Despite comprehensive study, the aetiology of stroke is not identified in 35% of cases.
AimsWe conducted a study to assess the diagnostic capacity of N-terminal pro-B-type natriuretic peptide (NT-proBNP) in the identification of ischaemic stroke of cardioembolic origin. The secondary purpose of the study was to evaluate the prognostic value of NT-proBNP for predicting 90-day all-cause mortality.
MethodsWe designed a prospective observational study including patients hospitalised due to stroke between March 2019 and March 2020. Blood samples were collected on admission to the emergency department and serum NT-proBNP levels were determined. Statistical analysis was performed using a bivariate logistic regression model and receiver operating characteristic (ROC) and Kaplan–Meier curves. Statistical significance was established at p<.05.
ResultsThe study included 207 patients with first ischaemic stroke. Plasma NT-proBNP levels were significantly higher (p<.001) in the cardioembolic stroke group (2069pg/mL±488.5). ROC curves showed that NT-proBNP>499pg/mL was the optimum value for diagnosing cardioembolic ischaemic stroke (sensitivity, 82%; specificity, 80%). Moreover, plasma NT-proBNP levels>499pg/mL were independently associated with cardioembolic stroke (OR: 9.881; p=.001). Finally, NT-proBNP>1500pg/mL was useful for predicting 90-day mortality (sensitivity, 70%; specificity, 93%).
ConclusionsNT-proBNP was independently associated with cardioembolic stroke and should be quantified in blood tests within 24h of stroke onset. High plasma levels (>499pg/mL) may indicate an underlying cardioembolic cause, which should be further studied, while NT-proBNP >1500pg/mL was associated with increased 90-day mortality.
A pesar de un completo y exhaustivo estudio, la etiología de un 35% de los ictus isquémicos es desconocida.
ObjetivosEvaluar la capacidad de diagnóstico del NT-proBNP en la identificación del ictus isquémico de origen cardioembólico. El objetivo secundario fue evaluar el valor pronóstico del NT-proBNP como predictor de mortalidad de cualquier causa tras 90 días del ictus.
MétodosDiseñamos un estudio observacional prospectivo, incluyendo pacientes hospitalizados por ictus. El periodo de reclutamiento fue de marzo de 2019 a marzo de 2020. Se obtuvieron muestras de sangre a su admisión en Urgencias y se midieron los niveles plasmáticos de NT-proBNP. El análisis estadístico fue realizado mediante un modelo bivariado de regresión logística, curva de la característica operativa del receptor (curvas ROC) y curvas Kaplan-Meier. Se consideraron significativas diferencias con p < 0,05.
ResultadosFueron incluidos 207 pacientes con un primer episodio de ictus isquémico agudo. Los niveles de NT-proBNP fueron significativamente mayores (p < 0,001) en el grupo de ictus isquémico cardioembólico (2.069 ± 488,5). Las curvas ROC mostraron que un NT-proBNP > 499 pg/mL es el valor óptimo para el diagnóstico de ictus isquémico cardioembólico (sensibilidad 82%, especificidad 80%). Además, los niveles plasmáticos de NT-proBNP > 499 pg/mL estaban asociados de forma independiente con el ictus isquémico cardioembólico (OR = 9.881, p = 0,001). Finalmente, un valor de NT-proBNP > 1.500 pg/mL fue útil para predecir la mortalidad de cualquier causa 90 días tras el ictus isquémico (sensibilidad = 70%, especificidad = 93%).
ConclusionesEl valor de NT-proBNP estaba asociado independientemente al ictus isquémico de origen cardioembólico y debería ser considerado su análisis en las primeras 24 h desde el inicio del ictus. Niveles elevados (NT-proBNP > 499 pg/mL) pueden indicar un origen cardioembólico subyacente, el cual debería ser estudiado con mayor detalle, mientras que niveles de NT-proBNP > 1.500 pg/mL se asociaron con un incremento de la mortalidad a los 90 días del ictus.
Stroke is the most frequent cause of permanent disability in adulthood and one of the leading causes of death in Spain and worldwide.1,2 In particular, the incidence of stroke is 187/100,000 inhabitants in Spain.3,4
The diagnosis of stroke is more difficult in the first hours, mainly if the onset is unknown, the signs are atypical, the patient is agitated and access to the image is delayed. Etiologically, ischaemic stroke is classified according to different classification systems such as the TOAST classification5 the ASCOD phenotyping system6 and the Causal System classification.7 All of them recognize the existence of ischaemic stroke of cardioembolic origin. Cardioembolic stroke has been associated with highest in-hospital mortality during the acute phase of stroke, higher rates of disability, neurological impairment, recurrence and worse prognosis.8 For these reasons, its diagnosis is of great importance for adequate treatment and correct secondary prevention. Despite a complete and exhaustive study, the origin of 35% of strokes is undetermined.9 In many of these cases, as well as in strokes of cardioembolic origin, the presence of a paroxysmal atrial fibrillation (AF) arrhythmia is the triggering cause of the episode.10 In this regard; cardiac blood biomarkers represent an objective measurement of molecular characteristics which may help in the diagnosis.
The N-terminal pro-type-B natriuretic peptide (NT-proBNP) is the proBNP's inactive residue released from the heart's left ventricle in response to wall stress through volume expansion and increased pressure.11 Its levels increase with heart failure, myocardial infarctions, atrial fibrillation and are higher in women and elderly.12 In the last few years, NT-proBNP emerged as a serum biomarker in stroke. A recent meta-analysis with data from 2834 patients demonstrated that natriuretic peptides are strongly increased in cardioembolic strokes.13 Nonetheless, a cut-off value was not obtained. Only few small studies showed different NT-proBNP cut-off values (>200pg/mL, >265.5pg/mL and >313pg/mL) to be associated with cardioembolic stroke.14–16 Furthermore, nautriuretic peptides have been found to correlate with stroke severity and mortality.17
Therefore, the primary aim of the present study was to assess the diagnostic ability of NT-proBNP for the identification of ischaemic stroke of cardioembolic origin. The secondary purpose was to evaluate the prognostic value of NT-proBNP for predicting 90-days all-cause mortality.
MethodsStudy design and clinical protocolThis is a prospective observational study including adult patients hospitalized by stroke at the Santa Lucia University Hospital from Cartagena, Spain; and designed following the STARD guidelines.18 The recruitment period was from March 1, 2019 to March 1, 2020. All adult patients (≥18 years) with clinically suspected stroke in Emergency Department were eligible for the study. Exclusion criteria were: presence of (a) solid tumours or lymphomas; (b) chronic and acute heart failure; (c) haemorrhagic stroke; (d) brain bleeding secondary to amyloid congophyl angiopathy, aneurysms, subarachnoid haemorrhage; (e) concomitant infections; (f) other complications such as epileptic seizures or acute myocardial infarction and (g) lack of analytical/clinical data.
Stroke diagnosis was performed by trained neurologists according to the World Health Organization definition19 and confirmed by neuroimaging. Symptoms severity was assessed by using the National Institutes of Health20 and the following variables related to the stroke were collected: systolic and diastolic blood pressure, glucose, LDL-cholesterol and creatinine. Stroke acute treatment and its secondary prevention treatment were carried out by neurologists following approved clinical guidelines21–24 but not any specific treatment or intervention for this study. Patients’ medical history was reviewed and collected the following covariates: high blood pressure, diabetes, dyslipidemia, atrial fibrillation, cardiac valvulopathy or shunt, chronic kidney disease, previous stroke, tobacco and alcohol consume, anticoagulants and antiplatelets intake.
Blood sampling and laboratory methodsBlood samples were collected by venipuncture into tubes with separator gel (BD Vacutainer SST II Advance 8.5mL) within the first 24h of admission. Tubes were immediately centrifuged (3500rpm for 10min at room temperature) and separated serum was used for the immediate measurement of NT-proBNP, the results of which were not reported to the attending physicians.
Serum NT-proBNP levels were measured on a Cobas e702 analyzer (Roche Diagnostics, Mannheim, Germany) by an electrochemiluminescence immunoassay (ECLIA). According to manufacturer's data, detection limit, functional sensitivity and measurement range were 10pg/mL, 50pg/mL and 10–35,000pg/mL, respectively.
Statistical analysisContinuous variables were tested for normal distribution using the Kolmogorov–Smirnov's test. Data are summarized as numbers and frequencies for categorical variables and medians with interquartile ranges (IQRs) for continuous data. Comparisons between groups were performed with Chi-squared test for categorical data and Mann–Whitney U and Kruskal–Wallis for continuous data.
For the first purpose, discriminatory ability of NT-proBNP for cardioembolic stroke was evaluated by calculating the area under the receiver operating characteristic curve (AUC-ROC) and we additionally calculated the optimal ROC-derived cutoff value according to Youden Index. Binary logistic regression was performed to identify variables associated with cardioembolic stroke. To achieve the best set of predictors, only variables with a statistical trend in univariate analysis (p<0.10) were selected for multivariate analysis. Covariates were retained in the final model if they were statistical significant with a p-value of <0.05.
For the second purpose, ROC analysis with calculation of the AUC was performed to evaluate the utility of NT-proBNP for prognosis of all-cause mortality in all patients after 90 days. We identified independent predictors for 90-day mortality by Cox regression analysis and Kaplan–Meier survival curves, according to NT-proBNP quartiles, were constructed for comparison among survivors and non-survivors
We performed analyses by using the software packages SPSS 21.0 (SPSS Inc., IL, USA) and MedCalc 15.0 (MedCalc Software, Ostend, Belgium). In all tests, a two-sided p-value of <0.05 was considered significant.
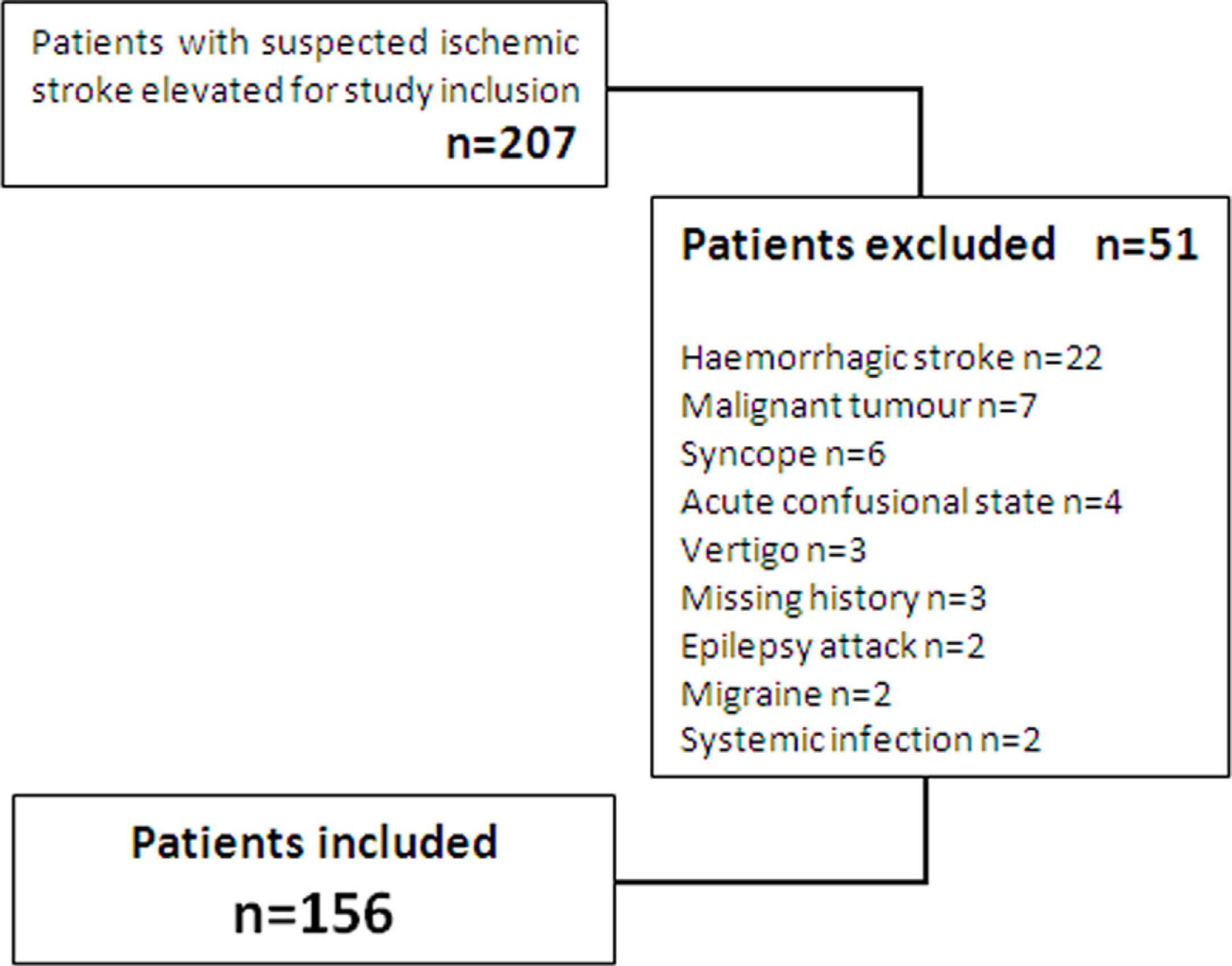
ResultsIn the study period, 207 consecutive patients with a suspected stroke at the time of first medical evaluation were recruited. After exclusion criteria were applied, 156 patients (72 women, 84 men; mean age: 69.3±0.9) were finally included, as showed in the study's protocol flowchart (Fig. 1).
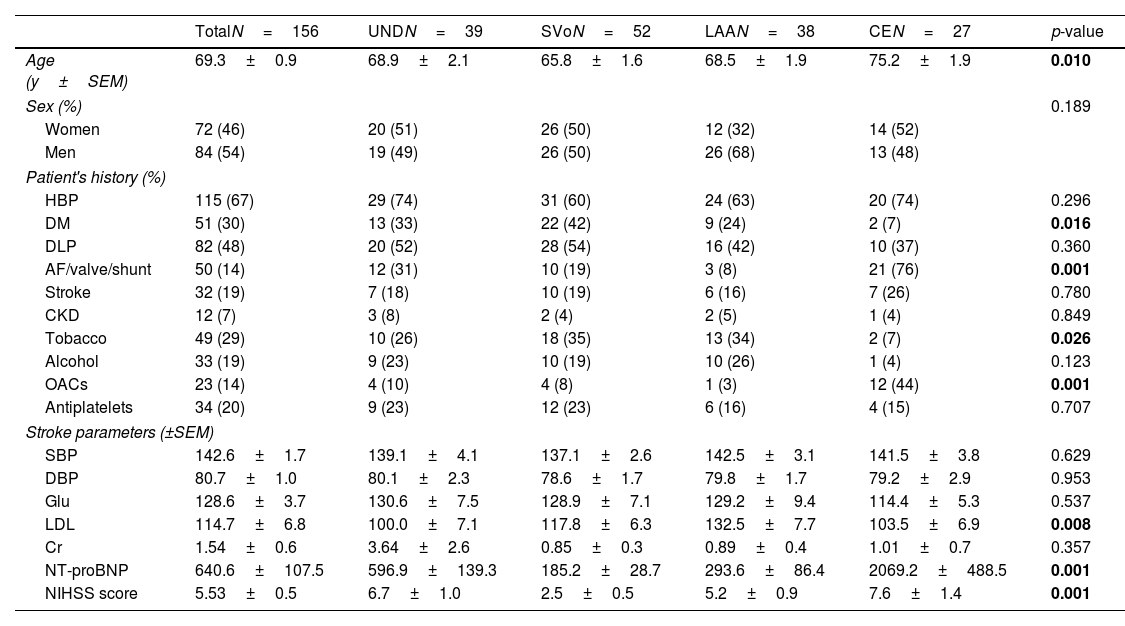
Baseline characteristics are shown in Table 1. Patients diagnosed with cardioembolic stroke were significantly older (75.2±1.9; p=0.010) and associated higher rates of atrial fibrillation/shunt or cardiac valvulopathy (76%; p=0.001) and oral anticoagulants intake (44%; p=0.001) versus other stroke groups. In contrast, the prevalence of smokers were significantly lower in the cardioembolic group (7%; p=0.026). Finally, plasma LDL-cholesterol values were significantly higher (132.5±7.7; p=0.008) in the large-vessel stroke group and the NIHSS score were significantly lower in the small vessel group (2.5±0.5; p<0.001).
Patients’ history and stroke related clinical parameters.
| TotalN=156 | UNDN=39 | SVoN=52 | LAAN=38 | CEN=27 | p-value | |
|---|---|---|---|---|---|---|
| Age (y±SEM) | 69.3±0.9 | 68.9±2.1 | 65.8±1.6 | 68.5±1.9 | 75.2±1.9 | 0.010 |
| Sex (%) | 0.189 | |||||
| Women | 72 (46) | 20 (51) | 26 (50) | 12 (32) | 14 (52) | |
| Men | 84 (54) | 19 (49) | 26 (50) | 26 (68) | 13 (48) | |
| Patient's history (%) | ||||||
| HBP | 115 (67) | 29 (74) | 31 (60) | 24 (63) | 20 (74) | 0.296 |
| DM | 51 (30) | 13 (33) | 22 (42) | 9 (24) | 2 (7) | 0.016 |
| DLP | 82 (48) | 20 (52) | 28 (54) | 16 (42) | 10 (37) | 0.360 |
| AF/valve/shunt | 50 (14) | 12 (31) | 10 (19) | 3 (8) | 21 (76) | 0.001 |
| Stroke | 32 (19) | 7 (18) | 10 (19) | 6 (16) | 7 (26) | 0.780 |
| CKD | 12 (7) | 3 (8) | 2 (4) | 2 (5) | 1 (4) | 0.849 |
| Tobacco | 49 (29) | 10 (26) | 18 (35) | 13 (34) | 2 (7) | 0.026 |
| Alcohol | 33 (19) | 9 (23) | 10 (19) | 10 (26) | 1 (4) | 0.123 |
| OACs | 23 (14) | 4 (10) | 4 (8) | 1 (3) | 12 (44) | 0.001 |
| Antiplatelets | 34 (20) | 9 (23) | 12 (23) | 6 (16) | 4 (15) | 0.707 |
| Stroke parameters (±SEM) | ||||||
| SBP | 142.6±1.7 | 139.1±4.1 | 137.1±2.6 | 142.5±3.1 | 141.5±3.8 | 0.629 |
| DBP | 80.7±1.0 | 80.1±2.3 | 78.6±1.7 | 79.8±1.7 | 79.2±2.9 | 0.953 |
| Glu | 128.6±3.7 | 130.6±7.5 | 128.9±7.1 | 129.2±9.4 | 114.4±5.3 | 0.537 |
| LDL | 114.7±6.8 | 100.0±7.1 | 117.8±6.3 | 132.5±7.7 | 103.5±6.9 | 0.008 |
| Cr | 1.54±0.6 | 3.64±2.6 | 0.85±0.3 | 0.89±0.4 | 1.01±0.7 | 0.357 |
| NT-proBNP | 640.6±107.5 | 596.9±139.3 | 185.2±28.7 | 293.6±86.4 | 2069.2±488.5 | 0.001 |
| NIHSS score | 5.53±0.5 | 6.7±1.0 | 2.5±0.5 | 5.2±0.9 | 7.6±1.4 | 0.001 |
Abv: UND=undetermined; SVo=small vessel disease; LAA=large artery atherothrombosis; CE=cardioembolic; y=years; HBP=high blood pressure; DM=diabetes mellitus; DLP=dyslipidemia; AF=atrial fibrillation; CKD=chronic kidney disease; OACs=oral anticoagulants; SBP=systolic blood pressure; DBP=diastolic blood pressure; Glu=glucose; LDL=low density lipoprotein; Cr=creatinin; NT-proBNP=N-terminal-pro brain derived natriuretic Peptide; NIHSS=national institute health stroke scale.
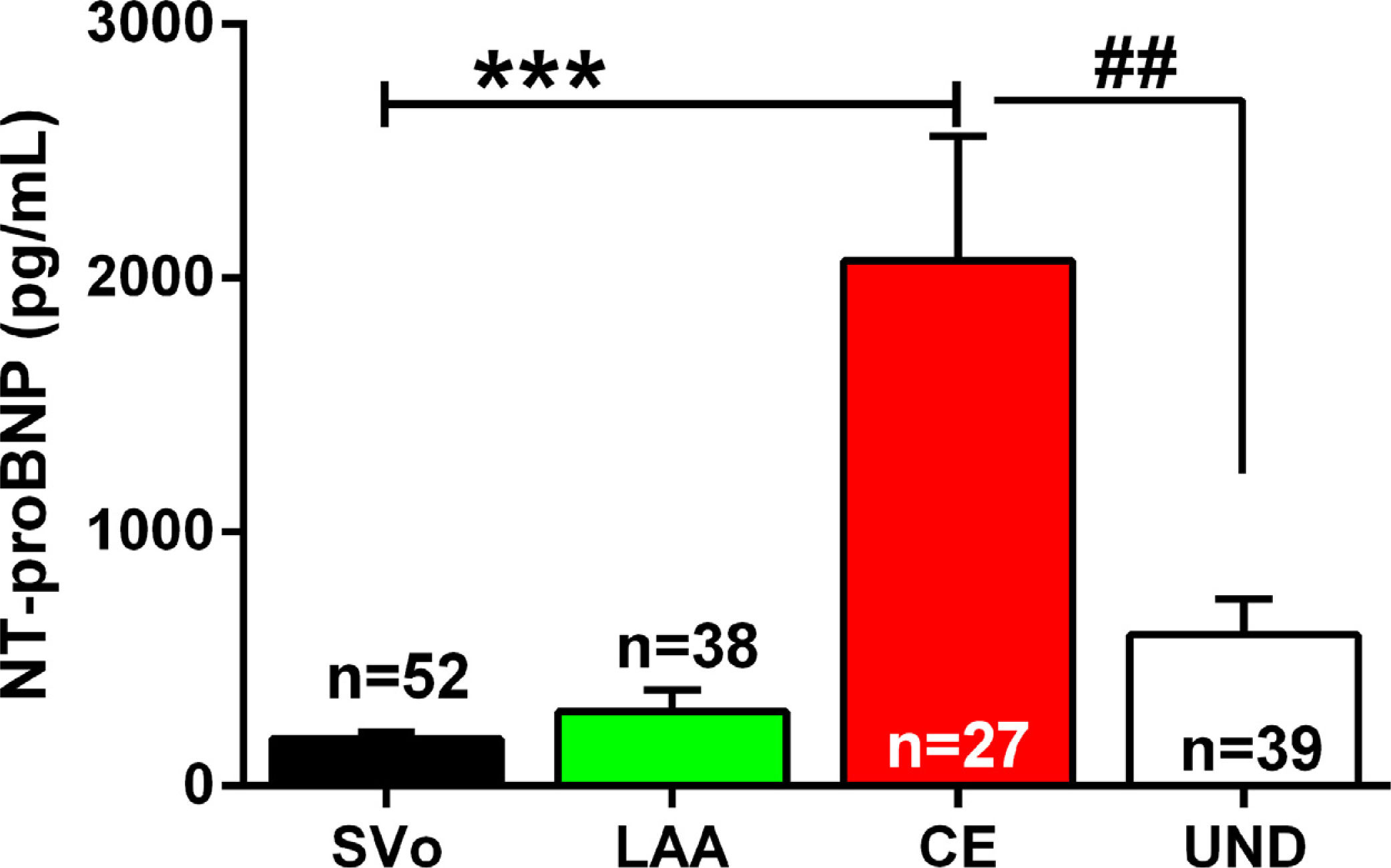
We compared the plasma levels of NT-proBNP in each group of stroke by TOAST classification: small vessel disease stroke (SVo), large artery atherothrombosis stroke (LAA), cardioembolic stroke (CE) and stroke of undetermined cause (UND). As shown in Fig. 2, Kruskal–Wallis revealed a significant increased NT-proBNP plasma levels in the cardioembolic stroke group (2069±488.5) versus the large vessel (293.6±86.35; ***p=0.0001), small vessel (185.2±28.66; ***p=0.0001) and undetermined (596.9±139.3; ##p=0.0088) stroke groups.
N-terminal pro-brain natriuretic peptide (NT-proBNP) plasma levels by ischaemic stroke sub-type. Data are expressed as the mean±SEM. Kruskal–Wallis test: ***p<0.001 vs. SVo and LAA; ## vs. UND stroke. Abv: SVo=small vessel occlusion stroke (n=52); LAA=large artery atherosclerosis stroke (n=38); CE=cardioembolic stroke (n=27); UND=undetermined aetiology stroke (n=39); NT-proBNP=N-terminal pro-brain natriuretic peptide.
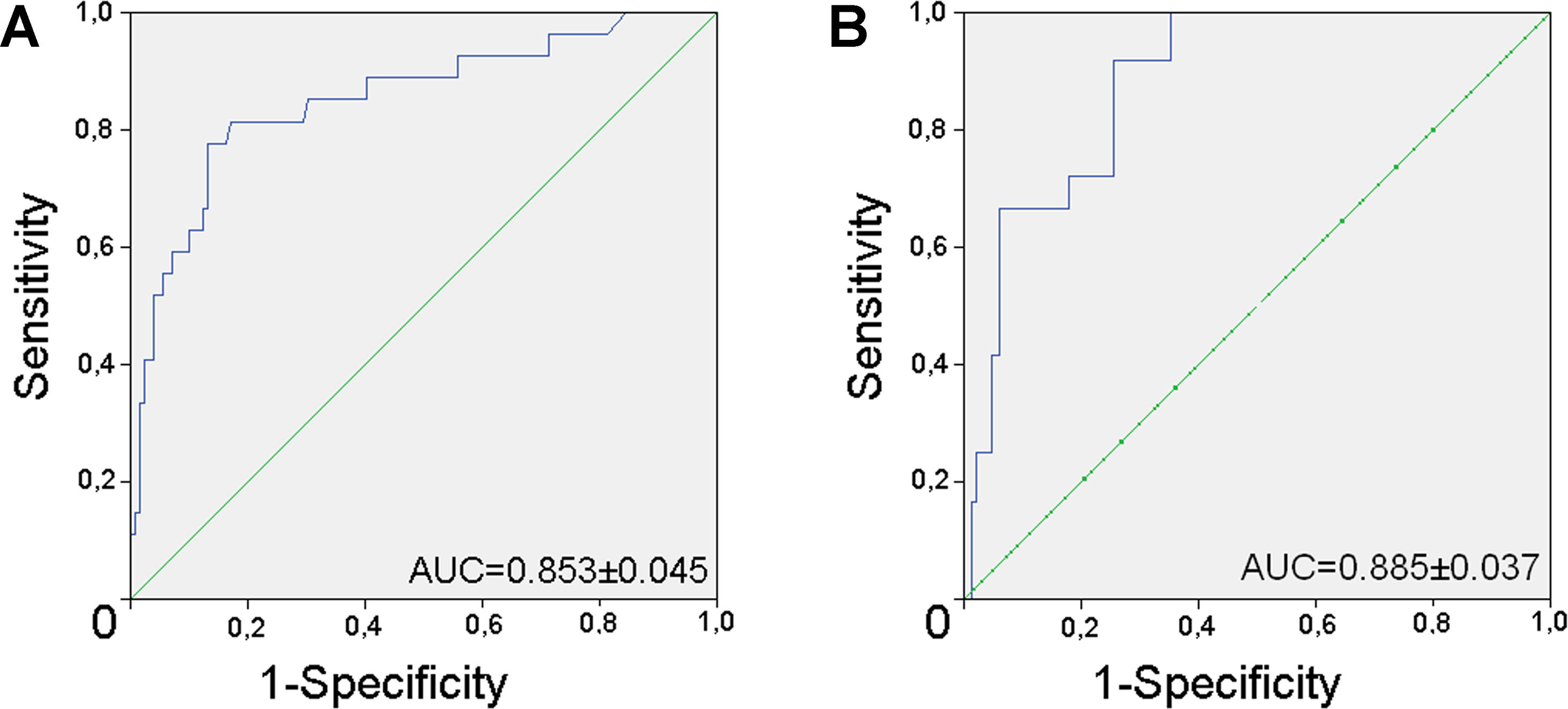
In supplementary material (A) is shown the area under the receiver operating characteristics curve (ROC) of NT-proBNP for diagnosis of cardioembolic stroke which was 0.853 (CI95%=0.766–0.941; p<0.001). As shown in Table 2, Youden index indicated that the optimal cut-off value of NT-proBNP was 499pg/mL (sensitivity 82%, specificity 80%).
NT-proBNP and cardioembolic strokeA logistic bivariate regression analysis was used to truly establish the parameters independently associated with cardioembolic stroke. As shown in Table 3, bivariate logistic regression analysis showed that NT-proBNP plasma levels were independently associated to cardioembolic stroke (OR=1.01, CI95%=1.00–1.02, p<0.003). Furthermore, bivariate logistic regression analysis showed that NT-proBNP>499pg/mL were independently associated to cardioembolic stroke (OR=9.881, CI95%=2.831–34.489, p=0.001).
Non-cardioembolic vs. cardioembolic stroke by bivariate logistic regression model.
| OR | IC95% | p-Value | |
|---|---|---|---|
| Age | 0.999 | 0.949–1.055 | 0.986 |
| DM | 4.550 | 0.870–23.683 | 0.072 |
| AF/valve/shunt | 0.395 | 0.126–1.237 | 0.111 |
| Tobacco | 5.866 | 0.598–57.575 | 0.129 |
| LDL | 0.998 | 0.985–1.011 | 0.768 |
| NT-proBNP | 1.001 | 1.000–1.002 | 0.003 |
| NT-proBNP>499 | 9.881 | 2.831–34.489 | 0.001 |
Abv: DM=diabetes mellitus; AF=atrial fibrillation; LDL=low density lipoprotein; NT-proBNP=N-terminal-pro brain derived natriuretic peptide.
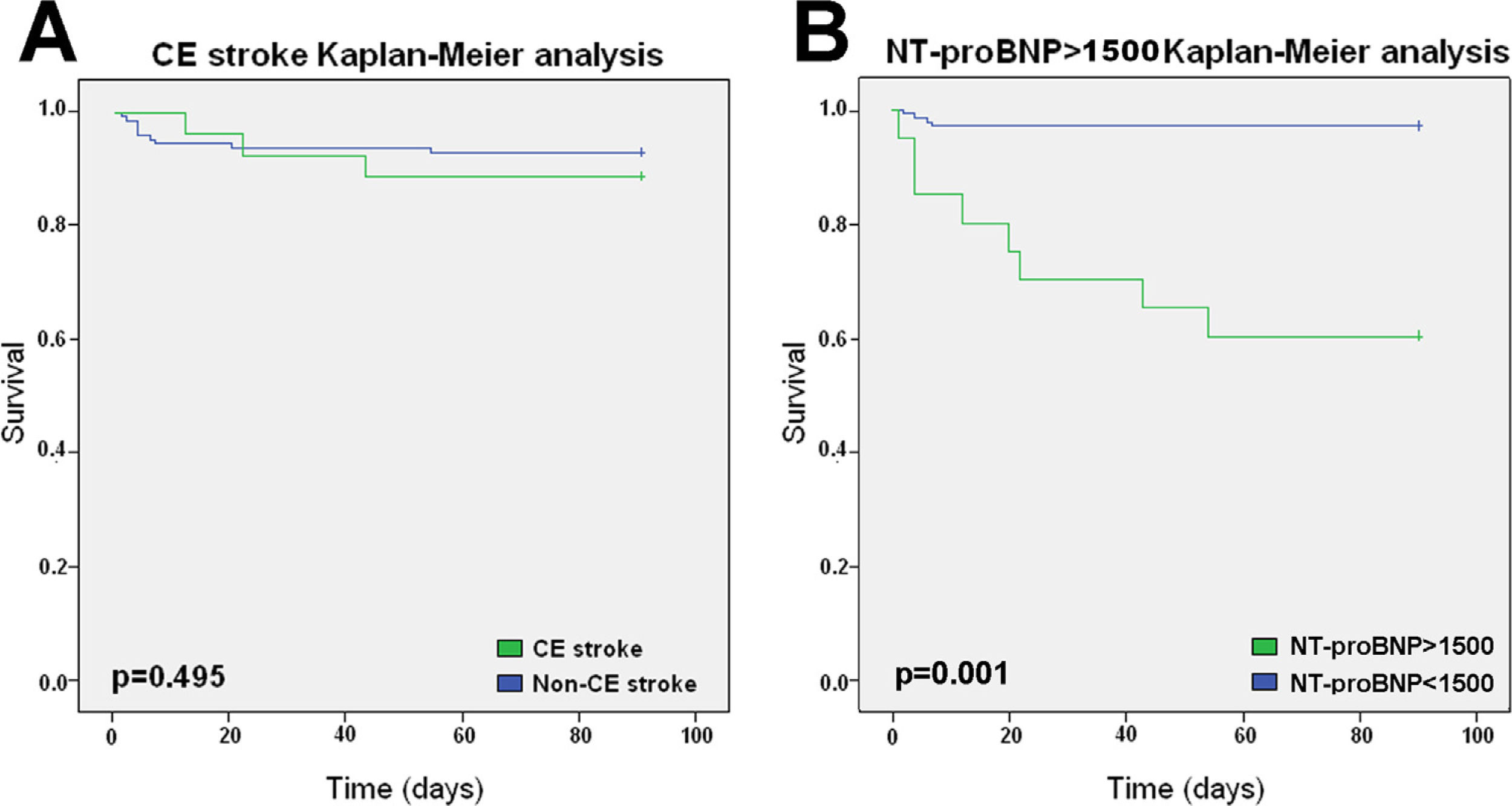
We examined the survival at 90 days in both, cardioembolic and no-cardioembolic stroke (Fig. 3A). Log rank (Mantel–Cox) showed no statistical differences (p=0.495) between cardioembolic (n=3; 17.15%, CI95%=9.35–24.6) and no-cardioembolic (n=9; 15.49%, CI95%=11.95–19.02) stroke in death, by all causes, at 90 days. Furthermore, we first obtained a NT-proBNP>1500pg/mL cut-off value (COR curve: AUC=0.885, CI95%=0.81–0.96%; p=0.001; sensitivity=70%, specificity=93%) to predict mortality at 90 days post-stroke (see supplementary material). Secondly we examined the prognostic value of a NT-proBNP>1500pg/mL. Kaplan–Meier analysis (Fig. 3B) revealed that NT-proBNP>1500pg/mL were found to significantly (p=0.001) increase the mortality at 90 days (38.0%, CI95%=32.2–53.8) after stroke versus lower plasma levels (12.5%, CI95%=10.19–14.93). In this regard, 8 of 12 deaths were in patients with NT-proBNP>1500pg/mL. In this subgroup of patients, 7 deaths were directly attributed to stroke severity and 1 was caused by traumatic car accident. The causes of death in the 4 patients with NT-proBNP<1500pg/mL were (all after hospital discharge): 2 sepsis, 1 heart attack and 1 intestinal haemorrhage in a patient anticoagulated by femoral artery occlusion.
Kaplan–Meier survival curves at 90 days. (A) Kaplan–Meier curves comparing survival between cardioembolic and non-cardioembolic stroke groups. (B) Kaplan–Meier curves comparing survival of patients with a NT-proBNP>1500pg/mL. The p values were obtained from the log rank tests. Abv: CE=cardioembolic stroke, NT-proBNP=N-terminal pro-brain natriuretic peptide.
Our results showed that NT-proBNP>499pg/mL was useful to predict cardioembolic stroke (sensitivity 82%, specificity 80%). In the last few years, different studies assessed an optimal cut-off value for discriminating the presence of a cardioembolic source. For example, Zecca et al.14 showed a level of NT-proBNP>200pg/mL and calculated a 65% sensitivity and 82% specificity 0.82 while Hajsadeghi et al.25 showed a cut-off value>342pg/mL (93% sensitivity, 73% specificity). A recent study showed that NT-proBNP≥505pg/mL distinguished AF-related from noncardiac stroke with a sensitivity of 93% and a specificity of 72%.26 Interestingly, cut-off value of NT-proBNP has been shown not only within 24h of stroke but also 7 and 90 days after (NT-proBNP>313; >181 and >174pg/mL, respectively).16 Future research and meta-analysis are needed to establish a common, accurate and reliable NT-proBNP's cut-off value.
NT-proBNP and cardioembolic strokeOur results demonstrated that NT-proBNP plasma levels were higher and independently associated to cardioembolic stroke. A large-scale European prospective study showed that levels of NT-proBNP are positively associated with ischaemic stroke, independently from several other risk factors.27 In this line, a prospective study using the ARIC cohort demonstrated an association between NT-proBNP plasma levels and cardioembolic stroke but not with lacunar or haemorrhagic stroke.28 Furthermore, a recent prospective study showed that patients with cardioembolic stroke had higher NT-proBNP.26 Finally, a recent meta-analysis showed that both, BNP and NT-proBNP display closely equivalent diagnostic accuracies in distinguishing cardioembolic ischaemic stroke from non-cardioembolic, with NT-proBNP showing a superior specificity.29 Altogether, these results suggest that NT-proBNP could be a useful biomarker of cardioembolic stroke and therefore may help clinicians to select patients for further etiologic study with subcutaneous Holter monitor. Further research is needed to rule out the impact of NT-proBNP in the etiologic study in patients with undetermined cause of stroke.
Stroke aetiology, NT-proBNP and mortalityOur results demonstrated no differences in mortality within stroke sub-types while a NT-proBNP>1500pg/mL showed increased mortality after 90days post-stroke. Mortality of ischaemic stroke has been widely studied in long-term. Nonetheless, short-term mortality has been scarcely studied and is about 8% after 30 days.30 According to previous studies31 we found no differences in mortality between cardioembolic and no-cardioembolic stroke, by all causes, up-to 90 days. Nonetheless, that study showed an increased mortality in cardioembolic stroke group after 1 and 5 years. Moreover, Bjerkreima et al.32 showed cardioembolic stroke had a 34% higher risk of death within 5 years while small vessel occlusion had a 48% lower risk of death. In this regard, the risk of recurrent stroke is increased in cardioembolic stroke and, as previously shown; stroke recurrence may be associated with increased inhospital mortality.33
Altogether, our data support previous findings indicating no differences in short-term mortality between subtypes of ischaemic stroke. In addition, recent evidence suggests that plasma levels of natriuretic peptides might be related to mortality after stroke. In particular, high BNP levels (>500pmol/L) have been shown to be an independent prognostic value for mortality after stroke.34 A meta-analysis showed that high NT-proBNP plasma levels (>1453pg/mL) were independently associated to mortality post-stroke with no differences between stroke sub-type. Furthermore, this study demonstrated that NT-proBNP had an added value (discrete) respect to simple clinical variables in ranking patients at high risk of death after stroke.17 As suggested by Jickling and Foerch35 the ability of NT-proBNP to predict mortality after stroke may relate to disease other than stroke. As previously showed, NT-proBNP is an independent predictor of mortality in cardiac dysfunction, in kidney disease,36 diabetes37 and cardiac surgery.38 Nonetheless, a NT-proBNP>1500pg/mL value could be useful for clinicians to inform patients’ family about a poor prognosis at 90 days. Further research is needed to assess the specific management and better treatment in that group of patients with worse prognosis after stroke.
ConclusionsIn summary, our results demonstrated that NT-proBNP>499pg/mL plasma levels may indicate an underlying cardiac cause which should be further studied. Furthermore, despite cardioembolic ischaemic stroke being not associated with higher mortality after 90 days; NT-proBNP>1500pg/mL plasma levels are associated with increased mortality. Therefore, NT-proBNP should be considered for blood testing within 24h of stroke.
LimitsThis study has several limitations that must be pointed out. First, we excluded patients with conditions which are able to enhance NT-proBNP plasma levels such as sepsis, malignant tumours, chronic or acute heart failure and haemorrhagic stroke. We excluded haemorrhagic stroke patients because a CT scan is mandatory in the diagnosis of acute stroke and then, the differential diagnosis between ischaemic and haemorrhagic stroke is done. For the same reason, we found low mortality rates; therefore the results for mortality prediction should be interpreted with caution.
Secondly, although the NT-proBNP value is measured upon arrival at the hospital, the time from the onset of the stroke to the arrival of the patient is variable due to various causes such as the distance to the hospital or the underestimation of the symptoms by the patient or even an incorrect initial diagnosis. Nonetheless, hospital admission is an easily reproducible clinical time point, increasing the external validity of our study and facilitating the replication of our results in clinical practice.
ContributorshipECG, DVM, VRA, MGM and JAGC collected data. JAGC, JAPV, LGGR, JJST, CSVB researched literature and designed the study. JAGC, LGGR were involved in protocol development, gaining ethical approval and data analysis. JAGC and LGGR wrote the first draft of the manuscript. All authors reviewed and edited the manuscript and approved the final version of the manuscript.
Ethical approvalThe study was performed according to the Declaration of Helsinki and approved by the Research Ethic Committee of the Murcia Health Service (E.O. 2020-37 BNPCS2020-01). No identifiable information was retained or is presented in this manuscript.
Informed consentInformed consent was not required for the present study because no additional blood tests were needed as recognized by the Ethical Committee.
GuarantorNot applicable.
FundingThe authors neither received public or private funding nor grant to carry out this study.
Conflict of interestsThe Authors declare that there is no conflict of interest.
Not reported.