Subarachnoid haemorrhage (SAH) associated with vitreous haemorrhage was first described by French ophthalmologist Albert Terson in 1900.1–3 At present, any type of intracranial haemorrhage2 accompanied by vitreous haemorrhage is known as Terson syndrome (TS). SAH generally occurs as a result of a ruptured cerebral aneurysm. It is relatively frequent, with an incidence accounting for 5% of all cases of cerebral vascular disease. In contrast, TS is exceptional. The mechanism by which SAH causes intraocular bleeding is a matter of debate.1–3 A number of theories state that by means of a direct mechanism, blood is forced through the stem of the optic nerve and into the globe while the SAH is occurring.1,3 Other authors suggest that vitreous haemorrhage is the result of venous hypertension and disruption of retinal vessels.3
In TS, most subarachnoid haemorrhages are caused by spontaneous rupture of an aneurysm. The 3 most common locations are the intracranial internal carotid artery, the bifurcation of the middle cerebral artery, and the superior part of the basilar artery. The anatomical location of the aneurysm has not been linked to the side on which TS appears. It has also been shown that anatomical proximity between the aneurysm and the vitreous cavity is not required in order for an intraocular haemorrhage to occur.3
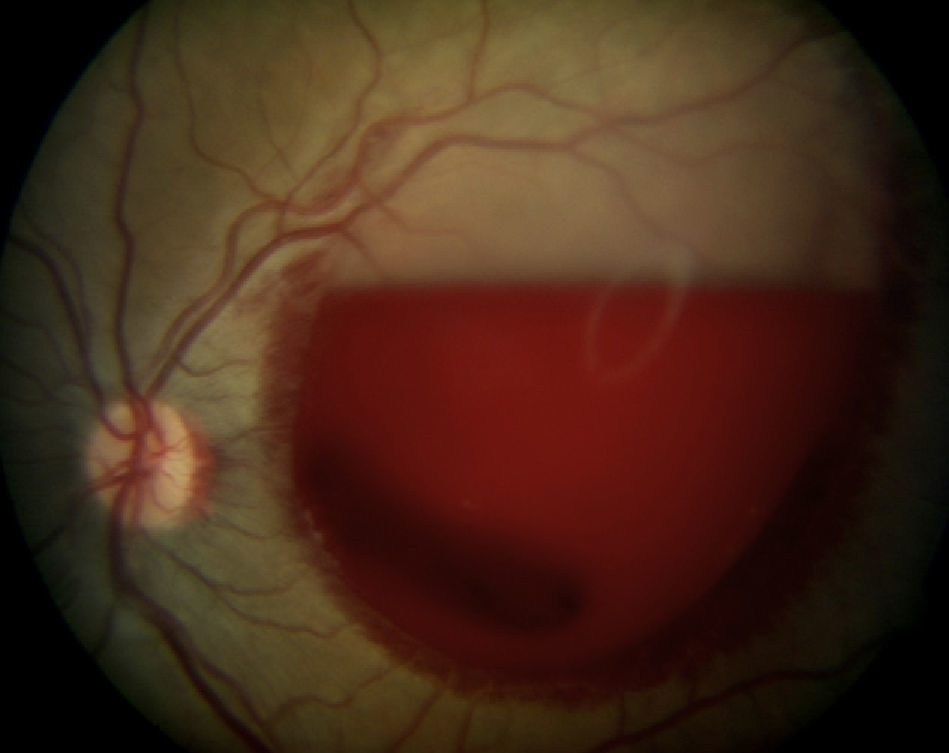
We present a case study of a white male who came to the emergency department due to sudden headache accompanied by vomiting and loss of consciousness. These symptoms resulted from SAH due to ruptured aneurysm, which was diagnosed by computed tomography (CT). The patient regained consciousness in 24h, which is very unusual; SAH patients normally remain in a coma for a longer period of time. The aneurysm was embolised several days later using a platinum microcoil. Nothing in the patient's medical history was relevant to the event. He was referred to an ophthalmologist due to loss of vision in the left eye (LE). Findings from the ophthalmic examination were normal, except for a large subhyaloid haemorrhage at the back of the LE that was affecting the macular area (Fig. 1). The haemorrhage was treated with Nd:YAG laser posterior hyaloidotomy. This caused a dense extension of blood in the vitreous cavity which was reabsorbed in 2 months, and the patient's eyesight recovered. This treatment option was chosen because the intraocular haemorrhage did not resolve spontaneously, and because the patient's condition discouraged us from subjecting him to stressful situations such as additional surgical procedures.4
It is a well-known fact that the presence of TS is an indicator of SAH severity.1 Most patients with TS remain unconscious for extended periods of time, as stated above, which is a sign of the magnitude of the condition. However, our patient's case was atypical, as he regained consciousness in 24h. In one study, Pfauser et al.3 found very high mortality rates among TS patients. Diagnosis of TS is indicative of a very poor prognosis, and frequently associated with rebleed from the aneurysm.
Therefore, examining the back of the eye in patients with SAH is a simple, non-invasive procedure that can provide information about the prognosis for SAH3; the outcome in our case, however, was atypical.
Please cite this article as: Sánchez Ferreiro AV, Muñoz Bellido L. Presentación atípica de un síndrome de Terson: A propósito de un caso. Neurología. 2012;27:380–1.