To evaluate the safety and efficacy of labor in patients with a previous uncomplicated cesarean section in the Obstetrics Department at a University Hospital.
Material and methodsWe performed an observational, longitudinal, prospective, descriptive, non-blind, comparative study of patients with a history of previous cesarean sections who attended a tertiary care teaching hospital in northeastern México for the care of their pregnancy from March 2013 to July 2014, where they were monitored during labor. A descriptive statistic, with a p-value significance and a Chi-squared analysis, was applied.
ResultsThree hundred patients attended the hospital, with 119 (39.6%) vaginal deliveries and 181 (60.3%) C-sections. The most common indication of a previous cesarean section was a narrow pelvic outlet in 59 patients (19.6%). There were more vaginal births in patients with cervical dilatation >4cm and previous vaginal births. Fetal weight >3500g, absence of previous vaginal birth, cervical dilatation <3.5cm and gestational age >40 weeks increase the risk of a cesarean section.
ConclusionLabor in women with uncomplicated previous cesarean sections is a useful clinical behavior, allowing an uncomplicated delivery in 39.6% of cases.
Cesarean sections are one of the most significant advances in the care of pregnant patients. However, with time, the higher number of indications of C-sections has caused a significant increase in its incidence worldwide.1
In 1985, the WHO established the highest accepted number of indications of C-sections at 15%, considering a higher number as unjustified.2 In Mexico, estimates suggest that the incidence of C-sections is between 36% and 42%.3 Labor after an uncomplicated C-section is considered to be safe, and one who can turn out successful in between 60% and 80% of cases.4–6 Since 1981, the American College of Obstetrics and Gynecology (ACOG) proposed the promotion of labor in pregnant women who had previously undergone a C-section.7 In 2004, the ACOG proposed the selection and contraindication requirements for a labor trial; these are still current.8 The incidence of complications is estimated to be between 0.05% and 1.09%.9 Labor induction with oxytocin and prostaglandins in women with a previous C-section is controversial due to reports which indicate a greater risk of uterine rupture.10–12 In our hospital, we have, as a rule, the allowance of a labor trial in women with a previous non-complicated C-section, but only when this offsets spontaneously.
Materials and methodsWe performed an observational, longitudinal, prospective, descriptive, non-blind and comparative study of patients with a history of previous cesarean sections who attended a tertiary care teaching hospital in northeastern México for pregnancy care. The following aspects were investigated: the indication of a previous cesarean section, previous deliveries, maternal age, gestational age, fundal height and cervical changes found during their admission. According to the ACOG criteria,8 only patients who were beyond 26 weeks of pregnancy, had a history of a previous cesarean section with at least a year's time from the cesarean section and the moment of pregnancy. Also, with a non-complicated transverse segmental hysterotomy and a physical examination ruling out a narrow pelvis or a cephalopelvic disproportion were selected. The time and evolution of spontaneous labor were analyzed. No labor-inducing medication was utilized. Moreover, different aspects were assessed in newborns, i.e., weight, clinical gestational age using the Capurro method, the Apgar score, and admission to the Neonatal Intensive Care Unit (NICU). A descriptive statistical study was conducted, with a p-value significance and a Chi-squared analysis. Relative risks were analyzed using 2×2 contingency charts, with data comparisons between them.
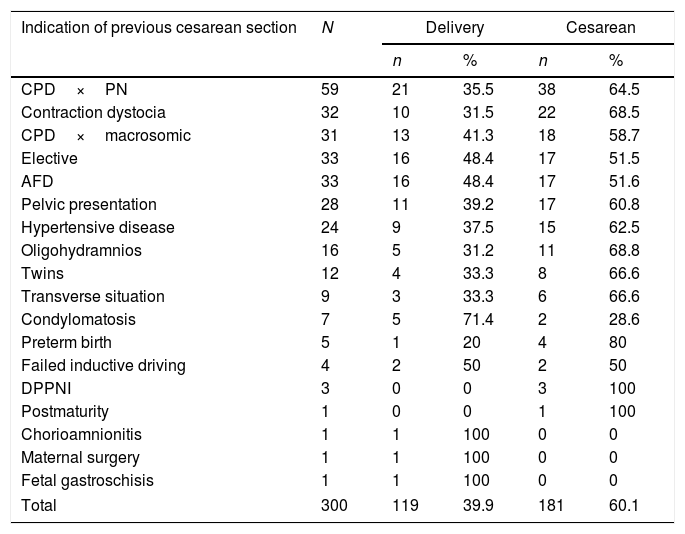
ResultsA total of 300 patients with spontaneous labor and a history of previous cesarean section were included, median maternal age was 25 years (range, 17–42) and median uterine fundal height was 32cm (range, 22–39). One-hundred and nineteen patients (39.6%) had subsequent natural deliveries and 181 (60.3%) cesarean sections. The reasons for the previous cesarean sections are shown in Table 1.
List of indications of previous cesarean sections and obstetric care received in 300 patients undergoing labor. CPD, cephalo-pelvic disproportion; PN, pelvic narrowing; AFD, acute fetal distress; PDPNI, premature detachment of placenta normo-insert.
| Indication of previous cesarean section | N | Delivery | Cesarean | ||
|---|---|---|---|---|---|
| n | % | n | % | ||
| CPD×PN | 59 | 21 | 35.5 | 38 | 64.5 |
| Contraction dystocia | 32 | 10 | 31.5 | 22 | 68.5 |
| CPD×macrosomic | 31 | 13 | 41.3 | 18 | 58.7 |
| Elective | 33 | 16 | 48.4 | 17 | 51.5 |
| AFD | 33 | 16 | 48.4 | 17 | 51.6 |
| Pelvic presentation | 28 | 11 | 39.2 | 17 | 60.8 |
| Hypertensive disease | 24 | 9 | 37.5 | 15 | 62.5 |
| Oligohydramnios | 16 | 5 | 31.2 | 11 | 68.8 |
| Twins | 12 | 4 | 33.3 | 8 | 66.6 |
| Transverse situation | 9 | 3 | 33.3 | 6 | 66.6 |
| Condylomatosis | 7 | 5 | 71.4 | 2 | 28.6 |
| Preterm birth | 5 | 1 | 20 | 4 | 80 |
| Failed inductive driving | 4 | 2 | 50 | 2 | 50 |
| DPPNI | 3 | 0 | 0 | 3 | 100 |
| Postmaturity | 1 | 0 | 0 | 1 | 100 |
| Chorioamnionitis | 1 | 1 | 100 | 0 | 0 |
| Maternal surgery | 1 | 1 | 100 | 0 | 0 |
| Fetal gastroschisis | 1 | 1 | 100 | 0 | 0 |
| Total | 300 | 119 | 39.9 | 181 | 60.1 |
The labor trial was conducted with a duration of more than 4h in 263 (87.6%) patients; for the remaining 37 (12.3%), the trial was suspended between 1 and 2h due to risky obstetric conditions (fetal distress, membrane rupture, and eclampsia). In patients who underwent a delivery, the average time in labor was 6.3h (range, 1–29), forceps were needed in 59 patients (49%) and 66 patients (55%) had a history of delivery prior to the cesarean section (37 completed delivery and 29 ended in a C-section).
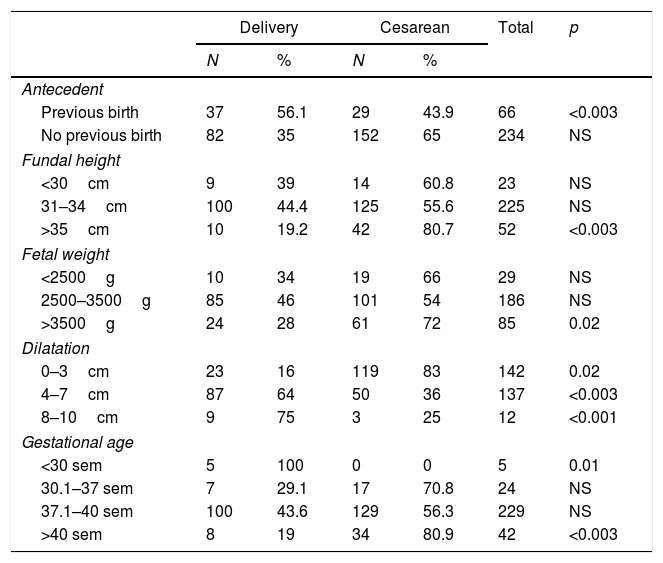
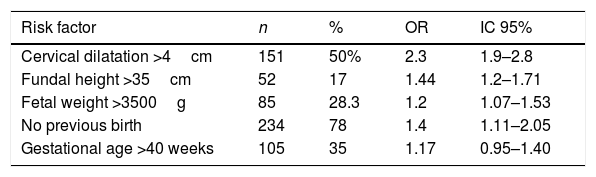
The differences between groups in the studied variables (previous birth, fundal height, fetal weight, dilatation and gestational age) are shown in Table 2, the risk factors for repeat cesareans are established in Table 3.
Relationship of previous antepartum, fundal height, fetal weight, dilation and gestational age with the incidence of delivery and cesareans.
| Delivery | Cesarean | Total | p | |||
|---|---|---|---|---|---|---|
| N | % | N | % | |||
| Antecedent | ||||||
| Previous birth | 37 | 56.1 | 29 | 43.9 | 66 | <0.003 |
| No previous birth | 82 | 35 | 152 | 65 | 234 | NS |
| Fundal height | ||||||
| <30cm | 9 | 39 | 14 | 60.8 | 23 | NS |
| 31–34cm | 100 | 44.4 | 125 | 55.6 | 225 | NS |
| >35cm | 10 | 19.2 | 42 | 80.7 | 52 | <0.003 |
| Fetal weight | ||||||
| <2500g | 10 | 34 | 19 | 66 | 29 | NS |
| 2500–3500g | 85 | 46 | 101 | 54 | 186 | NS |
| >3500g | 24 | 28 | 61 | 72 | 85 | 0.02 |
| Dilatation | ||||||
| 0–3cm | 23 | 16 | 119 | 83 | 142 | 0.02 |
| 4–7cm | 87 | 64 | 50 | 36 | 137 | <0.003 |
| 8–10cm | 9 | 75 | 3 | 25 | 12 | <0.001 |
| Gestational age | ||||||
| <30 sem | 5 | 100 | 0 | 0 | 5 | 0.01 |
| 30.1–37 sem | 7 | 29.1 | 17 | 70.8 | 24 | NS |
| 37.1–40 sem | 100 | 43.6 | 129 | 56.3 | 229 | NS |
| >40 sem | 8 | 19 | 34 | 80.9 | 42 | <0.003 |
Contingency table of risk factors for repeat cesareans in 300 patients with previous non-complicated cesarean sections, submitted to labor.
| Risk factor | n | % | OR | IC 95% |
|---|---|---|---|---|
| Cervical dilatation >4cm | 151 | 50% | 2.3 | 1.9–2.8 |
| Fundal height >35cm | 52 | 17 | 1.44 | 1.2–1.71 |
| Fetal weight >3500g | 85 | 28.3 | 1.2 | 1.07–1.53 |
| No previous birth | 234 | 78 | 1.4 | 1.11–2.05 |
| Gestational age >40 weeks | 105 | 35 | 1.17 | 0.95–1.40 |
Three patients had maternal complication: third-degree perineal tears in two of them and one uterine rupture with obstetric hysterectomy. The median Apgar score at 5min was 8 for both groups. Twelve neonates had complications: perinatal asphyxia caused by the cesarean in 2 of them, one stillbirth, and 9 admissions to the NICU due to prematurity (7 C-sections and 2 deliveries).
DiscussionIn this study, almost 40% of the patients who were attended to resulted in a delivery, which, even though it is favorable, is below the 60–80% estimated by the ACOG and other authors.13,14 When reviewing the indications of previous cesareans, it has come to our attention that in the case of a narrow pelvis, which ought to be an absolute indication to repeat a C-section, a little over a third of these patients resulted in delivery. In the indications of a large fetus and elective C-section, the percentage of delivery was greater (41% and 48%). Our results also match with those reported by other authors, who note that the risks are fewer when the patient went into labor prior to the cesarean, as well as a greater chance of success if the patient had a vaginal delivery before the cesarean.15 In fact, it is accepted that the best predictor for a vaginal delivery in women with a full term pregnancy and a history of non-complicated segmented cesarean is a vaginal delivery prior to the cesarean, with a success rate going anywhere from 84% to 90%.16–19 In our study, when there was spontaneous labor and a cervical dilation greater than 4cm, 80% were deliveries. The contingency table with the clinical variables related to a greater risk of labor failure are: absence of labor, cervical dilation <4cm, fetal weight <3500g, fundal height >35cm and a gestational age >40 weeks. These proved that the risk of failure could be 2–9 times higher depending on the number of variables present20–22 (Table 3). On the complications, the case of uterine rupture was detected after delivery, with a healthy newborn and uterine repair via laparotomy; it represented 0.3% of our cases, in accordance to the range of 0.05% and 0.74% stated in the literature.14,23,24 The two patients with third-degree vaginal tears were related to obstetric conditions (precipitated delivery and the use of forceps), with newborns within normal weight ranges and without complications.25 Perinatal morbidity–mortality observed in the study was related to prematurity and the mother's medical problems, and not to care in the delivery or cesarean.
In conclusion, every hospital ought to analyze its population and the efficacy of labor in patients with a previous non-complicated cesarean. It is not possible to achieve a 60–80% success rate of vaginal delivery in patients with labor and a previous non-complicated cesarean in many hospitals nationwide. It is necessary to perform an evaluation oriented to the characteristics of our patients, and detect those factors which represent a potential warning for a greater risk of complications.
FundingNo financial support was provided.
Conflict of interestThe authors have no conflicts of interest to declare.