A 31-year-old man was referred to our service because of recurrent hemospermia over the last 4 years, there were no other symptoms like perineal pain, fever, dysuria, nocturia or urgency; this patient only presented hemospermia with clots. Genital examination was normal. Semen analysis showed no change in volume and pH; however, hemospermia and asthenozoospermia were observed. The semen culture was normal. Ultrasonography only revealed the presence of a cystic lesion adjoining the prostate gland, next to the bladder neck. The retrograde urethrogram was normal. The CT scan revealed only a small calcification in the right seminal vesicle. Endoscopic cistourethroscopy demonstrated 2 cystic dilatations arising on both sides of the prostate gland adjacent to the bladder neck, behind the verumontanum with vessels running over the surface prostatic cyst dilatation. The diagnosis of prostatic gland cystic dilatation was reached and confirmed by pathology that reported fibroconnective tissue with fibrosis and hyalinization. Transurethral unroofing of the cyst was performed separately with a successful outcome.
Prostatic cysts, although an infrequent diagnosis in men, are usually asymptomatic and mostly detected incidentally during abdominal or transrectal ultrasonography. Etiological factors include chronic prostatitis as a cause of lateral prostatic cysts and congenital disease as a cause of midline cysts. Existent scientific publications on prostatic cysts are mostly isolated case reports, which highlights their uncommon occurrence and even lower propensity for causing symptoms.1 We report a case of a benign prostatic cyst with hemospermia.
Case reportA young 31-year-old male was presented to us with hemospermia with a duration of more than 4 years. Consecutive hemospermia was present in each ejaculation with abundant blood clots. There were no others symptoms like perineal pain, fever, dysuria, nocturia or urgency. No urinary tract infection or prostatic infection was reported.
Initial evaluation included a urine microscopic analysis, semen culture, and a screening abdominal ultrasonography, which documented the presence of a prostatic cyst. A CT scan was performed to evaluate the seminal vesicles and a small calcification was found in the right seminal vesicle (not shown). His sperm count was 36×106 sperm per milliliter (normal 15×106) with 109×106 sperm in the total count (normal 39×106), the progressive motility was 55% (normal 32%), white blood cells was 1×106 (normal 1×106) and red blood cells were abundant (normal 0×106). After the surgery, the semen analysis parameters were sperm count 33×106 sperm per milliliter, with 99×106 sperm in the total count, the progressive motility was 54%, white blood cells was 1×106, and red blood cells 0×106. The patient was initially managed with antibiotic therapy. A retrograde urethrogram did not reveal any communication with the prostatic cyst.
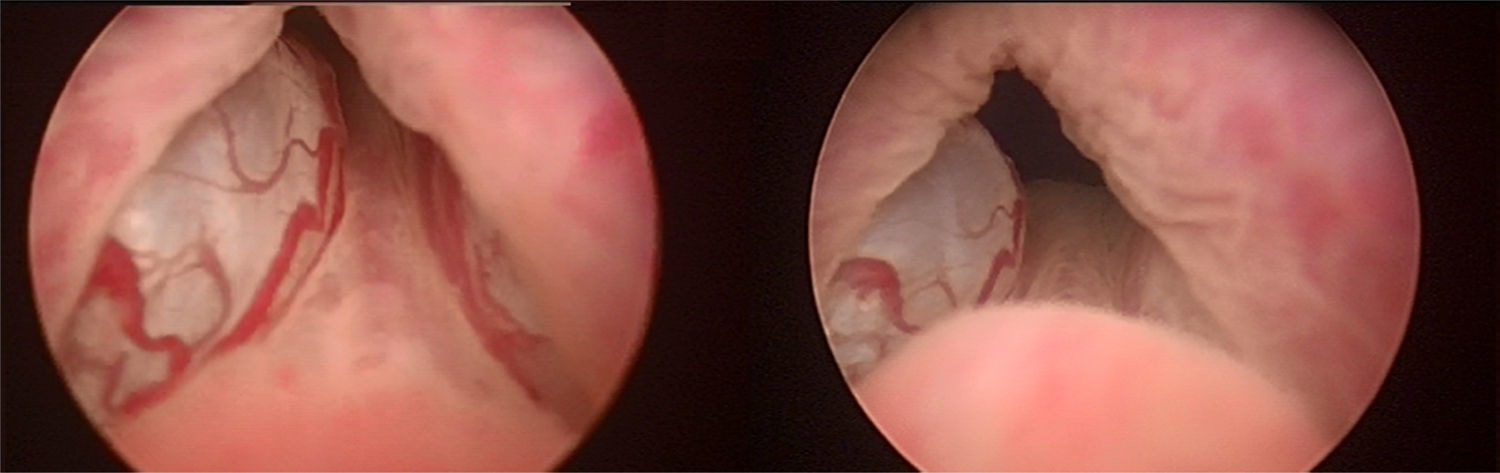
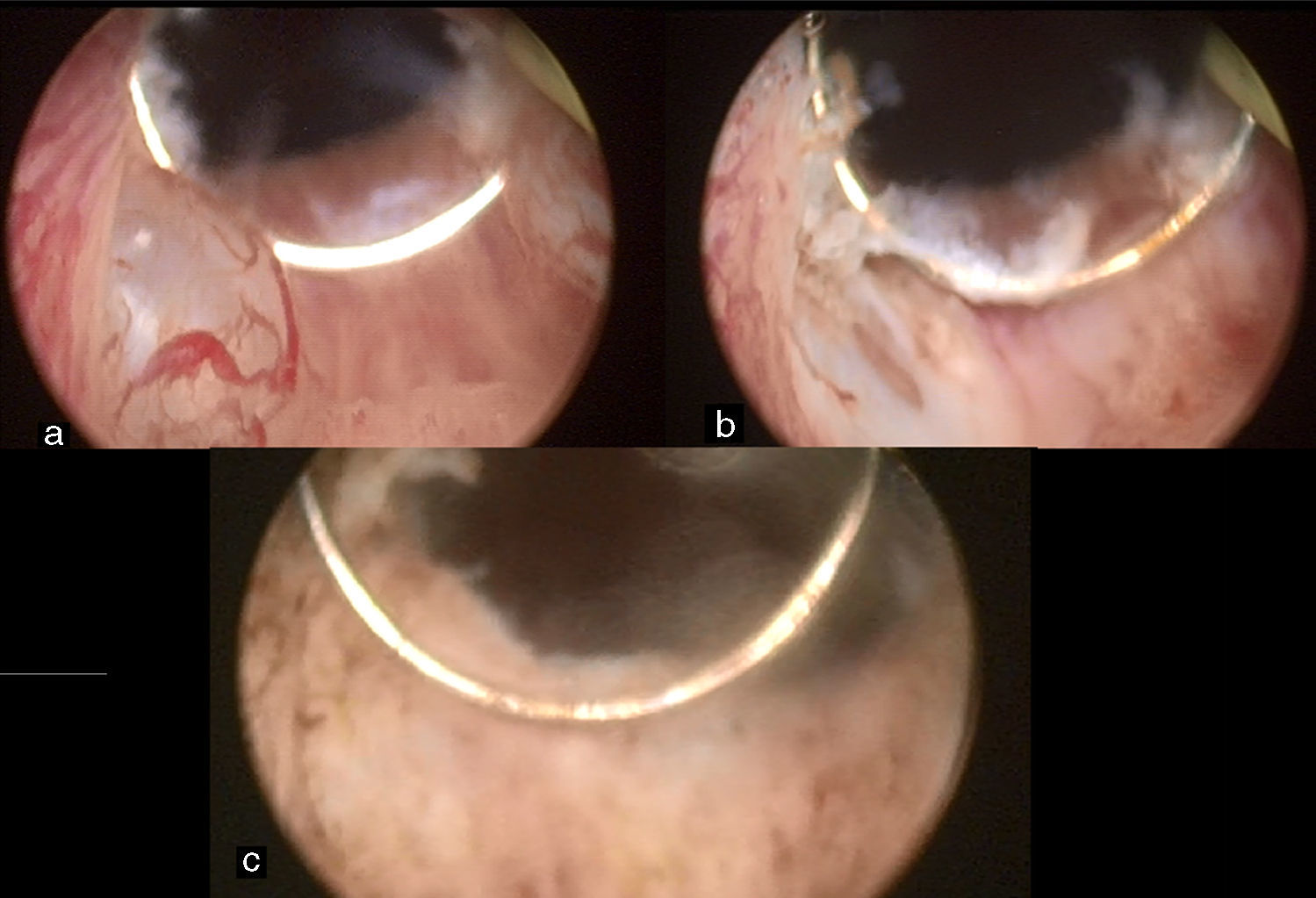
The patient underwent cystoscopy and transurethral resection of the prostatic cyst (Fig. 1). Back pressure changes were noted in this case. The roof of the cyst was resected with minimal coagulation under direct vision with a wire loop to marsupialize the cyst. Care was taken to spare the bladder neck and verumontanum to prevent retrograde ejaculation (Fig. 2). The resection resulted in drainage of a clear fluid. Cold-cup biopsies taken from the cyst wall revealed non-urothelial epithelium with no preneoplastic changes. A 16F Foley catheter was placed overnight and the patient was discharged the next morning. Follow-up at one, three and six months demonstrated unobstructed urinary flow and normal ejaculation.
DiscussionProstatic cysts include the utricle cyst, the Müllerian duct cyst, the hemorrhagic prostatic cyst, the hydatid cyst, and cysts associated with prostatitis. Our patient had a lateral cyst near the bladder neck in the right side and another small cyst in the left side. He was concerned about his hemospermia, because there was more than before in each event and this was the reason he came to the hospital. The patient never referred to pelvic pain, dysuria or perineal pain; his only symptom was hemospermia. He had no infertility problem (he had 2 children, aged 6 and 4). After the surgery and to date, he has never presented hemospermia again, and his sperm count parameters are normal. Some cysts are primarily prostatic glandular in origin and are acquired later in life. Most lateral prostatic cysts are related to chronic prostatitis.2,3 Symptomatic prostatic cysts are a cause of chronic pelvic pain, upper or lower urinary tract infection (UTI), infertility, hemospermia and, rarely, malignancy.4–6 In our case the only symptom was hemospermia, no infertility and no pelvic or perineal pain were present.
Some therapeutic options for managing prostatic cysts include transrectal aspiration with or without sclerotherapy, transurethral marsupialization, and open surgery. Some authors report durable recurrence-free results in a series of patients with medial prostatic cysts treated with transurethral incision.4,7 We treated this patient by means of a transurethral marsupialization and fulguration of the vessels. This lead to full recuperation, and the patient was discharged the next day without pain and he had an uneventful recovery.
Valuable information was obtained by performing a cistourethroscopy, demonstrating that the vessels ran over the cyst, which is by itself an unusual finding. This was important because hemospermia is usually treated only with antibiotics. In our case, the solution was marsupialization of the cyst and fulguration of the dilated vessels.
Conflicts of interestThe authors have no conflicts of interest to declare.
FundingNo financial support was provided.