Fibromyalgia (FMS) is a prevalent, disabling syndrome characterized by chronic widespread musculoskeletal pain and symptoms such as sleep disturbance, fatigue, stiffness, distress, cognitive impairments and a high comorbidity with anxiety and depressive disorders. Although no curative treatment has yet been found, various therapeutic approaches have been developed in the fields of pharmacology and psychology. The present paper aims to offer a narrative review and a description for clinicians and researchers of psychological therapies that have been applied in a format group in FMS with strong or promising empirical support: i.e., Cognitive Behavioral Therapy (CBT), Acceptance and Commitment Therapy (ACT), Mindfulness-Based Stress Reduction (MBSR), Psychoeducational program for FMS (FibroQoL), Amygdala Retraining Therapy (ART), and Attachment-Based Compassion Therapy (ABCT). This review will offer a brief practical summary of each therapy protocol (session-by-session), their rationale and available evidence of their effectiveness.
La fibromialgia es un síndrome frecuente e incapacitante caracterizado por dolor crónico generalizado en el sistema musculoesquelético y síntomas como alteraciones del sueño, cansancio, rigidez, problemas cognitivos y una elevada comorbilidad con trastornos de ansiedad y depresivos. Aunque actualmente no se ha hallado un tratamiento curativo, existen varios tratamientos farmacológicos y no farmacológicos que han demostrado cierta efectividad. El presente artículo trata de ofrecer una descripción y una revisión descriptiva para especialistas clínicos e investigadores sobre los principales tratamientos psicológicos que se han sido aplicados en formato grupal para tratar la fibromialgia y que han obtenido un apoyo empírico consistente o prometedor: la terapia cognitivo-conductual (TCC), la terapia de aceptación y compromiso (ACT), el programa de reducción del estrés basado en mindfulness (REBM), el programa FibroQoL, la técnica de reentrenamiento de la amígdala (TRA) y la terapia de compasión basada en los estilos de apego (ABCT). Esta revisión ofrecerá una descripción de cada terapia (sesión a sesión) y una breve exposición de los principales resultados de efectividad.
Fibromyalgia syndrome (FMS) is a disabling condition characterized by chronic widespread musculoskeletal pain, increased pain sensitivity, including allodynia and hyperalgesia, with tenderness to touch but no known structural pathology in muscles, ligaments, or joints. Stiffness throughout the body, along with fatigue, and sleep, cognitive and mood disturbances are also common symptoms (Häuser et al., 2015). Patients with FMS typically present comorbidities with psychiatric disorders such as anxiety (13–63.8%) and depressive disorders (20–80%) (Fietta, Fietta, & Manganelli, 2007). It is usually diagnosed in women between the ages of 20 and 50 years (Häuser et al., 2015), and with an estimated prevalence of 1.8–2.9% in the general population (Branco et al., 2010; Heidari, Afshari, & Moosazadeh, 2017), it is the second most common rheumatic syndrome, after osteoarthritis (Sanada et al., 2015). FMS is associated with high direct and indirect costs in industrialized countries (Schaefer et al., 2011). It is the leading chronic pain condition in unemployment, produces the greatest number of days of absenteeism, and leads the incapacity benefits claim rate (Leadley, Armstrong, Lee, Allen, & Kleijnen, 2012).
Unfortunately, a curative treatment for FMS has not yet been found (Häuser et al., 2015). This, linked with an absence of knowledge about its specific pathophysiological mechanisms, makes FMS a great challenge for health professionals. More ubiquitous effects from non-pharmacologic than from pharmacologic treatments have been reported (Perrot & Russell, 2014) and, recently, Thieme, Mathys, and Turk (2017) compared the guidelines on treatment of FMS issued by the American Pain Society (APS; Buckhardt et al., 2005), the Association of the Scientific Medical Societies in Germany (AWMF, 2012), the Canadian Pain Society (CPS; Fitzcharles et al., 2013), and the European League Against Rheumatism (EULAR; Macfarlane et al., 2017) and observed differences among their recommendations. Their work also revealed that the only consensual, strongly recommended treatment for FMS is physical exercise. Additionally, Cognitive Behavioral Therapy (CBT) and multicomponent therapy (including at least 1 educational or other psychological therapy with at least 1 exercise therapy; Häuser, Bernardy, Arnold, Offenbächer, & Schiltenwolf, 2009) are also strongly recommended by all the groups except EULAR. Pharmacotherapy is not recommended by AWMF and EULAR, while CPS and APS only recommend the use of amitriptyline, anticonvulsants and duloxetine, or only amitriptyline, respectively.
Psychological approaches in FMS aim to treating specific symptoms such as sleep problems, stress, anxiety and depression or unhelpful coping strategies which are highly relevant in the syndrome (Macfarlane et al., 2017). The present review will describe both well-established and other promising psychotherapies not yet included in the guidelines for FMS or other chronic-pain conditions. Our goal is to inform clinicians and researchers on the state of the art in psychological interventions for FMS and, thus, each intervention will contain a brief description of the theoretical foundation and indications for FMS, together with a summary of the evidence of their rationale and effectiveness. A summarized treatment protocol, detailed session-by-session, is also provided.
Well-established psychological therapies for FMSThe gold-standard psychotherapy for FMS is Cognitive Behavioral Therapy (CBT) according to the Division 12 of the American Psychological Association (2016), as it is a research-supported psychological treatment with strong evidence. Similarly, “third wave” CBT – Acceptance and Commitment Therapy (ACT) – has strong research support for chronic/persistent pain and the FibroQoL program has also obtained strong evidence of effectiveness in FMS.
Cognitive-Behavioral Therapy (CBT)Theoretical foundation and indications for fibromyalgiaCBT is the predominant psychotherapy with an extensive evidence-base of efficacy evaluated by means of randomized controlled trials across a wide range of health conditions. CBT is based on three principles: the access hypothesis, which asserts that thoughts can be accessed and are not “unconscious”; the mediation hypothesis, which states that our thoughts mediate our emotional and behavioral responses to the situations in which we find ourselves; and the change hypothesis, which maintains that we humans can intentionally modify the way we respond to events around us. Emotions, thoughts and behaviors influence each other according to this theory and, thus, dysfunctional thoughts, which are shaped by the patient's belief system, are responsible for pathological negative emotions (Bennett & Nelson, 2006).
As far as FMS and other chronic pain conditions are concerned, CBT attempts to change negative thoughts and maladaptive behaviors about pain to improve function and coping; these changes are fostered through several techniques such as problem-solving, stress and pain coping strategies, and relaxation (Bernardy, Klose, Busch, Choy, & Häuser, 2013; Turk, Meichenbaum, & Genest, 1983). The gate-control theory of pain (Melzack & Wall, 1965) and operant conditioning theory are the main models underlying the effects of CBT (Bennett & Nelson, 2006).
CBT considers that affective, behavioral, cognitive, and sensory or physical aspects play an important role in the patient's experience of pain, and underline the influence of the individual's beliefs on the pain experience (Bennett & Nelson, 2006; Bernardy, Klose, Welsch, & Häuser, 2017). Some of the main goals of CBT are increasing the patient's sense of personal control over pain, decreasing dysfunctional thought patterns about pain and its effects, and adapting behavior to the patient's condition, which in some cases would imply increasing daily activity and in others, reducing it to healthier levels (van Koulil et al., 2008).
Evidence of effectivenessCBT is considered to be the most widely-studied psychological therapy, as its effects have been tested on several conditions: substance use disorder, schizophrenia and other psychotic disorders, depression and dysthymia, bipolar disorder, anxiety disorders, somatoform disorders, eating disorders, insomnia, personality disorders, anger and aggression, general stress, chronic pain, and distress due to medical conditions. Generally, the findings have been positive and moderate effect sizes have been reported for most of those problems (Hofmann, Asnaani, Vonk, Sawyer, & Fang 2012).
However, with regard to FMS, as explained in the introduction, the American Pain Society (Buckhardt et al., 2005) gave the highest recommendation grade to CBT based on qualitative systematic reviews, whereas the European League Against Rheumatism gave only a weak (expert opinion) recommendation for CBT (Macfarlane et al., 2017). This divergence is reflected in the distinct findings on the effectiveness of CBT on FMS reported to date. On the one hand, some studies have reported small or inexistent effects of CBT on key FMS symptoms such as pain, fatigue, sleep disturbances, and limitations on quality of life (Bennett & Nelson, 2006; Bernardy, Klose, Welsch, & Häuser, 2017; van Koulil et al., 2008) and concluded that CBT would only be effective in alleviating depressed mood. On the other hand, other reviews (Goldenberg, Burckhardt, & Crofford, 2004; Rossy et al., 1999; Thieme & Gracely, 2009) do report significant, sustained-through-time effects of CBT on the main symptoms of FMS. These discordant results may be explained by the differing samples and analytical methods (i.e., qualitative vs. quantitative).
Taking all this into account, it is noteworthy that CBT has the highest level of evidence (1A) according to the CPS (2012) for FMS focused on improving patients’ functionality (Clauw, 2014). If we consider the most recent reviews and meta-analyses, we could conclude that CBT reduces the main symptoms of FMS after six months (Bernardy, Klose, Welsch, & Häuser, 2017) and its effects are robust and sustained through time, although they are usually small and require a high number of sessions to manifest themselves (Glombiewski et al., 2010).
Outline of a CBT intervention for FMSAlthough there are various applications of CBT in FMS, some common key strategies stand out: cognitive restructuring (i.e., confronting negative and catastrophic thoughts about pain and its consequences), education (i.e., teaching the meaning of the stress-tension-pain circle) and coping strategies (i.e., relaxation, social skills training). The treatment is usually administered in the fashion of a Socratic dialogue (Thieme, Flor, & Turk, 2006).
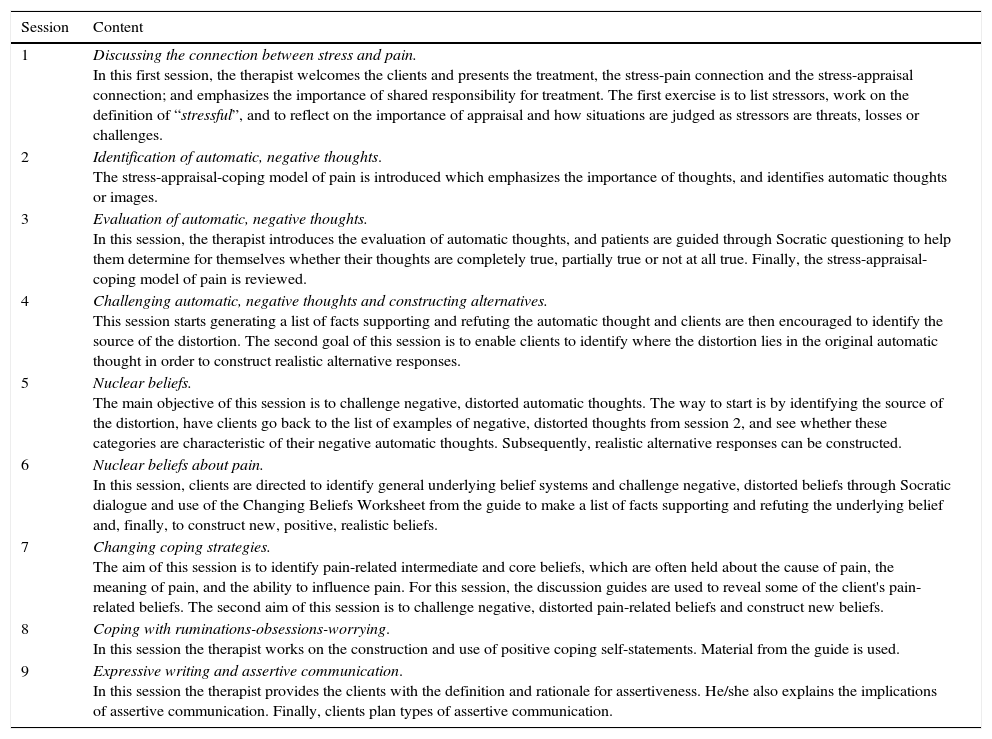
The materials described below are all from “Cognitive therapy for chronic pain: a step-by step guide” (Thorn, 2004), a program used in a recent article on the effectiveness and cost-effectiveness of CBT in FMS (Alda et al., 2011; Luciano, Guallar, et al., 2014; Luciano, D’Amico, et al., 2014). Sessions (nine 90-min, group-format) were structured as follows (Table 1).
CBT session-by-session for FMS.
| Session | Content |
|---|---|
| 1 | Discussing the connection between stress and pain. In this first session, the therapist welcomes the clients and presents the treatment, the stress-pain connection and the stress-appraisal connection; and emphasizes the importance of shared responsibility for treatment. The first exercise is to list stressors, work on the definition of “stressful”, and to reflect on the importance of appraisal and how situations are judged as stressors are threats, losses or challenges. |
| 2 | Identification of automatic, negative thoughts. The stress-appraisal-coping model of pain is introduced which emphasizes the importance of thoughts, and identifies automatic thoughts or images. |
| 3 | Evaluation of automatic, negative thoughts. In this session, the therapist introduces the evaluation of automatic thoughts, and patients are guided through Socratic questioning to help them determine for themselves whether their thoughts are completely true, partially true or not at all true. Finally, the stress-appraisal-coping model of pain is reviewed. |
| 4 | Challenging automatic, negative thoughts and constructing alternatives. This session starts generating a list of facts supporting and refuting the automatic thought and clients are then encouraged to identify the source of the distortion. The second goal of this session is to enable clients to identify where the distortion lies in the original automatic thought in order to construct realistic alternative responses. |
| 5 | Nuclear beliefs. The main objective of this session is to challenge negative, distorted automatic thoughts. The way to start is by identifying the source of the distortion, have clients go back to the list of examples of negative, distorted thoughts from session 2, and see whether these categories are characteristic of their negative automatic thoughts. Subsequently, realistic alternative responses can be constructed. |
| 6 | Nuclear beliefs about pain. In this session, clients are directed to identify general underlying belief systems and challenge negative, distorted beliefs through Socratic dialogue and use of the Changing Beliefs Worksheet from the guide to make a list of facts supporting and refuting the underlying belief and, finally, to construct new, positive, realistic beliefs. |
| 7 | Changing coping strategies. The aim of this session is to identify pain-related intermediate and core beliefs, which are often held about the cause of pain, the meaning of pain, and the ability to influence pain. For this session, the discussion guides are used to reveal some of the client's pain-related beliefs. The second aim of this session is to challenge negative, distorted pain-related beliefs and construct new beliefs. |
| 8 | Coping with ruminations-obsessions-worrying. In this session the therapist works on the construction and use of positive coping self-statements. Material from the guide is used. |
| 9 | Expressive writing and assertive communication. In this session the therapist provides the clients with the definition and rationale for assertiveness. He/she also explains the implications of assertive communication. Finally, clients plan types of assertive communication. |
Another example of a CBT program applied in FMS can be found in van Koulil et al. (2008). Interestingly, these authors adapted the intervention to fit two distinct but prototypical targets when treating FMS: pain-avoidance and pain-persistence. The first treatment is aimed at diminishing fear of pain and increasing the level of daily activities, while the second treatment focuses on changing pain-persistence cognitions and achieving regulation of daily activities. Both treatment programs consist of 16 sessions, 4h a day, twice a week, plus one follow-up session 3 months after treatment in group format. Every session includes CBT and exercise training. In the 3rd, 9th and 15th sessions a significant relative is invited. Treatment protocols for the pain-avoidance and pain-persistence group interventions were based on techniques from standardized treatment protocols for FMS.
Acceptance and Commitment Therapy (ACT)Theoretical foundation and indications for FMSACT was originally conceived as a transdiagnostic psychotherapeutic approach based on both behavioral science and a comprehensive empirical analysis of human cognition (Hayes, Strosahl, & Wilson, 1999). ACT applies mindfulness and acceptance processes to a number of aspects including spirituality, values and the self (Hayes, 2004) and is based on a functional contextual program of basic research in language and cognition: Relational Frame Theory (Hayes, Barnes-Holmes, & Roche, 2001).
This theory points directly to the likelihood of cognitive fusion and the principle of experiential avoidance (defined as the unwillingness to remain in contact with aversive private experience and the action taken to alter the aversive experiences or the events that elicit them); to the danger of suppression and disputation; to the importance of cognitive defusion and experiential acceptance; to the importance of a certain sense of “self”; to the centrality of values; and to the creation of psychological flexibility to experience both good and bad feelings and control our behavior to create meaningful and rich lives (Hayes et al., 1999; Hayes, 2004).
With regard to ACT's clinical application, it assumes that the general context and purpose of action are the problems underlying every negative feeling, thought, memory or behavior, and thus it addresses modification of these aspects in order to achieve powerful changes (Hayes, 2004). One of the main treatment objectives in ACT is to improve functioning by increasing psychological flexibility. In ACT, psychological flexibility is defined as the ability to notice and accept interfering thoughts, emotions and bodily sensations without acting on them, to facilitate behavior in accordance with personal values and long-term goals despite the presence of those negative experiences (Hayes et al., 1999). Psychological flexibility is attained by training six psychological core processes (the hexaflex): acceptance, cognitive defusion, present moment awareness, contact with self-as context, values formulation and committed actions. These skills can be divided into two overlapping processes, i.e., mindfulness and acceptance on the one hand and commitment and behavioral change on the other hand (Hayes, Luoma, Bond, Masuda, & Lillis, 2006).
The application of ACT in chronic pain is based on evidence that objective pain is not related to suffering, functional reduction and impairment (Yang & McCracken, 2005); the only predictors of functional status are disposition to experience pain and the ability to act according to personal values while feeling pain (McCracken, Vowles, & Eccleston, 2004; Yu & McCracken, 2016). Thus, psychological flexibility means that painful sensations, feelings and thoughts are accepted, that attention is focused on the opportunities in current situations rather than on ruminating on past or catastrophizing about the future, and that behavior is focused on realizing valued goals instead of pain control (McCracken & Vowles, 2014). According to these principles, people trained in accepting pain and not identifying with their thoughts about pain, tolerate it considerably better.
Evidence of effectivenessMany psychological disorders and medical conditions have responded positively to ACT. Some examples are substance use disorders (Lee, An, Levin, & Twohig, 2015), anxiety and obsessive-compulsive disorders (Bluett, Homan, Morrison, Levin, & Twohig, 2014), and cancer (Feros, Lane, Ciarrochi, & Blackledge, 2011; Hulbert-Williams, Storey, & Wilson, 2015). Regarding chronic pain, ACT has been able to produce small but significant effects on pain intensity, depression, anxiety, physical well-being, and quality of life (Veehof, Trompetter, Bohlmeijer, & Schreurs, 2016), and has recently been listed by the American Psychological Association, Division 12, as the empirically supported treatment for ‘Chronic or Persistent Pain in General’ (APA Division 12, 2016a).
In the specific case of FMS, the effectiveness of ACT has just started to be evaluated. As reported in different studies (Hughes, Clark, Colclough, Dale, & McMillan, 2017; Luciano, Guallar, et al., 2014; Luciano, D’Amico, et al., 2014), ACT produces significant improvements with large effect sizes in acceptance, psychological flexibility, and global functioning; and small but significant changes in pain catastrophizing, subjective quality of life, anxiety and depression, and acceptance and psychological flexibility. These results suggest that ACT is an effective intervention when addressed to FMS patients.
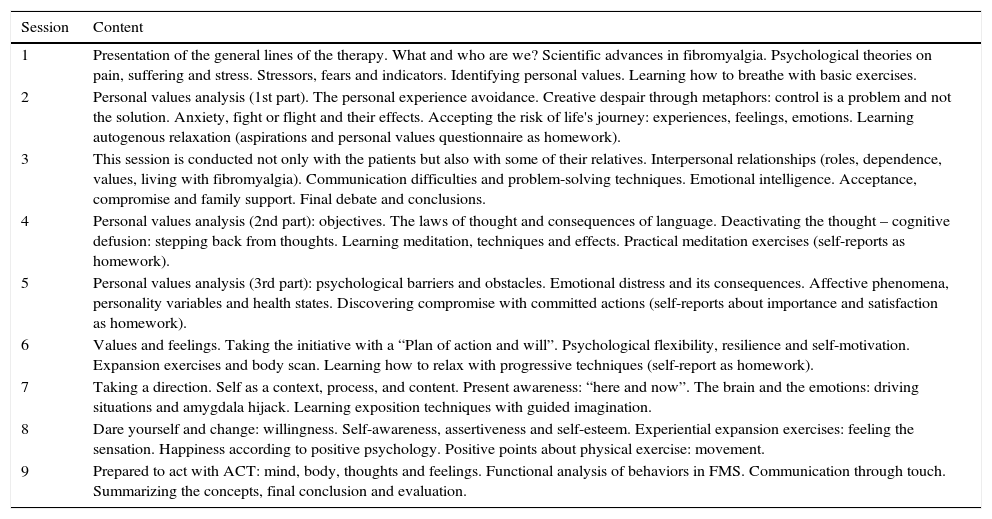
Outline of an ACT intervention for FMSThe ACT intervention protocol can be found in Wilson and Luciano (2002) (Table 2).
ACT session-by-session for FMS.
| Session | Content |
|---|---|
| 1 | Presentation of the general lines of the therapy. What and who are we? Scientific advances in fibromyalgia. Psychological theories on pain, suffering and stress. Stressors, fears and indicators. Identifying personal values. Learning how to breathe with basic exercises. |
| 2 | Personal values analysis (1st part). The personal experience avoidance. Creative despair through metaphors: control is a problem and not the solution. Anxiety, fight or flight and their effects. Accepting the risk of life's journey: experiences, feelings, emotions. Learning autogenous relaxation (aspirations and personal values questionnaire as homework). |
| 3 | This session is conducted not only with the patients but also with some of their relatives. Interpersonal relationships (roles, dependence, values, living with fibromyalgia). Communication difficulties and problem-solving techniques. Emotional intelligence. Acceptance, compromise and family support. Final debate and conclusions. |
| 4 | Personal values analysis (2nd part): objectives. The laws of thought and consequences of language. Deactivating the thought – cognitive defusion: stepping back from thoughts. Learning meditation, techniques and effects. Practical meditation exercises (self-reports as homework). |
| 5 | Personal values analysis (3rd part): psychological barriers and obstacles. Emotional distress and its consequences. Affective phenomena, personality variables and health states. Discovering compromise with committed actions (self-reports about importance and satisfaction as homework). |
| 6 | Values and feelings. Taking the initiative with a “Plan of action and will”. Psychological flexibility, resilience and self-motivation. Expansion exercises and body scan. Learning how to relax with progressive techniques (self-report as homework). |
| 7 | Taking a direction. Self as a context, process, and content. Present awareness: “here and now”. The brain and the emotions: driving situations and amygdala hijack. Learning exposition techniques with guided imagination. |
| 8 | Dare yourself and change: willingness. Self-awareness, assertiveness and self-esteem. Experiential expansion exercises: feeling the sensation. Happiness according to positive psychology. Positive points about physical exercise: movement. |
| 9 | Prepared to act with ACT: mind, body, thoughts and feelings. Functional analysis of behaviors in FMS. Communication through touch. Summarizing the concepts, final conclusion and evaluation. |
For other examples of an ACT protocol for FMS, check Wicksell et al. (2013) and Kemani et al. (2015). These protocols consist of 12, weekly, group sessions (5–6 participants in each group) organized in four phases, with both in-session exercises and homework assignments in addition to illustrations and metaphors. Phase 1 includes sessions 1 and 2 and the objective is to alter the context in which pain symptoms and avoidance behaviors occurs along with initiating a shift in perspective from symptom reduction to valued living. In phase 2 (sessions 3 and 4) the workability of previous strategies to reduce pain is evaluated and the therapist teaches more flexible behaviors in relation to pain and distress. Additionally, personal values are formulated and clarified. In phase 3 (sessions 5 and 6) the focus is on disengagement from verbal processes, to decrease the negative impact of thoughts and experiences on behavior (cognitive defusion), and to willingly experience unpleasant private experiences that cannot be directly changed (acceptance). Sessions 7–12 comprise the 4th phase, where participants define short and long-term behavioral goals based on personal values (Kemani et al., 2015).
Psychoeducation for FMS (FibroQoL)Theoretical foundation and indications for FMSThe FibroQoL intervention was based on two consensus documents developed by expert and multidisciplinary groups. The first was published in 2006 by the Catalan Health Department (Nou Model d’Atenció a la Fibromiàlgia i la Síndrome de Fatiga Crònica) and the second in 2007 by the Barcelona College of Physicians (Quaderns de la Bona Praxi: Fibromiàlgia i Síndrome de Fatiga Crònica). This intervention is divided into two parts (Feliu-Soler et al., 2016): the first consisting of a psychoeducational approach which includes updated information about pathophysiology, diagnosis, and management of FMS symptoms (4 sessions); and the second is led by a psychologist and includes training in self-hypnosis (4 sessions). In each of these sessions, a distinct self-hypnosis technique is explained and practiced. The goal of these techniques is to generate a state of deep relaxation, explore the sensations produced by one's own body, achieve control over the body and pain, and imagine the one's life in the future without pain.
An extensive body of literature exists demonstrating that health education promotes self-management and improves health-related behaviors in chronic diseases. Well-informed patients are thought to be better prepared, since active and continuing health education can lead to greater patient autonomy, suggesting a lower intake of medication and less dependence on the health system. The group dynamics of FibroQoL also uses a constructivist focus to address patients’ dilemmas (Botella & Feixas, 1998; Feixas & Compañ, 2015), understood as a stagnation of the person in life choices, as he or she cannot behave in the desired way because of the implications of that change on the person's identity. These topics are considered nuclear in FMS, as patients often refer to a strong resistance to relaxing, which has been associated with some personality traits such as an excessive sense of responsibility, extreme desire to please and make sacrifices for others, and difficulties setting limits or “saying no”. In this regard, self-hypnosis emerges as a useful technique to overcome these barriers and achieve relaxation free of pain, automatic thoughts, and muscular and psychic tensions. These moments can represent a corrective emotional experience (Alexander & French, 1946) and a corrective physical experience, reclaiming control of the patients’ internal states and moments of peace.
Evidence of effectivenessAccording to the most recent European League Against Rheumatism (EULAR) guideline (Macfarlane et al., 2017) initial management of FMS should involve patient education and focus on nonpharmacological therapies. The educational approach is considered a very useful part of treatment (Carville et al., 2007), as patients get a better understanding of their condition and this helps to reduce associated stigma.
Psychoeducational interventions have been recommended in various guidelines with grade A of evidence for FMS (AIAQS, 2011; Alegre et al., 2010; Häuser et al., 2009; Häuser, Thieme, & Turk, 2010; Luciano et al., 2011, 2013; Mannerkorpi & Henriksson, 2007). The components of psychoeducational interventions usually include health education (Cedraschi et al., 2004; King, Wessel, Bhambhani, Sholter, & Maksymowych, 2002; Kirby, Dunwoody, & Millar, 2009; Mannerkorpi, Ahlmén, & Ekdahl, 2002) in conjunction with non-exhausting or aerobic exercise (Schachter, Busch, Peloso, & Sheppard, 2003; Valim et al., 2003) or relaxation programs (Mannerkorpi & Henriksson, 2007; Taggart, Arslanian, Bae, & Singh, 2003).
Regarding hypnosis, a systematic review and meta-analysis demonstrate clinically significant improvements in reducing pain and key symptoms of FMS (Zech, Hansen, Bernardy, & Häuser, 2017). It has also been demonstrated that it modulates unpleasant pain without affecting its intensity; for instance, the person subject to hypnosis can feel pain but is not so disturbed by the sensation (Garland et al., 2017; Kropotov, Crawford, & Polyakov, 1997; Montgomery, Duhamel, & Redd, 2000; Rainville, Carrier, Hofbauer, Bushnell, & Duncan, 1999). The reference model used in FibroQoL is Ericksonian hypnosis (Erickson, 1958, 1959–1989), a type of hypnosis “tailored” to the patient which uses the patient's previous experiences, resources and learning therapeutically. Not only the typical properties of hypnosis are used in this intervention (experience of absorption of attention, ability to change the strength of experience, suggestibility, flexibility of the time-space relationship and alteration of sensory experience) but also an attempt at decomposition of unnecessary or limited patterns and of behaviors that prevent the construction of new meanings.
The FibroQoL intervention has proved its effectiveness in FMS. Luciano et al. (2011) observed an improvement in global functional status, physical impairment, days not feeling well, pain, general fatigue, morning fatigue, stiffness, anxiety, and depression when the psychoeducational intervention is finished, with a medium effect size in most cases and maintained at one-year follow-up. The FibroQoL intervention is not only more effective than usual treatment applied in Spanish primary care but is also a more cost-effective approach (Luciano et al., 2013).
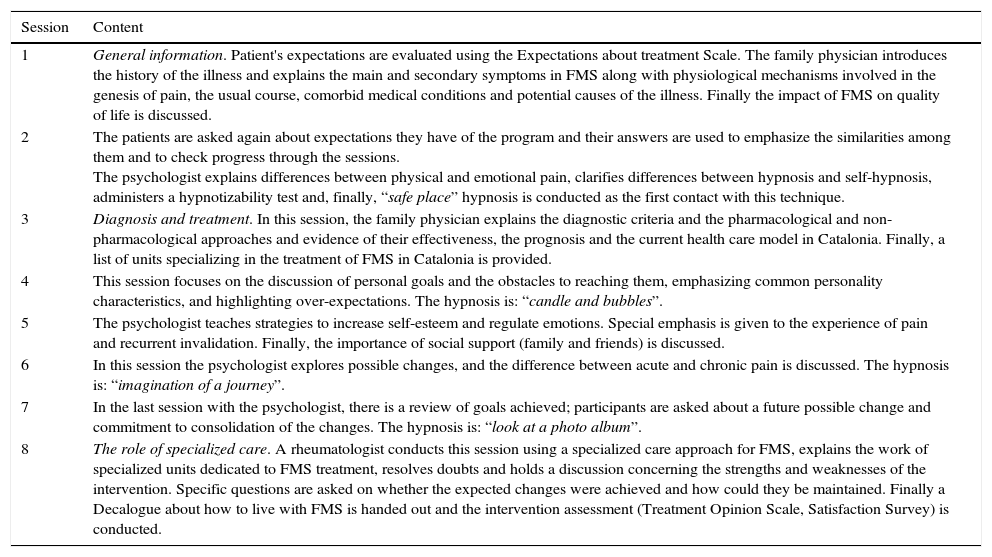
Outline of the FibroQoL program for FMSThe FibroQoL intervention consists of weekly sessions of 2h each over 8 consecutive weeks. Participants are allocated to groups with a maximum of 18 per group. The sessions are conducted by a multidisciplinary group (family physicians, psychologists and a rheumatologist) in a participative style, so the participants can intervene when they feel like it with the intention of generating a team atmosphere among participants and speakers.
At the beginning of the intervention, the recently-published “Debut Guide in Fibromyalgia” (ADFM, 2015) is handed out to each participant as support material. In addition, after each session some patient information sheets are distributed to remind patients about the health information covered.
Although the intervention is tailored for the patients and for the specific group, meaning that each therapy cycle may differ regarding the content of the sessions, the basic and general structure is as follows (Table 3).
FibroQoL session-by-session for FMS.
| Session | Content |
|---|---|
| 1 | General information. Patient's expectations are evaluated using the Expectations about treatment Scale. The family physician introduces the history of the illness and explains the main and secondary symptoms in FMS along with physiological mechanisms involved in the genesis of pain, the usual course, comorbid medical conditions and potential causes of the illness. Finally the impact of FMS on quality of life is discussed. |
| 2 | The patients are asked again about expectations they have of the program and their answers are used to emphasize the similarities among them and to check progress through the sessions. The psychologist explains differences between physical and emotional pain, clarifies differences between hypnosis and self-hypnosis, administers a hypnotizability test and, finally, “safe place” hypnosis is conducted as the first contact with this technique. |
| 3 | Diagnosis and treatment. In this session, the family physician explains the diagnostic criteria and the pharmacological and non-pharmacological approaches and evidence of their effectiveness, the prognosis and the current health care model in Catalonia. Finally, a list of units specializing in the treatment of FMS in Catalonia is provided. |
| 4 | This session focuses on the discussion of personal goals and the obstacles to reaching them, emphasizing common personality characteristics, and highlighting over-expectations. The hypnosis is: “candle and bubbles”. |
| 5 | The psychologist teaches strategies to increase self-esteem and regulate emotions. Special emphasis is given to the experience of pain and recurrent invalidation. Finally, the importance of social support (family and friends) is discussed. |
| 6 | In this session the psychologist explores possible changes, and the difference between acute and chronic pain is discussed. The hypnosis is: “imagination of a journey”. |
| 7 | In the last session with the psychologist, there is a review of goals achieved; participants are asked about a future possible change and commitment to consolidation of the changes. The hypnosis is: “look at a photo album”. |
| 8 | The role of specialized care. A rheumatologist conducts this session using a specialized care approach for FMS, explains the work of specialized units dedicated to FMS treatment, resolves doubts and holds a discussion concerning the strengths and weaknesses of the intervention. Specific questions are asked on whether the expected changes were achieved and how could they be maintained. Finally a Decalogue about how to live with FMS is handed out and the intervention assessment (Treatment Opinion Scale, Satisfaction Survey) is conducted. |
Besides the well-established psychotherapies, other psychological treatments have been studied in recent years with some promising results regarding FMS; Mindfulness-Based Interventions (MBI), such as Mindfulness-Based Stress Reduction (MBSR) and Mindfulness-Based Cognitive Therapy (MBCT), the Amygdala Retraining Technique (ART), and Attachment-Based Compassion Therapy (ABCT).
Mindfulness-Based Interventions (MBI)Theoretical foundation and indications for FMSMBI were developed for people with chronic physical problems who were managing pain, low mood and health-related anxiety (Alsubaie et al., 2017). Mindfulness is defined as the “awareness that emerges through paying attention on purpose, in the present moment, and nonjudgmentally to the unfolding of experience” (Kabat-Zinn, 2003) and has been described as a multifaceted construct (observe, describe, act with awareness, nonjudge and nonreact) (Baer, Smith, Hopkins, Krietemeyer, & Toney, 2006). Since the first program based on mindfulness meditation was conceived, a number of interventions have been designed targeting various medical and psychological conditions. Among these interventions are Mindfulness-Based Stress Reduction (MBSR; Kabat-Zinn, 1982), Mindfulness-Based Cognitive Therapy (MBCT; Segal, Wiliams, & Teasdale, 2001) and Mindfulness-Based Pain Management (Burch, 2008).
On the one hand, MBSR was proposed as a coadjuvant medical intervention for patients suffering from chronic pain conditions, aiming to relieve suffering through the practice of mindfulness. Patients’ repeated practice of mindfulness helps them to learn how to pause and choose their response to difficulty rather than reacting impulsively. MBSR supports the development of a nonjudgmental stance toward one's experiences and helps participants find adaptive strategies to deal with stressful events (Keng, Smoski, & Robins, 2011). On the other hand, MBCT, which integrates MBSR with CBT, was developed as a relapse prevention treatment in those with high risk of recurring depression but has been adapted to other conditions (Alsubaie et al., 2017). Finally, MBPM has a distinctive approach to mindfulness in daily life and mindful movement together with compassion and acceptance meditation as part of the core curriculum (Burch, 2008).
MBI include a range of formal mindfulness practices as a key method for training attentional control as well as the non-judgmental attitudinal dimensions of mindfulness (Crane et al., 2017). Distinct psychological mechanisms underlying mindfulness effects are attentional processes, such as decreased vigilance to threat cues (Garland & Howard, 2013); emotional processes, such as increased distress tolerance and positive affective reactivity (Holzel et al., 2011); and cognitive-evaluative processes, such as decreased pain catastrophizing and increased pain acceptance (Davis, Zautra, Wolf, Tennen, & Yeung, 2015). Together, these mechanisms help the patients to modulate the subjective experience of pain (Ludwig & Kabat-Zinn, 2008).
Evidence of effectivenessSome systematic reviews have concluded that MBSR and MBCT have small to medium effect sizes on psychological and physical symptoms across a range of chronic somatic conditions including cancer, cardiovascular disorders and arthritis (Abbott et al., 2014; Bohlmeijer, Prenger, Taal, & Cuijpers, 2010; Hofmann, Sawyer, Witt, & Oh, 2010).
Regarding MBSR, most of the studies conducted to date have concluded that it has benefits in clinical populations with psychiatric disorders such as depression or anxiety, both highly comorbid with FMS (Dell’Osso et al., 2015), as it reduces distress and teaches patients skills to handle their symptoms (Fjorback, Arendt, Ornbol, Fink, & Walach, 2011). Furthermore, it has proved to be therapeutic not only for patients but also for healthcare providers, with no side effects reported (Praissman, 2008). Moreover, various systematic reviews have shown that MBSR might be effective for chronic pain conditions (Chiesa & Serretti, 2011; Cramer, Haller, Lauche, & Dobos, 2012; Veehof et al., 2016). According to these results, MBSR may be effective for pain intensity and stress and anxiety reduction, although no more than other active treatments such as CBT. Prior uncontrolled trials of MBSR (Kaplan, Goldenberg, & Galvin-Nadeau, 1993; Quintana & Fernández, 2011; Rosenzweig et al., 2010; Singh, Berman, Hadhazy, & Creamer, 1998) showed significant improvements in pain, sleep, fatigue and depression. Some reviews (Kozasa et al., 2012; Lakhan & Schofield, 2013) have reported on the effectiveness of mindfulness-based therapies or meditation-based therapies, such as MBSR, on somatization disorders, including FMS, but these reviews present some methodological issues that lead us to consider these conclusions with caution.
As far as FMS is concerned, some studies (Cash et al., 2015; Schmidt et al., 2011; Sephton et al., 2007; Gordon, Shonin, Dunn, Garcia-Campayo, & Griffiths, 2017) found that MBSR achieved improvements in some of the major FMS symptoms and reduced subjective illness burden. Systematic reviews (Crowe et al., 2016; Lauche, Cramer, Dobos, Langhorst, & Schmidt, 2013) reported low-quality evidence for a small, short-term improvement in pain and quality of life after MBSR when compared to usual care or active control interventions, although no evidence was found for long-term effects.
On the subject of MBCT, it has been reported that it can decrease depression, anxiety and fatigue in some physical conditions, such as coronary heart disease (O’Doherty et al., 2015), diabetes (van Son et al., 2014) and cancer (van der Lee & Garssen, 2012). To the best of our knowledge, only one randomized controlled trial (RCT) testing its effectiveness in FMS has been conducted (Parra-Delgado & Latorre-Postigo, 2013) with promising results but with a relatively small sample (n=33). Thus, further research is required to assess MBCT effectiveness in FMS.
Outline of the MBSR program for FMSThe original curriculum (Kabat-Zinn, 1982) consists of weekly 2.5h group-based classes with a trained teacher, daily audio-guided home practice (approximately 45min/day), and a day-long mindfulness retreat (occurring during week 6 of the 8-week program) (Kabat-Zinn, 1990). Much of the MBSR program focuses on learning how to mindfully attend to bodily sensations through the use of body scans, gentle stretching, and yoga mindfulness exercises, along with discussions and practices geared toward applying mindful awareness to daily life experiences, including dealing with stress (Creswell, 2017).
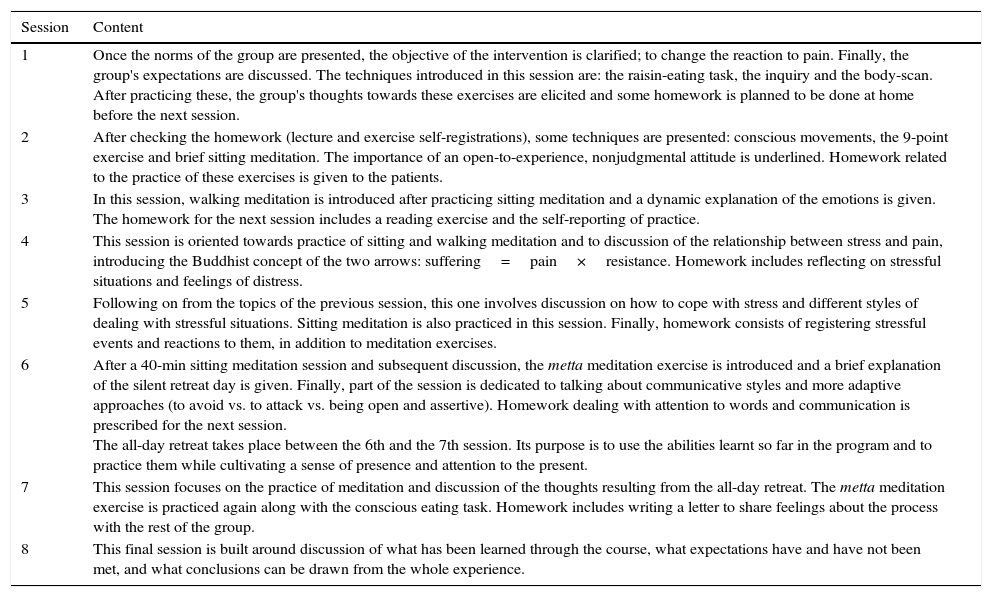
The following is a session-by-session description of the contents of this program as it is used in the ongoing study by Feliu-Soler et al. (2016). It is notable that this therapy includes a book “Con rumbo propio” with a CD for practice at home (Martin-Ausero, 2008) (Table 4).
MBSR session-by-session for FMS.
| Session | Content |
|---|---|
| 1 | Once the norms of the group are presented, the objective of the intervention is clarified; to change the reaction to pain. Finally, the group's expectations are discussed. The techniques introduced in this session are: the raisin-eating task, the inquiry and the body-scan. After practicing these, the group's thoughts towards these exercises are elicited and some homework is planned to be done at home before the next session. |
| 2 | After checking the homework (lecture and exercise self-registrations), some techniques are presented: conscious movements, the 9-point exercise and brief sitting meditation. The importance of an open-to-experience, nonjudgmental attitude is underlined. Homework related to the practice of these exercises is given to the patients. |
| 3 | In this session, walking meditation is introduced after practicing sitting meditation and a dynamic explanation of the emotions is given. The homework for the next session includes a reading exercise and the self-reporting of practice. |
| 4 | This session is oriented towards practice of sitting and walking meditation and to discussion of the relationship between stress and pain, introducing the Buddhist concept of the two arrows: suffering=pain×resistance. Homework includes reflecting on stressful situations and feelings of distress. |
| 5 | Following on from the topics of the previous session, this one involves discussion on how to cope with stress and different styles of dealing with stressful situations. Sitting meditation is also practiced in this session. Finally, homework consists of registering stressful events and reactions to them, in addition to meditation exercises. |
| 6 | After a 40-min sitting meditation session and subsequent discussion, the metta meditation exercise is introduced and a brief explanation of the silent retreat day is given. Finally, part of the session is dedicated to talking about communicative styles and more adaptive approaches (to avoid vs. to attack vs. being open and assertive). Homework dealing with attention to words and communication is prescribed for the next session. The all-day retreat takes place between the 6th and the 7th session. Its purpose is to use the abilities learnt so far in the program and to practice them while cultivating a sense of presence and attention to the present. |
| 7 | This session focuses on the practice of meditation and discussion of the thoughts resulting from the all-day retreat. The metta meditation exercise is practiced again along with the conscious eating task. Homework includes writing a letter to share feelings about the process with the rest of the group. |
| 8 | This final session is built around discussion of what has been learned through the course, what expectations have and have not been met, and what conclusions can be drawn from the whole experience. |
Finally, MBI have been adapted when applied to FMS patients in some aspects, such as MBCT in the study by Parra-Delgado and Latorre-Postigo (2013), which included a closer look at the acceptance of the experience of pain, automatic thoughts focusing on those related to pain and their relationship with the feelings and behaviors it caused. Additionally, and in response to patients’ requests, they provide information on anxiety and its cause.
Amygdala Retraining Technique (ART)Theoretical foundation and indications for FMSART was developed by Gupta in 2002, and its main objective is to treat the symptoms of patients with chronic fatigue syndrome and FMS (Navarro-Gil, 2017). Its principles are based on Ledoux's neurobiological theory of conditioned fear that maintains that the amygdala has a key role in the symptomatology of various disorders (Ledoux, 2000; Maren & Quirk, 2004). In addition, this theory explains that the constant conditioned response of the amygdala and other neural centers when aversive and traumatic events happen, causes problems in the immune and sympathetic systems, and the person can suffer consequent physical and mental problems such as those described in FMS (Ehrlich et al., 2009; Gupta, 2002; Morris, Ohman, & Dolan, 1999). In fact, the theory says that the conditioning of the amygdala generates a state of hypervigilance to threat, real or not, leading to an imbalance of homeostasis, which causes the body to react constantly with high levels of alarm, and this feeds back onto the state of hypervigilance (Gupta, 2010).
Based on this theory, ART has been designed with the aim of creating a neural network that connects the prefrontal cortex with the amygdala, assuming that this network will provoke a relaxation response when hypervigilance is triggered by a symptom, interrupting the amygdala's automatic response (Gupta, 2010).
Evidence of effectivenessDue to ART's relatively short existence, there is not much scientific research on the effectiveness of this therapy in FMS. In fact, ART is not even included in the most recent meta-analysis conducted on the efficacy of pharmacological and non-pharmacological treatments (Gupta, 2010; Nüesch, Häuser, Bernardy, Barth, & Jüni, 2013; Papadopoulou, Fassoulaki, Tsoulas, Siafaka, & Vadalouca, 2016). Additionally, the few studies that have been published on the effectiveness of ART on FMS have not followed a common methodology. These two factors make it difficult to carry out an in-depth analysis of the efficacy of ART. In spite of this, the few studies that do exist on the effectiveness of ART have shown promising results. For instance, in a pilot study conducted in patients diagnosed with FMS, chronic fatigue, or both, an ART with standard care group was compared with a standard care alone group. Patients in the intervention group achieved significant improvements in physical health, energy, pain, symptom distress and fatigue compared with patients in the control group (Toussaint, Whipple, Abboud, Vincent, & Wahner-Roedler, 2012). Another recent study evaluated the efficacy of Attachment-Based Compassion Therapy (ABCT), Mindfulness enriched with adaptation of the ART (Mindfulness+Amygdala and Insula Retraining) and an intervention based on relaxation techniques in patients with FMS. Results showed that FMS symptoms in patients in the M+AIR group improved significantly compared with the relaxation group, and these improvements were maintained at 3-month follow-up (Garcia-Campayo, personal communication). These results suggest that the ART is a promising treatment, although further research is required to provide more evidence and to overcome the methodological issues of those studies available.
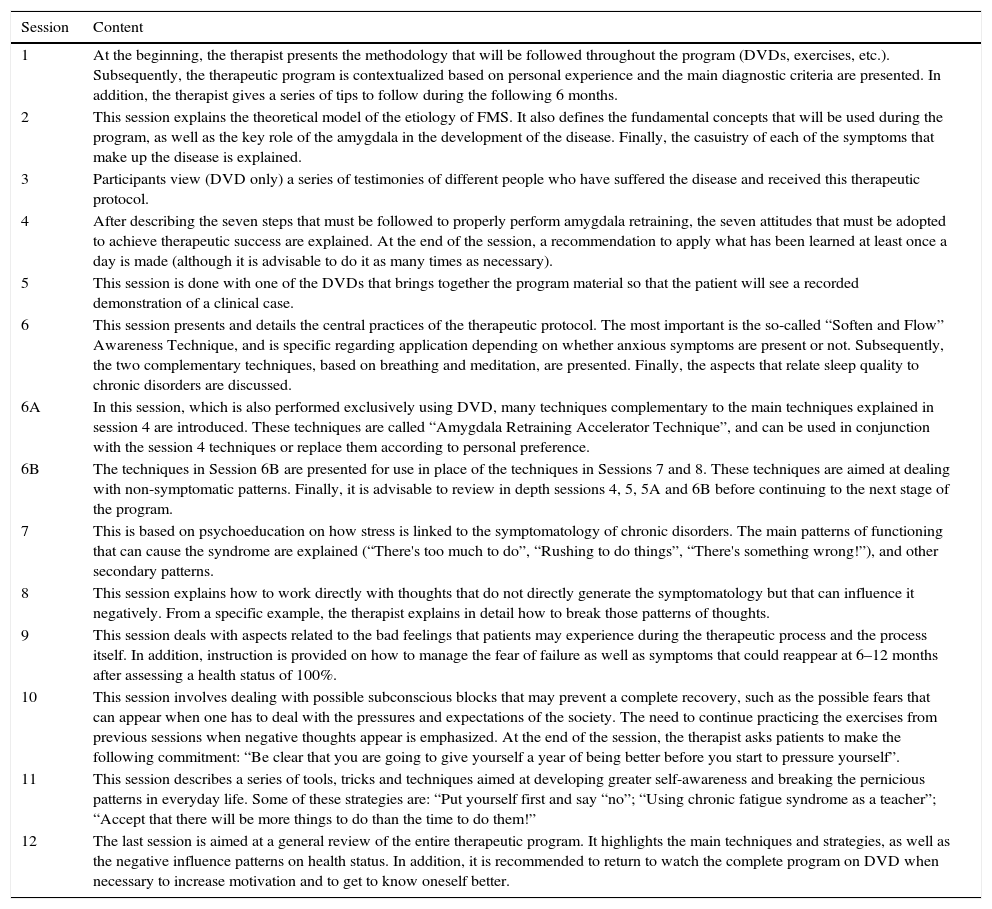
Outline of ART for FMSThe program consists of 14 sessions (18h) available on DVD that are accompanied by a manual (transcription of DVDs) and 2 CDs with exercises and guided meditations (Gupta, 2007). The sessions are structured as follows (Table 5).
ART session-by-session for FMS.
| Session | Content |
|---|---|
| 1 | At the beginning, the therapist presents the methodology that will be followed throughout the program (DVDs, exercises, etc.). Subsequently, the therapeutic program is contextualized based on personal experience and the main diagnostic criteria are presented. In addition, the therapist gives a series of tips to follow during the following 6 months. |
| 2 | This session explains the theoretical model of the etiology of FMS. It also defines the fundamental concepts that will be used during the program, as well as the key role of the amygdala in the development of the disease. Finally, the casuistry of each of the symptoms that make up the disease is explained. |
| 3 | Participants view (DVD only) a series of testimonies of different people who have suffered the disease and received this therapeutic protocol. |
| 4 | After describing the seven steps that must be followed to properly perform amygdala retraining, the seven attitudes that must be adopted to achieve therapeutic success are explained. At the end of the session, a recommendation to apply what has been learned at least once a day is made (although it is advisable to do it as many times as necessary). |
| 5 | This session is done with one of the DVDs that brings together the program material so that the patient will see a recorded demonstration of a clinical case. |
| 6 | This session presents and details the central practices of the therapeutic protocol. The most important is the so-called “Soften and Flow” Awareness Technique, and is specific regarding application depending on whether anxious symptoms are present or not. Subsequently, the two complementary techniques, based on breathing and meditation, are presented. Finally, the aspects that relate sleep quality to chronic disorders are discussed. |
| 6A | In this session, which is also performed exclusively using DVD, many techniques complementary to the main techniques explained in session 4 are introduced. These techniques are called “Amygdala Retraining Accelerator Technique”, and can be used in conjunction with the session 4 techniques or replace them according to personal preference. |
| 6B | The techniques in Session 6B are presented for use in place of the techniques in Sessions 7 and 8. These techniques are aimed at dealing with non-symptomatic patterns. Finally, it is advisable to review in depth sessions 4, 5, 5A and 6B before continuing to the next stage of the program. |
| 7 | This is based on psychoeducation on how stress is linked to the symptomatology of chronic disorders. The main patterns of functioning that can cause the syndrome are explained (“There's too much to do”, “Rushing to do things”, “There's something wrong!”), and other secondary patterns. |
| 8 | This session explains how to work directly with thoughts that do not directly generate the symptomatology but that can influence it negatively. From a specific example, the therapist explains in detail how to break those patterns of thoughts. |
| 9 | This session deals with aspects related to the bad feelings that patients may experience during the therapeutic process and the process itself. In addition, instruction is provided on how to manage the fear of failure as well as symptoms that could reappear at 6–12 months after assessing a health status of 100%. |
| 10 | This session involves dealing with possible subconscious blocks that may prevent a complete recovery, such as the possible fears that can appear when one has to deal with the pressures and expectations of the society. The need to continue practicing the exercises from previous sessions when negative thoughts appear is emphasized. At the end of the session, the therapist asks patients to make the following commitment: “Be clear that you are going to give yourself a year of being better before you start to pressure yourself”. |
| 11 | This session describes a series of tools, tricks and techniques aimed at developing greater self-awareness and breaking the pernicious patterns in everyday life. Some of these strategies are: “Put yourself first and say “no”; “Using chronic fatigue syndrome as a teacher”; “Accept that there will be more things to do than the time to do them!” |
| 12 | The last session is aimed at a general review of the entire therapeutic program. It highlights the main techniques and strategies, as well as the negative influence patterns on health status. In addition, it is recommended to return to watch the complete program on DVD when necessary to increase motivation and to get to know oneself better. |
Nowadays, there are many definitions of compassion from both the Eastern and the Western point of view, although one of the most-commonly used is provided by Goetz and colleagues (Goetz, Keltner, & Simon-Thomas, 2010) who define compassion as “the feeling that arises in witnessing another's suffering and that motivates a subsequent desire to help” (p. 351). According to Simon, the two key elements of compassion are sensitivity to the suffering of others and oneself, and the commitment to alleviate that suffering (Simón, 2014). Regarding its nature, there are authors who emphasize compassion as a trait, and others who argue that what is really important is that this construct can be developed through practice (Elices et al., 2017).
One of the main theoretical foundations of compassion-based interventions is the evolutionary model of social mentality theory, which suggests that people develop a style of relationship with themselves from systems developed to relate to others (Gilbert & Procter, 2006; Hermanto & Zuroff, 2016). These relationships are shaped by the interaction between the psychophysiological and social signals mediated by the main human brain circuits: the system of satisfaction, calm and safety; the threat-protection system; and the achievement system (García-Campayo & Demarzo, 2015; Gilbert, 2009, 2014). According to this theory, current society is characterized by a great increase in the activity of both the threat system associated with self-criticism and shame and high levels of cortisol and adrenaline. The achievement system that correlates with consumerism and social climbing linked to the activity of dopamine, while the system of satisfaction and calm is hypoactivated (related to the levels of oxytocin in the blood) (García-Campayo & Demarzo, 2015; Gilbert, 2015). Compassion therapy would therefore allow activation of the system of calm and satisfaction, which would produce a better balance in the excess activation of the other two systems, and this would facilitate the development of a general state of peace and happiness, thus reducing the impact of pathology on people's health (García-Campayo & Demarzo, 2015; Neff, Kirkpatrick, & Rude, 2007).
According to García-Campayo and Demarzo (2015), the main mechanisms of action of compassion-based therapies are: a decrease in self-criticism (thanks to the feelings of common humanity that is developed with the practice of compassion. People describe their weaknesses, not as something unique to them but as something common in society); a decrease in ruminations (this allows people to break the cycle of negative self-messages and accept their own imperfections and weaknesses more adaptively); re-perception of negative life events (self-compassion allows people to take responsibility for their problems with better psychological health as it facilitates the understanding that problems and difficult situations seem to be common among other people in the world); and Emotional Regulation (thanks to self-compassion people do not suppress negative emotions or thoughts and allow people to recognize that all emotional experience is valid and has a role in the survival of the human being). Finally, one of the key aspects of compassion-based therapies is that, unlike the psychological therapies of previous generations, compassion places the focus of therapy on the development of affiliative and prosocial functioning, which reduces the impact of pathology on people's health (García-Campayo & Demarzo, 2015; Neff et al., 2007).
Evidence of effectivenessIn recent years, compassion therapy has been studied in different psychopathologies, including depression and anxiety, psychosis, trauma-related symptoms, eating disorders and personality disorders. Overall, the size of the effect found was large for the relation between compassion and psychopathology, indicating a strong association between a higher level of compassion and lower levels of psychopathology (Beaumont & Hollins-Martin, 2015; MacBeth & Gumley, 2012). Specifically, a recent meta-analysis found moderate effect sizes in pre-post intervention comparison and in measures of compassion, self-compassion, mindfulness, and well-being as well as moderate effect sizes in reducing suffering in people with anxiety, depression and psychological stress (Kirby, Tellegen, & Steindl, 2017). However, there are very few studies on FMS, chronic pain or similar pathologies; in fact, a systematic review in 2014 on the psychotherapeutic benefits of Compassion-Focused Therapy and a recent meta-analysis of the effects of compassion-based interventions on different measures did not include any study in these diseases (Carson, 2005; Kirby et al., 2017; Leaviss & Uttley, 2015). Nevertheless, existing research shows promising results that favor continuity of this line of research. For example, in a study conducted in patients with chronic pain, it was observed that compassion decreased self-criticism and isolation, and reduced identification with thoughts (Costa & Pinto-Gouveia, 2011). In another pilot study of patients with chronic pain comparing an experimental group (9-week compassion cultivation intervention) and a waiting-list control group, results showed that participants in the experimental group significantly reduced the severity of perceived pain and increased acceptance of pain compared with participants in the control group (Chapin et al., 2014). Finally, a recent study evaluating the effectiveness of an attachment-based compassion therapy in patients diagnosed with FMS showed that this intervention was more effective than a relaxation-based treatment; the people in the experimental group (ABCT) experienced an increase in general health status as well as a reduction of the anxiety and depressive symptomatology associated with the syndrome (Navarro-Gil, 2017).
Outline of ABCT for FMS (reproduced with the permission of García-Campayo, Navarro-Gil, & Demarzo, 2016)Currently, there are several standardized therapeutic programs based on compassion but none is specific for FMS. These interventions are: Cognitive-based Compassion Therapy (Pace et al., 2009), Compassion Cultivation Training (Jazaieri et al., 2015), Compassion Focused Therapy (Gilbert, 2015) and Mindful Self-Compassion (Neff, 2012).
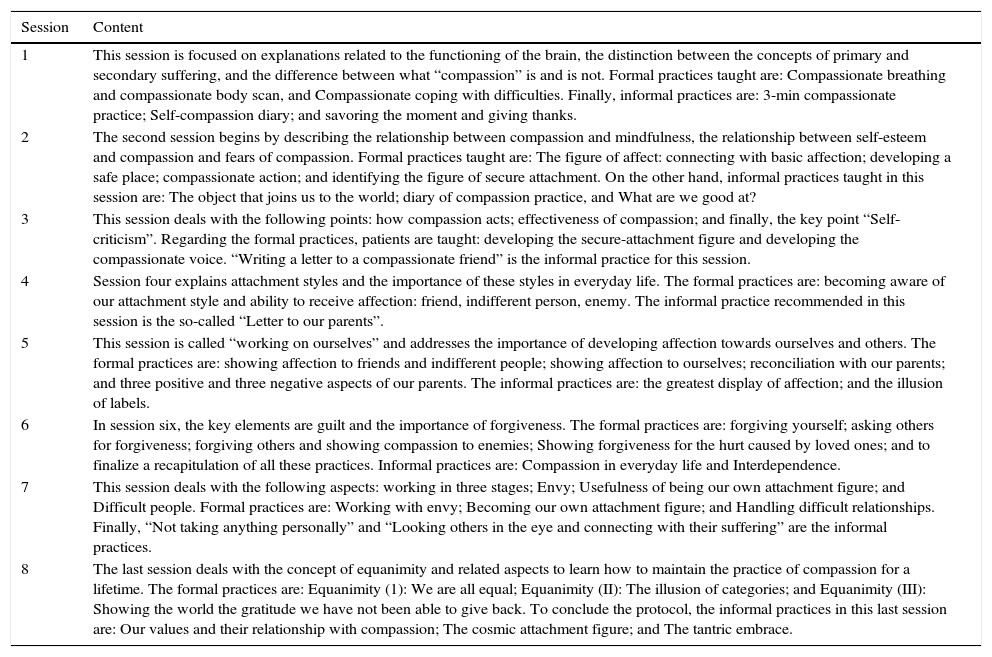
In addition to these protocols, in 2015 the University of Zaragoza together with the Federal University of Sao Paulo developed and published Attachment-based Compassion Therapy (García-Campayo & Demarzo, 2015), and recently a doctoral thesis has been published evaluating its efficacy in patients with FMS (Navarro-Gil, 2017). This protocol consists of 8 weekly group sessions of 2h duration and the sessions are structured as follows (García-Campayo, Navarro-Gil, & Demarzo, 2016) (Table 6).
ABCT session-by-session for FMS.
| Session | Content |
|---|---|
| 1 | This session is focused on explanations related to the functioning of the brain, the distinction between the concepts of primary and secondary suffering, and the difference between what “compassion” is and is not. Formal practices taught are: Compassionate breathing and compassionate body scan, and Compassionate coping with difficulties. Finally, informal practices are: 3-min compassionate practice; Self-compassion diary; and savoring the moment and giving thanks. |
| 2 | The second session begins by describing the relationship between compassion and mindfulness, the relationship between self-esteem and compassion and fears of compassion. Formal practices taught are: The figure of affect: connecting with basic affection; developing a safe place; compassionate action; and identifying the figure of secure attachment. On the other hand, informal practices taught in this session are: The object that joins us to the world; diary of compassion practice, and What are we good at? |
| 3 | This session deals with the following points: how compassion acts; effectiveness of compassion; and finally, the key point “Self-criticism”. Regarding the formal practices, patients are taught: developing the secure-attachment figure and developing the compassionate voice. “Writing a letter to a compassionate friend” is the informal practice for this session. |
| 4 | Session four explains attachment styles and the importance of these styles in everyday life. The formal practices are: becoming aware of our attachment style and ability to receive affection: friend, indifferent person, enemy. The informal practice recommended in this session is the so-called “Letter to our parents”. |
| 5 | This session is called “working on ourselves” and addresses the importance of developing affection towards ourselves and others. The formal practices are: showing affection to friends and indifferent people; showing affection to ourselves; reconciliation with our parents; and three positive and three negative aspects of our parents. The informal practices are: the greatest display of affection; and the illusion of labels. |
| 6 | In session six, the key elements are guilt and the importance of forgiveness. The formal practices are: forgiving yourself; asking others for forgiveness; forgiving others and showing compassion to enemies; Showing forgiveness for the hurt caused by loved ones; and to finalize a recapitulation of all these practices. Informal practices are: Compassion in everyday life and Interdependence. |
| 7 | This session deals with the following aspects: working in three stages; Envy; Usefulness of being our own attachment figure; and Difficult people. Formal practices are: Working with envy; Becoming our own attachment figure; and Handling difficult relationships. Finally, “Not taking anything personally” and “Looking others in the eye and connecting with their suffering” are the informal practices. |
| 8 | The last session deals with the concept of equanimity and related aspects to learn how to maintain the practice of compassion for a lifetime. The formal practices are: Equanimity (1): We are all equal; Equanimity (II): The illusion of categories; and Equanimity (III): Showing the world the gratitude we have not been able to give back. To conclude the protocol, the informal practices in this last session are: Our values and their relationship with compassion; The cosmic attachment figure; and The tantric embrace. |
The aim of this paper was to review, in a brief and practical way, the six psychological interventions that have been shown to have strong or promising empirical evidence for the management of FMS. It can be asserted that, of all the psychotherapies reviewed, the three therapies that have been listed as empirically supported treatments for chronic pain conditions are CBT, ACT, and the psychoeducational program FibroQoL.
CBT is the most widely-studied psychological therapy in terms of effectiveness for chronic pain conditions such as FMS. It has been considered a treatment with solid empirical evidence for FMS according to the APA and has demonstrated its impact by significantly reducing symptoms associated with FMS (Bernardy, Klose, Welsch, & Häuser, 2017; Clauw, 2014; Hofmann et al., 2012). Regarding ACT, its listing as an empirically supported treatment for ‘Chronic or Persistent Pain in General’ is relatively recent (APA Division 12, 2016b). Although research on its effectiveness in FMS started recently, some well-conducted studies such as that by Luciano, Guallar, et al. (2014) and Luciano, D’Amico, et al. (2014), with a control group and a large sample size, found that ACT produced a significant impact on functional status, pain catastrophizing, quality of life, anxiety and depression. However, more studies with longer follow-ups designed to evaluate ACT effectiveness on FMS to replicate these authors’ results are needed. Similarly, the psychoeducational program FibroQoL has proved to be an effective and cost-effective treatment when compared with treatment as usual (Luciano et al., 2011, 2013).
On the other hand, MBSR, ART, and ABCT have presented promising results in some recent studies although evidence is not as strong as that found for the three other psychotherapies. MBSR, for its part, has been increasingly studied over the last decade, and some randomized clinical trials have shown very positive outcomes for this treatment (Cash et al., 2015; Schmidt et al., 2011; Van Gordon et al., 2017) although its effects on FMS symptomatology have been small according to some reviews (Crowe et al., 2016; Lauche et al., 2013). Thus, further well-designed, large trials are needed to clarify whether MBSR is or is not an effective approach for treatment of FMS. Regarding ART and ABCT, they are both relatively recent psychotherapies which have not yet been widely studied for FMS. Although the results reported to date are promising, further randomized clinical trials with control groups and large sample sizes are required to assess their effectiveness in reducing FMS symptomatology.
From the description of theoretical bases for these 6 psychological therapies, it can be seen that although most of them are addressed to management of chronic pain, they all target distinct psychological processes. However, whether these interventions share mechanisms of change or really have specific, tailored mediating mechanisms is still unknown. Psychological studies generally focus on measuring the effectiveness of their intervention rather than how they exert their effect on the outcome, which may lead to some mistakes, such as targeting the wrong psychological process. To assess how psychological therapies work, research needs to be focused on mediational analysis (Windgassen, Goldsmith, Moss-Morris, & Chalder, 2015). To the best of our knowledge, there are no studies conducting mediational analyses in FMS although some have assessed it in other related conditions such as chronic pain or irritable bowel syndrome, which presents a high prevalence in FMS (63–81%; Kurland, Coyle, Winkler, & Zable, 2006). In this regard, a recent study found that acceptance may have a mediating effect on change in physical functioning in ACT for persons with chronic pain (Cederberg, Cernvall, Dahl, von Essen, & Ljungman, 2016); and a systematic review on the effects of psychological mechanisms of treatment in irritable bowel syndrome found that change in illness-specific cognitions (i.e., chronicity, seriousness, and controllability of the illness; pain-specific catastrophizing or general catastrophizing) is a key process by which psychological treatments (CBT and MBSR) may have an effect on the outcomes of symptom severity and quality of life. However, they did not find changes in perceived stress and in depression to mediate the therapy outcome, suggesting that depression and stress do not necessarily need to be targeted in order to achieve improvement (Windgassen et al., 2017).
In another vein, an aspect of interest which should be studied in the future is the cost-effectiveness of the different psychotherapies; CBT proved to be cost-effective compared with recommended pharmacologic treatments (Luciano, Guallar, et al., 2014; Luciano, D’Amico, et al., 2014). Similarly, the FibroQoL intervention was also significantly more cost-effective than usual treatment for patients with FMS. One study (Kemani et al., 2015) concluded that ACT was more cost-effective than applied relaxation at post-assessment and at 3-month follow-up, but not at 6-month follow-up, and another study conducted in Spain (Luciano et al., 2017) found that ACT was cost-effective when compared to recommended pharmacotherapy, although the sample size was relatively small, which implies that these results must be considered preliminary until further economic evaluations are published. There is some evidence suggesting that MBSR may reduce health costs not only for FMS but also for many other conditions, although these reductions seem to be strongly related to regular practice of mindfulness exercises, as the cost reduction was only observed in the short-term (Knight, Bean, Wilton, & Lin, 2015). There is an ongoing study assessing cost-utility of MBSR in patients with FMS which will shed more light on the issue (Feliu-Soler et al., 2016). To the best of our knowledge, the cost-effectiveness of ART and ABCT has not yet been assessed for any disorder. We consider it would be a really interesting research topic for further studies, along with some comparison of cost-effectiveness of the other four psychotherapies which have already shown better results than recommended pharmacologic treatments and applied relaxation.
In summary, CBT, ACT, and FibroQoL present solid evidence of effectiveness in FMS. Despite having shown positive, promising results, MBSR, ART, and ABCT need more high-quality research to overcome the limitations of the studies conducted to date and to evaluate their effectiveness and cost-effectiveness. From our point of view, mediation and cost-effectiveness analyses are essential for smooth, gradual clinical and research improvement and so there is a pressing need to include these analyses as indispensable when conducting psychological research.
Funding statementThe first author has a FI predoctoral contract awarded by the Agency for Management of University and Research Grants (AGAUR; 2017; FI_B 00754). The ninth author has a Sara Borrell contract and the last author has a Miguel Servet contract awarded both by the Institute of Health Carlos III (ISCIII; CD16/00147 and CP14/00087, respectively). We are also grateful to the Network for Prevention and Health Promotion in Primary Care funded by the ISCIII (RD16/0007/0005 & RD16/0007/0012). The funding bodies did not have any role in the collection, analysis and interpretation of data; in the writing of the report; and in the decision to submit the article for publication.