Use and evaluate the US-TAP BLOCK (Ultrasound Transverse Abdominis Plane Block) for the management of postoperative pain in patients submitted to ambulatory laparoscopic cholecystectomy at the General Surgery service of the “Dr. José E. González” University Hospital.
Materials and methodsClinical trial, experimental, transversal, comparative, prospective, blind study with 24 patients. 12 patients in the “control” group, where pain was managed with intravenous administration of ketorolac 30mg, and 12 patients in the “cases” group using US-TAP BLOCK with bupivacaine 0.5% for pain control. We evaluated the pain level using the Visual Analog Scale (VAS) at 1/2/4/6h postoperatively. Whenever the patients presented severe pain (VAS >6), tramadol 50mg was administered intravenously as a rescue drug.
ResultsGallbladder disease was more frequent in the female gender (87.5%), between 40–49 years old (37.5%), the majority were overweight (54.1%). The predominant histopathological diagnosis was cholecystolithiasis (38%). We observed no difference between the levels of postoperative pain in the compared groups. The use of rescue drugs was lower in the case group (p=0.035).
ConclusionsThe US-TAP BLOCK is an effective analgesic technique, comparable to the standard for pain management used at our hospital, and decreases the use of rescue analgesics.
Benign biliary pathologies are a topic of interest for the medical community, since they are frequently diagnosed in health institutions. Cholelithiasis and cholecystitis are the ones with the highest incidence. Over a million cases are diagnosed annually, mainly affecting the adult population, and more predominantly in females.
In Mexico, cholelithiasis prevalence is 8.5% in men and 20.5% in women.1 This has required the development of surgical techniques and analgesia which allow better medical attention and patient recovery. At the “Dr. José E. González” University Hospital, the surgical technique of choice is ambulatory laparoscopic cholecystectomy, which is currently accepted worldwide as the first choice of approach for gallbladder removal,2 which is similar to what medical literature reports, reducing surgical time3 and providing a lesser sensation of pain for the patient. An ideal postsurgical management of pain requires a multimodal and multidisciplinary approach with a combination of therapeutic maneuvers acting at multiple levels of the nervous system that interfere with the different mechanisms of perception and pain propagation.4 Current pain management of patients who require this procedure as treatment for their medical condition at the General Surgery service of this health institution consists of the administration of non-steroidal anti-inflamatory drugs (NSAIDs) intravenously, such as ketorolac at 30mg, and/or opioids like tramadol at 50mg, when the pain is severe.
Local or regional anesthesia plays a major role in postsurgical pain management. Techniques have been described and performed which can be considered an alternative in pain management, such as the TAP-BLOCK (Transverse Abdominis Plane block), which consists of identifying a neurovascular plane in the anterolateral abdominal muscles and injecting a local anesthetic.5 It is considered to be a relatively new technique, which was described in 2001 by A. N. Rafi,6 who qualified it as a novel focus in the field of abdominal blockage, allowing control of pain. It is performed through the anatomical region dubbed the “Petit's triangle”, the anesthetic drugs are deposited in-between the internal oblique muscle and the abdominal transverse muscle, blocking the T7–12 intercostal nerves, the iliohypogastric and ilioinguinal nerves and the cutaneous branches of the L1–L3 dorsal branch.7
The most commonly prescribed local anesthetic is bupivacaine,8 which belongs to the long-term amino-amida family, provides a superior pain control than opioids and is used commonly in postoperative periods for infiltrative, regional and neuraxial blockade.4
Because the TAP-BLOCK is a blind technique, it can cause inappropriate blockades. However, the introduction of ultrasound has allowed the block to be made with great precision,9 and creating the US-TAP BLOCK (UltraSound guided Transverse Abdominis Plane block), which has minimized errors in the blockade, due to the real-time visualization of the abdominal planes. Previous studies have reported the use of the US-TAP BLOCK technique in patients submitted for a laparoscopic cholecystectomy, using groups at different concentrations of levobupivacaine (B0.25 and B0.5) as an analgesic, and showing a decrease of pain which was evaluated with a visual scale at 20/30/60min and 6/12/24h after the surgery in groups treated with the US-TAP BLOCK and those who did not undergo the prodedure.10
Due to the fact that the postoperative pain which results from laparoscopic procedures in the abdominal plane is moderate to severe, and that at the “Dr. José E. González” University Hospital there is no precedent for the use of alternatives for postoperative pain control, our study's objective was to use the US-TAP BLOCK as an alternative technique to analgesia in patients submitted for a laparoscopic cholecystectomy and compare it against the use of conventional analgesics. It is a quick and simple technique which can be performed on patients of an advanced age. These characteristics make it applicable to the clinic and the population of our hospital would benefit in its entirety.
Materials and methodsThis was a clinical, transversal, comparative, prospective, and blind study, carried out in the Ambulatory Surgery area of the Department of General Surgery of the “Dr. José E. González” University Hospital of the School of Medicine of the Autonomous University of Nuevo León (or UANL, by its Spanish acronym). The study was reviewed and approved by the institution's Ethics Committee. During the period of January–February of 2015, we recruited volunteer patients over 18 years of age, male or female, who were not pregnant, diagnosed with cholelithiasis or cholecystitis, with a previous signed consent form, who required a laparoscopic cholecystectomy as treatment. We excluded patients with alterations in their blood coagulation, patients who were allergic to local anesthetics (bupivacaine) and patients with dermal injuries in the blockade zone.
Patient participation consisted of selecting a closed and sealed envelope in the presence of a witness and the doctor on duty, which could either contain the word “control”, which made reference to postoperative pain management via intravenous ketorolac at 30mgs, or “cases” which made reference to the sole application of a US-TAP BLOCK, injecting bupivacaine as a local anesthetic for pain control. Each group had 12 patients, and each patient counted on the security that whichever procedure they selected was intended to control postoperative pain. Only the surgeon was aware of the procedure to which each envelope referred to.
With the “cases” group, the US-TAP BLOCK technique was applied under general anesthesia immediately after the surgery. The external oblique muscle and the abdominal transversal muscle were located using Philips HD3 ultrasounds equipment (Philips, Canada), allowing the introduction of a 21G, 100mm needle (Stimuplex® A, B.Braun, Germany) into the plane at the level of the anterior axillary line, following its course until it was placed between the internal oblique and abdominal transverse muscles, where the anesthetic (bupivacaine) was deposited at a concentration of 0.5%, at a dosage of 2mg/kg, maximal dose of 175mg, equivalent to 35ml (17.5ml on each side), followed by a bolus of 0.5ccs of saline solution at 0.9%.
Both groups were evaluated at 1, 2, 4 and 6h to follow their postoperative evolution, and their degree of pain was evaluated with the Visual Analog Scale (VAS), where 0 means no pain, 1–3 means light pain, 4–6 means moderate pain and 7–10 is severe pain.
Tramadol at a 50mg dosis was administered intravenously as a rescue drug to patients who, during their postoperative evaluation, presented severe pain (VAS±7).
Clinical data of the patients, and the data obtained with the VAS, were introduced into a database with Excel for Windows 7 Home Premium and statistically analyzed with the SPSS v. 20.0 statistics program, a descriptive analysis was used with the quantitative variables and the qualitative variables were expressed as proportions.
We compared the data on the level of pain between the groups using the student's t-test. The need to apply rescue analgesics during the observation period was compared using x2 and p<0.05 was determined to signify a statistically significant difference.
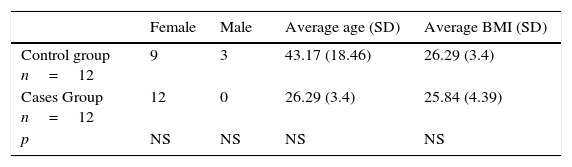
ResultsThe total population studied was 24 patients. The socio-demographic parameters analyzed were gender, age, height, weight and body mass index. 87.5% of the patients were female with an age between 40 and 49 years and overweight, with a body mass index (BMI) greater than 25. The results by group are reported in Table 1.
The average time spent in surgery was 60min for the control group and 70min for the cases group. No patient required the use of drainage and there were no mishaps or complications during the procedures (surgery and treatment). The histopathological diagnosis of the surgical pieces reported that 38% were cases of cholecystolithiasis, 33% chronic cholecystitis and lithiasis, 17% chronic cholecystitis with cholesterolosis and lithiasis, 8% chronic cholecystitis and 4% chronic cholecystitis aggravated by cholesterolosis and lithiasis.
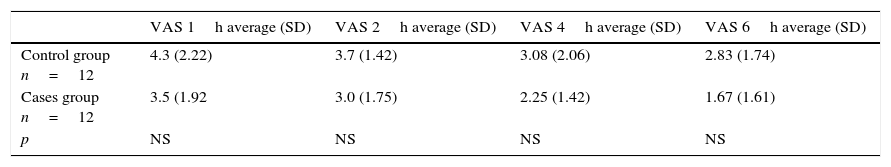
Using Pearson's Chi-squared test, we did not find a statistically significant difference when comparing the values of the VAS taken at 1/2/4/6h postoperatively between the patients participating in the control group and those in the cases group, finding values of p>0.05 (Table 2).
Results of pain evaluated by the Visual Analog Scale.
| VAS 1h average (SD) | VAS 2h average (SD) | VAS 4h average (SD) | VAS 6h average (SD) | |
|---|---|---|---|---|
| Control group n=12 | 4.3 (2.22) | 3.7 (1.42) | 3.08 (2.06) | 2.83 (1.74) |
| Cases group n=12 | 3.5 (1.92 | 3.0 (1.75) | 2.25 (1.42) | 1.67 (1.61) |
| p | NS | NS | NS | NS |
SD=Standard deviation; NS=Not significant.
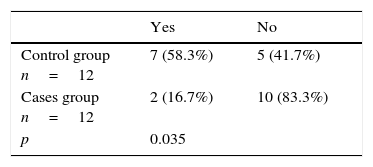
Another parameter which was evaluated to determine if the proposed technique for postoperative analgesia was effective was the use of rescue drugs, which were administered to patients when the VAS value was equal to or greater than 7 at the time of their evaluation. Of the total number of patients, 62.5% did not require the use of rescue analgesics, against the 37.5% that did require the administration of Tramadol.
We observed that a larger number of patients in the control group required the administration of rescue analgesics, with a statistically significant difference (Table 3).
DiscussionThe US-TAP BLOCK has demonstrated a reduction in postoperative pain and the dependence on analgesics after abdominal and gynecological surgery,11 when it is used as a part of a regimen of multimodal analgesics.
The findings of our study report that the US-TAP BLOCK technique has shown itself to be effective in pain control. Although its efficacy was only comparable and not superior to conventional methods, the two procedures can be considered effective through the VAS pain reports that showed light pain at the different hours of the evaluation.
The characteristics of the patients participating in our study show that, in our field, the female gender is more often affected by a diagnosis of biliary disease. Compared to other studies like that of Ra YS et al.,10 our population did not differ much in the BMI that they presented at the time of the surgical procedure, the majority were overweight. Regarding the average age of our patients (43.17±18.46), it was similar to the population of the control group in our study (43.4±12.4), and differed in our cases group, which was composed of patients around 26 years old.
When compared with other published studies on the use of the US-TAP BLOCK in abdominal surgical procedures, we found that the values reported in the pain evaluation, applying the technique with different concentrations and local anesthetics, did not differ much between the control and cases groups. For example, Mun Gyu et al.12 used the blockade in the total extraperitoneal plasty for the management of inguinal hernias, using ropivacaine at 0.375%, and found that, at 4h, the values of the numerical pain scale were 3.11±2.00 in the control group and 2.61±1.56 in the TAP group. Our study reports an evaluation of pain at the same postoperative time, values similar to 3.08 in the control group and 2.25 in the cases group.
Niraj, et al.,13 in his study to evaluate the efficacy of the US-TAP BLOCK analgesia in patients submitted to an open appendectomy using bupivacaine at 0.5% and evaluating the pain through a VAS at 30min and 24h, found that the pain values at rest were reduced significantly after the block. The same study also revealed that the standard group required significantly more rescue antiemetics than the TAP group.
The majority of published studies used the application of the anesthetic in a single dose, but there are studies which report the blockade in a continual manner, which also show that postoperative pain was less in the TAP group, but with a greater emphasis on the first and second postoperative day at rest and in motion.15
Regarding the use of rescue analgesics, when comparing the groups of patients, we found an important decrease in the use of tramadol after the surgical procedure (p 0.035) in the cases group (US-TAP BLOCK), the same as reported by other studies like the one by Sharma, et al.,14 which reported a decrease in the use of tramadol 24h after the surgical procedure. Kadam Rao et al.,15 in a study which used the blockade application in a continuous manner, reported the use of rescue analgesics in two groups (control and TAP) in the recovery unit; The TAP group used significantly less.
We didn’t found any restrictions in the application of US-TAP BLOCK. There were no mishaps or complications during the performance of the procedures. We could mention that the cost of implementing this technique as a postoperative alternative rises because, more surgical time is required along with the acquisition of bupivacaine.
We can conclude that the US-TAP BLOCK, in our field, offers a lesser use of rescue analgesics after the procedure when compared to the normal management of postoperative analgesics.
Conflict of interestThe authors have no conflicts of interest to declare.
FundingThe resources financed come from the General Surgery Service at the “Dr. José E. González” University Hospital at the Autonomous University of Nuevo León.
Special thanks to Dr. Neri A. Álvarez Villalobos, Medical Statistics Support Coordinator at the Research Department of the School of Medicine at the Autonomous University of Nuevo León.