To present the laparoscopic splenectomy (LS) experience at the “Dr. José E. González” University Hospital from January 2008 to October 2014.
MethodsRetrospective and descriptive analysis of clinical and surgical aspects of all patients who underwent laparoscopic splenectomy from January 1st 2008 to October 31st 2014 at the “Dr. José Eleuterio González” University Hospital.
ResultsLaparoscopic splenectomies were performed on 14 patients, with a mean age of 20.6 years. Indications for splenectomy included the following diagnosis: idiopathic thrombocytopenic purpura (ITP), 71%; hereditary spherocytosis, 14%; sickle cell anemia and thalassemia, 7%; pyruvate kinase deficient hemolytic anemia, 7%. Mean operative time was 177.5min. Mean intraoperative hemorrhage was 223.5ml. Conversion to laparotomy occurred in one patient (7%) associated with uncontrollable bleeding with splenomegaly. Accessory spleens were identified in 3 patients (21%). Mean spleen weight was 187.5g. Mean postoperative hospital stay was 3.35 days. There was no surgical re-intervention. The 4 trocar right lateral decubitus approach was the preferred method for all patients.
ConclusionsLS can be performed as a safe and effective procedure in benign hematological diseases in our everyday environment.
Among the most important advances in the field of surgery is, without a doubt, the development of minimally invasive techniques. Laparoscopic splenectomy (LS) has proven to be safe and effective in different retrospective series, with a lower postoperative rate and a greater reduction in hospital stay compared to the referred data in historic series of open splenectomies.1
In 1991, Delaitre et al. reported the first successful LS.2 Since then it has become the procedure of choice for spleen removal in patients with hematologic diseases that require surgical treatment.3
Laparoscopic splenectomy is a technically demanding procedure, the knowledge of the distribution of the splenic vascularization is of utmost importance. The challenges are the release of different support elements, vascular pedicle control and the removal of the excised tissue.4
The continuous development of surgical skills and growing technological advances have allowed surgeons to reproduce, through the use of laparoscopy, most open surgical techniques; however, in order for a minimally invasive procedure to have universal acceptance, it must meet some conditions: it must be reproducible, morbidity and mortality rates ought to be comparable or lower, base disease control must be equal or better to the results of the open approach, and it must have additional benefits for patients, such as less postoperative pain, a shorter in-hospital stay, a faster return to everyday activities or better cosmetic results.3
Approach in the surgical technique (supine – anterior – semilateral, lateral) is the choice of the surgeon and based on the concomitant conditions.5 The most utilized technique in most hospitals is the technique described by Targarona.6
The objective of this document is to present an experience with LS in the “Dr. José E. González” University Hospital between January 2008 and October 2014
Materials and methodsThe study was conducted using a retrospective and descriptive analysis of clinical and surgical aspects of all patients who underwent laparoscopic splenectomy between January 2008 and October 2014, at the General Surgery Service of the “Dr. José E. González” University Hospital.
Different variables were inputed in a database including: age, sex, diagnostic, operative data (operative time, blood loss, presence of accessory spleen, spleen weight, conversion, surgical technique) and postoperative data (major and minor postoperative complications, re-interventions and in-hospital stay length).
The inclusion criteria for the study were: all patients who underwent LS at the “Dr. José E. González” University Hospital between January 2008 and October 2014, independently of age range or gender.
The surgical technique utilized in all patients is described below. After the inductions of general anesthesia and endotracheal intubation, the patient is placed in a right lateral decubitus position with a 60° angle. The surgeon remains on the right side of the patient; the camera assistant is to the right of the surgeon and the first assistant on the left of the patient. The pneumoperitoneum is insufflated using the Hasson technique and by maintaining intra-abdominal pressure between 12 and 15mm Hg. Four trocars are placed, (2 of 5mm and the other 2 of 10mm) using 30° optics. The patient is given an orientation in inverted Trendelenburg at 15°, this maneuver allows the spleen to be suspended by its diaphragmatic ligaments, while the force of gravity retracts the stomach, transverse colon and the greater omentum to an inferior position. The abdomen is systematically examined in order to rule out an accessory spleen before starting dissection to avoid darkening of the visual field with cloths. Dissection is performed in 5 stages: division of splenocolic ligament, lower-pole vessel ligation, control of vascular hilum, division of short gastric vessels and detachment of diaphragmatic ligaments. The division of the different splenic ligaments is performed using a harmonic scalpel (Harmonic Shears; Ethicon®, Cincinnati, Ohio) and hilum control through the use of medium–large titanium staples (Titanium clips; Weck Horizon), two proximal and one distal, in the splenic vein and artery. Once the specimen is resected it is placed in an extraction bag previously inserted in the abdominal cavity. The piece is morcellated, and then the small fragments are extracted with the use of banding pliers and an aspirator, avoiding spilling of the content in the cavity. Closed drainage systems were placed in every patient.
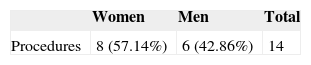
ResultsA total of 14 laparoscopic splenectomies were performed between January 2008 and October 2014. There were 8 women and 6 men, representing 57.14% and 42.86%, respectively, with a mean age of 20.6 years (range 1–65 years) (Table 1).
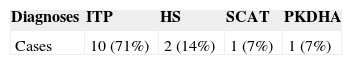
Indications for splenectomy included the following diagnosis: idiopathic thrombocytopenic purpura (ITP), 10 patients, 71%; hereditary spherocytosis, 2 patients, 14%; sickle cell anemia and thalassemia, 1 patient, 7%; pyruvate kinase deficient hemolytic anemia, 1 patient, 7% (Table 2).
Mean operative time was 177.5min (range 110–255min) and mean intraoperative hemorrhage was 223.5ml (range 100–900ml).
A concurrent procedure was performed in one case (7%), represented by cholecystectomy. Accessory spleens were identified in 3 patients (21%). Mean spleen weight was 187.5g. (range 50–900g). Mean postoperative hospital stay was 3.35 days (range 2–16 days). There was no surgical re-intervention. The 4 trocar right lateral decubitus approach was the preferred method for all patients.
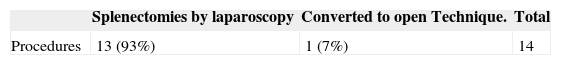
Conversion to laparotomy occurred in one patient (7%) due to uncontrollable bleeding with splenomegaly (900g) (Table 3). The same patient presented as a postoperative complication, a sub-phrenic abscess drained by radio-interventionism using a universal catheter, thus prolonging the patient's hospital stay to 16 days.
DiscussionThe benefits of laparoscopic surgery are undeniable and well-known. In the case of splenectomy, the main observed advantages are the presence of less postoperative pain, immediate reinstatement of the intestinal passage, shorter postoperative in-hospital stay, a quicker return to everyday activities and excellent cosmetic results.7
LS disadvantages include the need to train the surgical team, a requirement of longer surgical time in comparison to conventional surgery and an increment in costs.8
ITP is the most common indication for LS and in combination with hereditary spherocytosis involves 40–100% of the cases in most of the reported series. In ITP, the size of the spleen in characteristically lower, due to splenic infarction, this can facilitate its laparoscopic manipulation as well as its extraction.9 Preoperative information is of particular relevance in order to achieve a better planning for the laparoscopic approach. For experienced surgeons, as well as those with less experience, LS has a higher morbidity and a higher conversion risk when dealing with patients with splenomegaly.10 Targarona et al. found a direct correlation between conversion incidence and the weight of the spleen. The conversion rate was 0% when the spleen weighed between 400 and 1000g, 25% when it weighed more than 1000g and 75% when it weighed more than 3000.11 However, Owera et al. established that despite higher surgical times, LS recovery time is shorter and less torpid.12
Due to the high volumes and pressures involved in spleens, in addition to splenomegaly and the vascular congestion that is usually present in these illnesses, on top of the fragility of the splenic capsule, a hemorrhage at this level is hard to control in some situations in open technique as well as in laparoscopy, hence when presented with bleeding during a procedure which could potentially set back hemorrhage control and compromise the patient's hemodynamic state we opted for the conversion to open technique, given the fact that there is more experience and skill with this technique.
Incidence of accessory spleen detection is somewhere between 4% and 27% of the cases during open splenectomy in patients with ITP,13 while different LS series refer to incidences between 11% and 21%.14 In our series we detected accessory spleens in 21% of the patients, usually located in relation to the splenic hilum or adjacent to the pancreatic tail. However, they may be found throughout the splenic vessels’ route, in the gastro-splenic or splenic-renal ligaments, inside the pancreatic tail, on the wall of the intestine or colon, in the greater omentum or the mesentery, and even in the pelvis or scrotum. The detection and characterization of accessory spleens are important due to 3 problems. First, the accessory spleens may be symptomatic, presenting torsion, spontaneous rupture, hemorrhage or cystic formation. Second, it is necessary to detect them when dealing with patients with hematologic diseases which require splenectomy and which could remain sub-treated if the functional splenic tissue is not removed in full. Finally, accessory spleens can be confused with lymphatic adenopathy or tumors of other organs. Usual accessory spleen diagnosis is performed using a tomography, finding an image with precise margins, in general smaller than 3cm, and capturing a homogenous shape with a similar density to the main spleen in its phases with and without contrast. In cases where there is a diagnostic doubt and there is a suspicion of an accessory spleen, the use of centelleographic studies with elements which are taken by the splenic tissue is prescribed. Among these studies a few stand out, like centelleograms with 111 in-labeled platelets, technetium Tc-99m Sulfur Colloid, and heat-denatured red blood cells labeled with technetium-99m (Tc-99m DRBC), the latter being the most specific because it presents a reduced capture by the liver, resulting in a better contrast of white tissue.
In the cases of our study, we were not counting on a diagnostic suspicion because of previous image studies and accessory spleen identification as a result of rigorous surgical examination in the operative field as well as the route of the fixing elements of the spleen. The methodology was performed through the inspection and dissection of the spleen's peripheral structures using laparoscopic instruments.15,16
The frequency of conversion in the literature ranges from 3% to 8%1, which corresponds with the data shown by our study, and most conversions occur as a consequence of bleeding or difficulty in the dissection, especially in patients with a large splenomegaly.
The reported learning curve in the literature for this surgery is 20 procedures, as a standard to accomplish better results and benefits from this surgery.17 This technique is imperative to be taken into account as a part of every general surgeon's training, even when the vast majority of prescriptions represent hematologic diseases. Our objective was not to evaluate the response of these diseases to surgical treatment but to prove the safety and efficacy of the approach.
ConclusionsLS can be considered as a safe and effective procedure in benign hematological diseases and can be regularly used in our environment. It provides the advantages of minimally invasive surgery with a lower morbidity and mortality compared with open surgery, placing it as the first choice for hematologic diseases which require a surgical approach.
Conflict of interestThe authors have no conflicts of interest to declare.
FundingNo financial support was provided.