Rhombencephalosynapsis (RES) is a rare posterior fossa malformation first described in 1914 by Obersteiner1 in a post mortem study of a 28-year-old man. The term RES was coined by Gross2 and Hoff in 1959. The entity is characterised by aplasia or hypoplasia of the cerebellar vermis, associated with midline fusion of the cerebellar hemispheres.3,4 RES may be associated with other malformations of the central nervous system and other structures.3,5 Diagnosis of this rare condition in adulthood is extremely infrequent, with very few cases reported to date.6–9
We present a case of late diagnosis of paucisymptomatic RES.
Our patient was a 43-year-old man, a former smoker with history of repeated syncope, with no known structural heart disease. He visited our hospital’s emergency department due to paraesthesia in the face and the left crural region associated with headache in the context of a hypertensive crisis. The neurological examination revealed tactile hypoaesthesia and hypoalgesia in the aforementioned location, with no alterations in muscle strength, language comprehension and production, or cranial nerve function, and no limb dysmetria. The patient remained asymptomatic after blood pressure was controlled. CT, blood and urine analyses, and ECG yielded normal results, with no signs of haemodynamically significant stenosis in the duplex ultrasound of the supra-aortic trunks.
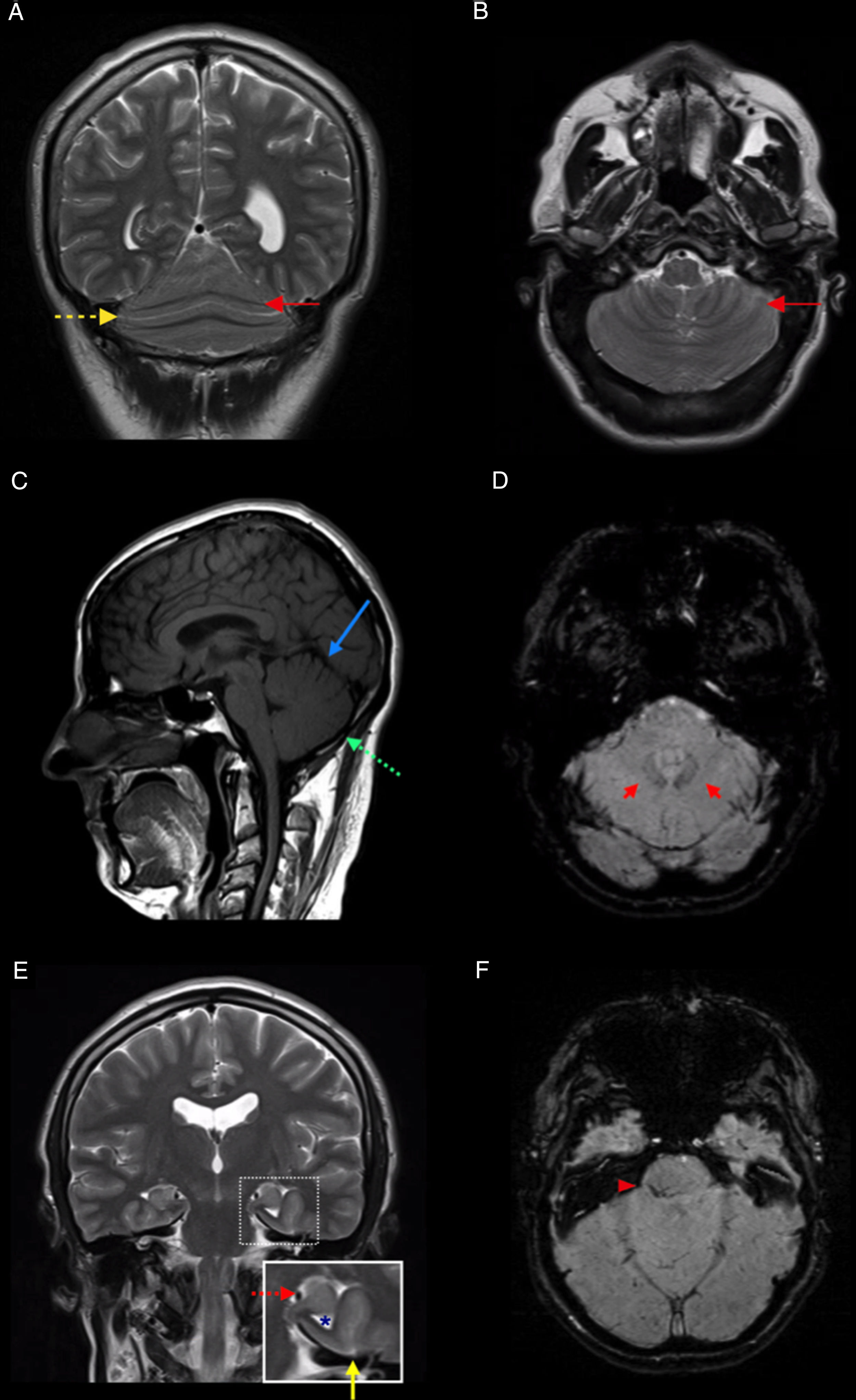
An MRI study revealed partial agenesis of the cerebellar vermis with partial posterior fusion of the cerebellar hemispheres (Fig. 1A and B), absence of the primary and prepyramidal fissures of the cerebellum (Fig. 1C), proximity of the dentate nuclei to the midline (Fig. 1D), left-sided incomplete hippocampal inversion associated with colpocephaly (Fig. 1E), and capillary telangiectasia in the right middle cerebellar peduncle (Fig. 1F).
MRI study of our patient. A and B) Coronal and axial T2-weighted sequences, showing partial fusion of the cerebellar hemispheres and continuity of the folia (solid red arrow) and fissures (dashed yellow arrow) across the midline. C) Sagittal T1-weighted sequence showing absence of the primary (solid blue arrow) and prepyramidal fissures (dashed green arrow). D) Axial SWI sequence showing proximity of the dentate nuclei to the midline (red arrows). E) Coronal T2-weighted sequence showing left-sided incomplete hippocampal inversion (dashed red arrow), associated with vertical orientation of the collateral sulcus (solid yellow arrow) and dilation of the ipsilateral temporal horn (asterisk). F) Axial SWI sequence showing capillary telangiectasia in the right middle cerebellar peduncle.
A subsequent examination only revealed severe difficulty walking in tandem. In a targeted medical history interview, the patient reported a long history of gait instability, presenting only when performing certain activities.
Diagnosis of RES is based on brain MRI findings and correct interpretation of clinical signs and symptoms, particularly in more subtle cases with partial RES. The main radiological finding for diagnosis is aplasia or hypoplasia of the cerebellar vermis, associated with midline fusion of the cerebellar hemispheres.3,4 Other diagnostic findings include hydrocephalus or ventriculomegaly (which may be associated with aqueductal stenosis),9 corpus callosum abnormalities (hypoplasia), and absent septum pellucidum.4 The literature also includes reports of other abnormalities associated with RES: fusion of the thalamus, tectum, and fornices; temporal lobe hypoplasia; incomplete hippocampal inversion10; and hypoplasia of the optic chiasm, olivary nuclei, and anterior comissure.11–13 Other noteworthy neuroradiological findings include: 1) on sagittal images: absence of the primary fissure (Fig. 1C), abnormal (rounded) morphology of the fourth ventricle, and deficient indentation of the fourth ventricle by the nodulus; and 2) on axial and coronal images: continuity of the cerebellar folia and fissures across the midline (Fig. 1A and B) and fusion/apposition of the superior cerebellar peduncles and the dentate nuclei (Fig. 1D).3
Over 150 cases of RES have been reported in the literature.14 RES frequently co-presents with a wide range of syndromes, including Gómez-López-Hernández syndrome15 (the most frequent) and VACTERL association.16,17
Although multiple cases suggest that RES has a genetic basis, the precise cause has not been identified.14
Few cases have been reported of RES diagnosed in adulthood, with our patient being one of the oldest in the literature.6–9 Clinical presentation and prognosis of RES are extremely variable, and usually depend on the associated supratentorial abnormalities; however, cases have been reported of patients who only display mild gait alterations.7,18 Therefore, despite its low prevalence, RES should be included in the differential diagnosis of ataxia in adults.
Please cite this article as: Sánchez-Villalobos JM, Torres-Perales AM, Serrano-Velasco L, Pérez-Vicente JA. Romboencefalosinapsis en el adulto: una presentación inusual de una entidad poco frecuente. Neurología. 2021;36:628–630.