Introduction: Hospital malnutrition risk has prevalence values of 20%-50%, and it is a major health problem in the health institutions worldwide.
Objective: To assess the accomplishment of nutritional screening and the prevalence of hospital malnutrition risk in a University Hospital.
Materials and methods: A retrospective analysis was carried out with nutritional screening, using primary data from six clinical areas obtained in the period between July 2012 and December 2013. According to previous results in Mexican health institutions and considering a mean malnutrition risk prevalence of 50%, it was calculated that a sample size of 3200 subjects was required for the assessment of valid risk values. Patients with values ≥3 on the Nutritional Risk Screening (NRS, 2002) were classified as carriers of nutritional risk.
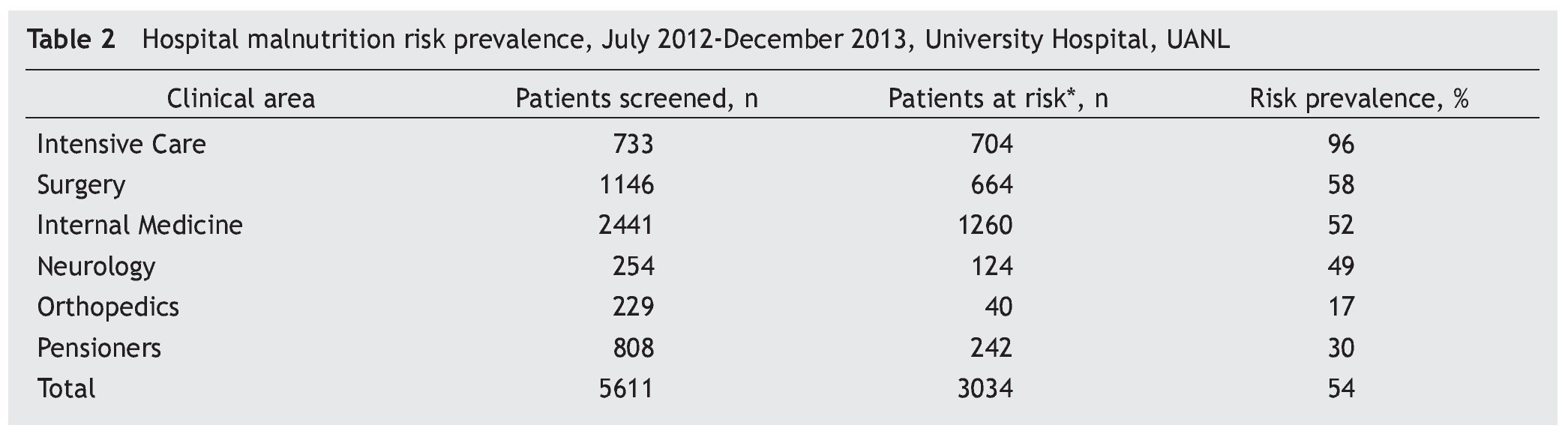
Results: A total of 5611 patients (38% of all patients admitted) were studied. The rate of screening declined from 55% in 2012 to 31% in 2013. During the whole period, 3034 patients were classified with risk of malnutrition (54% prevalence).
Conclusions: The prevalence of hospital malnutrition risk was high. The accomplishment of the nutritional screening was deficient, and declined between 2012 and 2013. The lack of nutritional screening does not meet the vital care requirements of hospitalized patients and prevents the timely treatment of those at malnutrition risk.
Introduction
Malnutrition is a major public health problem which affects the entire world, not only less favored economies, but developed countries as well.1
Patients admitted to a hospital are a group especially vulnerable to malnutrition, with a high prevalence, around 20-50%, depending on the diagnostic criteria.2-11 The Latin American Federation of Nutritional Therapy, Clinical Nutrition and Metabolism (FELANPE for its Spanish acronym) hosted the first Latin American Study of Hospital Malnutrition in the biennial 1999-2001, which found a malnutrition frequency of 51.2%.12 In Mexico there are few studies on the subject; however, the existing conducted studies suggest a severe situation to take into account by the health system.13-15
Hospital malnutrition is defined as malnutrition which affects hospitalized patients as a result of a complex interaction between illnesses, food and nutrition.1,16 It is a distinct entity whose term was coined in the 70s, as a result of the studies by Bistrian, where he made evident the high prevalence of this condition in hospitalized patients.17
In 1974 Butterworth used the term “iatrogenic malnutrition” to describe body composition disorders of hospital patients caused by the actions or omissions of the medical team, and documented some practices which contributed to the patients’ nutritional deterioration, like omission of responsibilities in nutritional care, prolonged use of intravenous nutrition, deficiency in the monitoring or register of dietary intake and inexistence of proper nutritional support.18,19
The etiology of hospital malnutrition is multifactorial and includes causes related to the disease itself: intake reduction, response to aggression, mechanical obstruction of the gastrointestinal tract, pharmaceutics, advanced age, an increase in requirements, an increase of its losses, and inflammatory conditions; causes related to hospitalization: a change in habits, reactive emotional situations, complementary examinations, surgical treatments, pharmaceutics, chemotherapy-radiotherapy, hospitality; causes related to the medical team: misuse of therapeutic fasts, lack of nutritional assessment, lack of intake control, dilution of responsibilities; causes related to health authorities: lack of nutritionists, absence of nutrition units, lack of dietician-nutritionist acknowledgement, and lack of a coordinated and multidisciplinary work.1,17,20
Hospital malnutrition usually enters a vicious cycle, despite the fact that the patient has increased requirements, they tend to not be met, causing depletion and exhaustion of energy and nutrimental reserves and thus increasing his/ her consumption needs. There are reports confirming that hospitalized patients, in general, do not consume the necessary amount of energy and nutriments to cover their requirements, which worsens their nutritional condition.21-23
Once established, malnutrition sensibly affects the organisms’ response capabilities to medical-surgical treatment, impedes proper healing and increases the risk of suture dehiscence and sore outbreaks, placing the patient in a situation of immunosuppression which makes him/her susceptible to opportunistic infections. If not treated in a timely manner, malnutrition may lead to the patient’s death.9,24-28
For over 25 years it has been known that malnutrition is one of the main and more frequent causes of mortality in hospitalized individuals. Early work dates back to 1936, when Studdley reported that weight losses over 20% of the total weight increase mortality rate in hospitalized patients by 10 times.29 According to Howard, “each and every patient who is admitted to a hospital has the right to expect his/her nutritional requirements to be provided.”30 but in reality how many patients receive proper nutrition in clinics and hospitals? Probably, the answer to that question is shown in different statistics in Europe, US, or in the IBRANUTI study, where numbers show that close to 50% of hospitalized patients have some type of malnutrition.4
Nutritional screening and a proper nutrition are part of the rights of every patient who is admitted to a hospital, thus making it essential for these requirements to be met. Without a doubt, analysis of the ethical aspects in clinical practice contributes to the improvement in healthcare quality.31-33
In order to reduce hospital malnutrition, the development of formal and coordinated intervention is imposed, with specific objectives which include the implementation of recognized methods of nutritional screening which allows us to program a timely and proper nutritional plan for at-risk patients.34-36
In 2003 the Resolution on Food and Nutritional Care in Hospitals was published by the Council of Europe’s Committee of Ministers, who took on the political commitment of the 18 signing countries. This resolution includes elements of obliged consideration on nutritional assessment, the identification and prevention of causes of malnutrition, nutritional counseling, conventional diets and artificial diets. Moreover, this resolution highlights the proper distribution of responsibilities among healthcare authorities, hospital and clinical management. Even though the resolution lacks an obligatory compliance rule, it functions as a starting point of reflection in many hospitals, thus motivating them to raise the need for implementing nutritional screening and acting protocol methods.37 Nevertheless, it is still far from its generalization, as shown in a survey conducted in 75 Spanish hospitals (half of them without a clinical nutrition unit in the organization chart), where only 15% had systemic nutritional screening on admission.38
In many countries, hospitals must provide a nutritional screening in order to go through a quality certification process, as with hospitals in the US (Joint Commission’s accreditation requirement JCAHO).39 In Mexico it is a requirement as well (General Health Council standards AOP.1.6 and AOP.1.7, Establishment Certification Commission for Medical Attention, National Certification System of Medical Attention Establishments, Certification Standards for Hospitals, Version 2011, active since January 2011).
The “Dr. José E. González” University Hospital of the UANL is the only one with third-level care in the northwest of Mexico for a population without medical or social security coverage, with a mid-low or low socioeconomic level. Today there are 500 beds, 22 departments and 20 clinical services, of which 17 and 18 respectively have a close relationship with food and nutrition.
One of their duties is to guarantee the patient’s safety and to keep the hospital certification processes up-to-date, thus making it necessary to establish a nutritional screening as an indispensable step in the medical care of every admitted patient.
For this purpose, the development and implementation of nutritional screening began in several clinical areas of the hospital since early 2012, as a pilot program. After almost two years of implementation of screening and data collection, a diagnosis of the process needed to be conducted.
Some of the objectives of this investigation were to evaluate the level of execution of the screening in clinical areas and establish the prevalence of hospital malnutrition risk.
Materials and methods
A retrospective analysis was carried out with nutritional screening primary data from six clinical areas: adult and postsurgical intensive care unit (ICU), surgery, internal medicine, neurology, orthopedics and pensioners. Primary data, monitored by the nutrition clinic, was obtained in the period between July 2012 and December 2013.
Nutritional Risk Screening (NRS 2002) was the method used to obtain the nutritional screening.40 This method includes a nutritional assessment aimed at detecting malnutrition risk (weight loss, body mass index and lowered intake), as well as an assessment of the severity of the disease and the increase of the nutritional requirements which it may condition. Age is considered an additional risk factor if the patient is more than 70 years old. The NRS indicates the need for a deeper nutritional assessment if the global score is ≥3.
The NRS screening method is recommended by the European Society of Parenteral and Enteral Nutrition (ESPEN) to apply to hospitalized patients, it is applicable to most patients, fast and easy to complete. The most subjective data is the assessment of the severity of the disease, which can influence the final result. However, the variability among observers is small when applied by trained personnel (nurses, doctors, nutritionists). This method was developed by the ESPEN in 2002 and was designed from a retrospective analysis of 128 controlled clinical trials focused on nutritional assessment, nutrition support and patient evolution; it is validated to detect those patients who present malnutrition risk, but does not categorize it.1
In order to consider the prevalence of malnutrition risk as valid, the sample size was calculated from a supposed mean malnutrition risk of 50%, according to the data obtained in other studies conducted in different health institutions in Mexico.14,15 A required sample of 3200 patients was estimated to detect an absolute difference of the prevalence with a potency of 80% (β=.20) and a confidence level of 95% (Software SampleSize, EpiInfo 7.1.2.0).
The data of the number of admitted patients were obtained directly from the respective departments. Screening adherence percentages are expressed as an average of the 6 months evaluated in the year 2012 and all 12 months of 2013, as a total and by clinical area where the screening was being implemented.
For the prevalence of malnutrition risk calculation the following data were used: the number of patients who obtained a score >3 during the survey and the number of patients who were screened.
The nutritional screening form was filled out directly by the nutrition clinic personnel during 2012. However, in 2013 it became part of the residents’ responsibilities, as a part of the patient’s medical history.
Primary data collected, after cleaning and cross checking, was stored in a digital container created with Microsoft Office Excel. The variables of interest were reduced to location statisticians (average) and aggregation (percentages) using SPSS 11.0 (SPSS Inc.; Pennsylvania, United States). The protocol of this study was approved by the ethics committee of the hospital, MI14-003.
Results
A total of 5611 patients were screened, 38% of the patients admitted between July 2012 and December 2013 in all six clinical areas being evaluated. In 2012 screening accomplishment was 55%; the clinical area with the highest rate of screening was the ICU (75%) and the lowest orthopedics (35%). During 2012 screening decreased considerably, with an accomplishment rate of 31%; the clinical area with the highest rate of screening was the ICU (63%) and the lowest was orthopedics (11%).
Very low screening execution percentages during 2013 compared with 2012 were found in two clinical areas: surgery and orthopedics (table 1).
Average prevalence of hospital malnutrition risk was 54%, with the highest prevalence in the ICU (96%) and the lowest in orthopedics (17%). An elevated prevalence was observed in surgical areas (58%), internal medicine (52%) and neurology (49%) (table 2).
Discussion
Nutritional screening accomplishment was low in 2012 as well as 2013, considering it should be practiced in 100% of admitted patients, and during the first 24 h of admission. In 2012 the screening accomplishment was higher, because it was performed directly by the personnel of the nutrition clinic, whilst in 2013 this activity was assumed by the residents of the different clinical areas, which was linked to a reduction of 17% in its execution. One of the possible associated factors with this low accomplishment was the fact that this action was not a part of the routine practices of the hospital and there wasn’t an awareness of its necessity.
It is known that basic work teams fail at recognizing the presence of nutritional disorders or malnutrition risk in the patient. The reasons can be multiple and overlap in their influence; it is also possible that the different nutritional needs that may be present are difficult to recognize in everyday clinical practice, especially in adult patient care.
In general, the possible objective and subjective causes, which may have affected the nutritional screening accomplishment, were: absence of specific form in clinical history, form’s lack of completion or improper completion, lack of a normalized procedure of operation which rules all activities related to nutritional screening, lack of proper training, lack of a multidisciplinary concept in nutritional care, a possible responsibility dilution and the possible lack of conviction by the doctor of the importance of food-nutrition in normal and pathological states.
Nutritional education has been forgotten in medical curricular formation in a large number of countries, or it is taught in a very superficial manner.41 However, the doctor must be trained to properly assess each patient’s nutritional risk and thus be able to request the required nutritional support in a timely manner.
This principle can be initially satisfied with the proper execution of nutritional screening as an essential part of the clinical history and should be performed by the doctor. Even though the whole screening process, as well as its control, must be responsibility of the nutrition clinic.
Prevalence of malnutrition risk in hospital areas where nutritional screening is performed can be considered high, if compared to the rates reported in medical literature.2-15 This fact demands urgent and strong actions from the hospital’s health policies.
There are studies that show the nutritional state deteriorating during hospitalization if there isn’t proper food, nutritional and metabolic support.21 On the other hand, the moment of assessment of the nutritional state is also an important factor linked to malnutrition risk and presence. Several studies prove the need to perform nutritional evaluations as soon as possible in hospitalized patients, because they evidence a higher malnutrition risk when they are evaluated during hospitalization in comparison to the patients who are evaluated at the moment of hospital admission.27,42
Hospital malnutrition not only alters treatment efficacy, it also increases risk of complications and morbi-mortality, prolongs hospital stay and increases premature re-admission rates, which all affects healthcare costs negatively.43-52
Healthcare costs linked to hospital malnutrition have been recently calculated by the European Society of Parenteral and Enteral Nutrition at 170 billion euros a year.38 Mal-nourished patients have a higher possibility of needing successive hospital admissions, which may be 30-70% higher than that of well-nourished patients. Moreover, it is well-known that nutritional intervention improves the patient’s prognosis in numerous diseases. The associated expense to nutritional support was estimated to be less than 3% of the total expense generated by malnutrition; hence savings as a result of timely nutritional intervention are considerable, especially from the reduction of hospital stay and the lower need of extended-care facilities.38 Given the findings of the present study, the development of standard operating procedures to organize nutritional screening processes in the hospital, with the corresponding formats validated for different groups of patients (children and teenagers, adults, elderly and babies); to provide nutritional screening coverage of all clinical areas of the hospital and to all the patients who are admitted, within the first 24 h, in addition to the completion of the clinical history; development of training courses aimed at the healthcare personnel responsible for its execution (doctors, residents, nurses); the development of a monitoring plan for nutritional screening and follow-up actions, including a deep evaluation of the nutritional state of every patient detected to be at-risk of malnutrition, all this in a multidisciplinary work context, should be an important priority.
Acknowledgements
We give special thanks to the management staff of the “Dr. José Eleuterio González” University Hospital of the School of Medicine of the UANL for their contribution to the development and implementation on nutritional screening.
Financing
The authors declare that they did not receive any sponsorship to conduct this study.
Conflict of interests
The authors declare not to have any conflict of interests.
Received: July 2014;
Accepted: September 2014
*Corresponding author:
Consulta No. 2, Clínica de Nutrición,
Hospital Universitario “Dr. José Eleuterio González”,
Facultad de Medicina,
Universidad Autónoma Nuevo León (UANL),
Ave. Madero y Gonzalitos s/n, Colonia Mitras Centro,
CP 64460, Monterrey, Nuevo León,
México. E-mail address:patyaner@hotmail.com (P.R. Áncer Rodríguez).