Posterior reversible encephalopathy syndrome (PRES) is the association of a set of clinical characteristics (headache, epileptic seizures, changes in alertness, visual loss and other focal deficits) and radiological signs indicating reversible changes in white matter, especially in the parietal-temporal-occipital area.1,2 It has been linked to high blood pressure and immunosuppressive agents, among other factors. Recurrence is infrequent; a recent study of 25 patients with long-term follow-up3 reported it in 8% of the study cases.
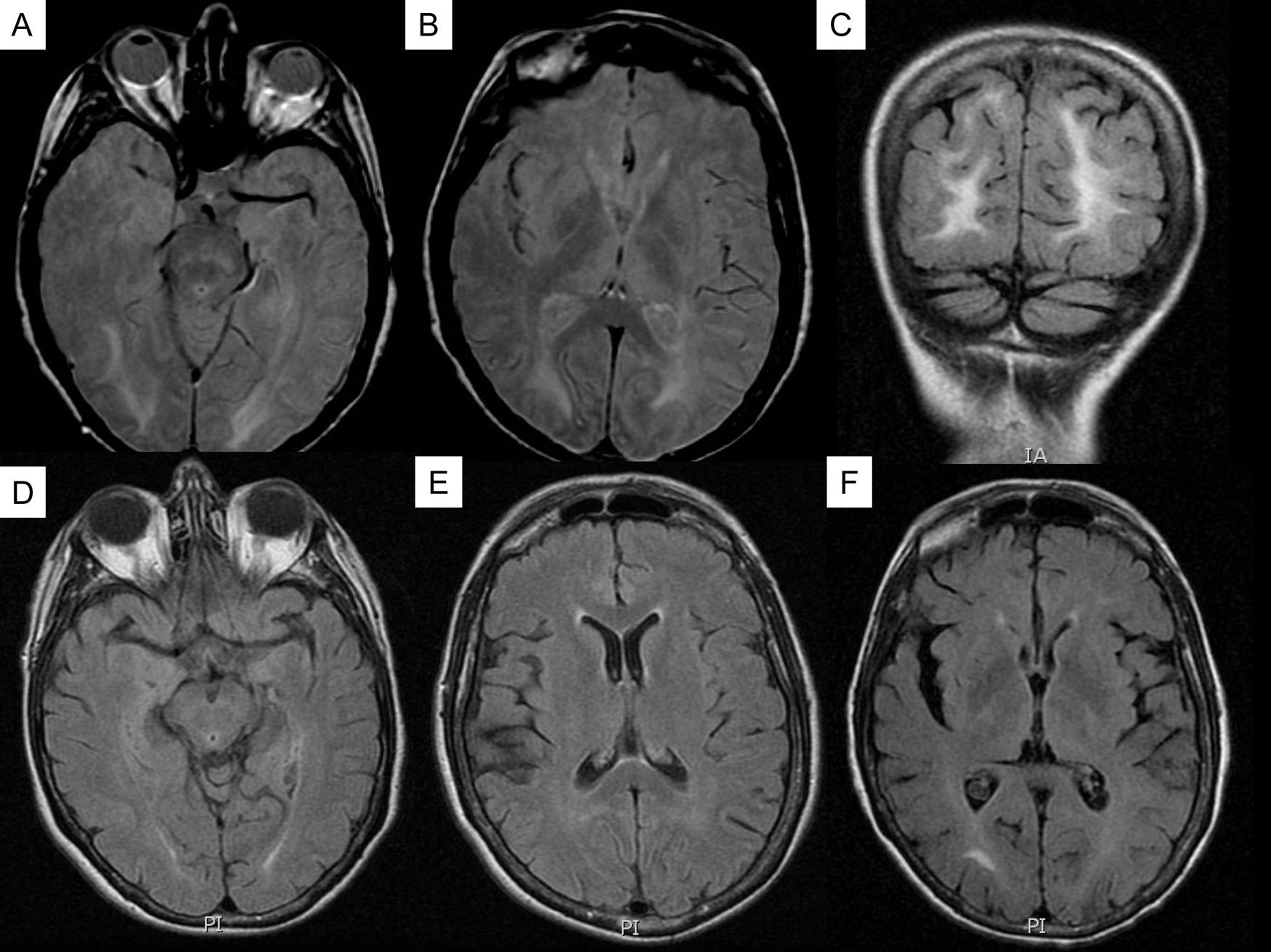
Various physiopathological mechanisms have been suggested, including vasoconstriction, increased perfusion, and endothelial damage. A study of recurrent cases may help us answer some of the unresolved questions about this syndrome. We present the case of a patient with recurrent PRES episodes which were effectively treated with nimodipine. The patient was a 60-year-old female who came to the emergency department in May 2009. She had a history of smoking, high blood pressure, high cholesterol, and ischaemic heart disease. She presented with headache, drowsiness, nausea, vomiting, and aphasic comprehension which had developed over 2 days, coinciding with an attack of hypertension (blood pressure 220/110mmHg). Once the hypertension had been resolved, the patient gradually regained her baseline state and was asymptomatic 48 to 72hours after being admitted. The patient had been treated with chemotherapy during the preceding 2 years for stage IV ovarian adenocarcinoma. Magnetic resonance (MR) scan showed predominantly parietal-occipital white matter lesions with no restrictions in the diffusion sequences. The lesions disappeared one month later (Fig. 1). Following that, the patient presented with 3 similar episodes in January, April, and June 2010; all episodes coincided with a marked increase in blood pressure. The MR scan showed changes similar to those described in PRES, which disappeared once the episode had resolved. The patient discontinued chemotherapy following the first episode and started antihypertensive treatment with beta blockers, ARBs, alpha blockers and diuretics; blood pressure control between episodes was good. Treatment with nimodipine was begun in June 2010; at 15 months of follow-up, no new episodes had occurred.
There are currently 2 hypotheses regarding PRES physiopathology. The first postulates that high blood pressure would cause arterial vasoconstriction, thereby producing ischaemia and cytotoxic oedema. The second supports there being a disturbance in cerebrovascular autoregulation secondary to uncontrolled high blood pressure. That condition subsequently leads to vasodilation, endothelial dysfunction and vasogenic oedema. The fact that parietal-occipital areas are predominantly involved is probably due to the sparse sympathetic innervation in posterior circulation. MRI findings seem to support the second hypothesis, as they revealed no restrictions in the diffusion sequence. However, cerebral vasoconstriction may be common in PRES, and it may also be related to reversible cerebral vasoconstriction syndrome (RCVS). Ducros et al. describe radiological findings for PRES in 10% of all cases of patients with RCVS.4 In turn, vasoconstriction has also been described in some published PRES case studies.5 It is not clear whether high blood pressure triggers the episode, or if in fact the episode causes high blood pressure.
Recurrence is uncommon in this syndrome. To our knowledge, there are only 15 published cases of recurrence at present, with a prevalence of 8% according to the series published by Roth et al.3 Various factors may be involved, including high blood pressure, chemotherapy, kidney failure, and eclampsia; however, persistence of these conditions has not been associated with episode recurrence.5 For example, our patient left chemotherapy following the first episode. Prior infection has been suggested as a possible episode trigger, but no such infection was present during any of the episodes in the clinical case we present here.
Most published cases of recurrence list 2 episodes, and the case we describe here has the highest number of recurrences recorded in the literature. Favourable response to nimodipine may be due to its role in preventing vasospasm, or caused by its effect on the endothelium. In fact, nimodipine has been put forth as a possible treatment for RCVS,6 but no clinical trials have been carried out for this use. Although ours is merely an isolated case, we suggest trying nimodipine as preventive treatment for new recurrent episodes of PRES.
Please cite this article as: Matías-Guiu JA, et al. Síndrome de encefalopatía posterior reversible recurrente con respuesta a nimodipino. Neurología. 2012;27:378–80.