41%). Historically, performing C-sections is related with obstetric complications or associated with medical conditions.25
Conclusion
Assessment of MM in addition to SOM provides reliable data about the prevalence of severe obstetric complications; thus, this relevant information allows taking specific preventive measures as well as improving medical care and the allocation of resources addressed at caring for women of childbearing-age.26
Conflicts of interest
The authors have no conflicts of interest to declare.
Funding
No financial support was provided.
Received: October 2013;
Accepted: October 2013
* Corresponding author:
Department of Gynecology and Obstetrics,
"Dr. José Eleuterio González" University Hospital.
Madero y Gonzalitos Avenue, Mitras Centro, Monterrey, N. L., México.
E-mail address: joseiglesias2210@gmail.com (J. L. Iglesias-Benavides).