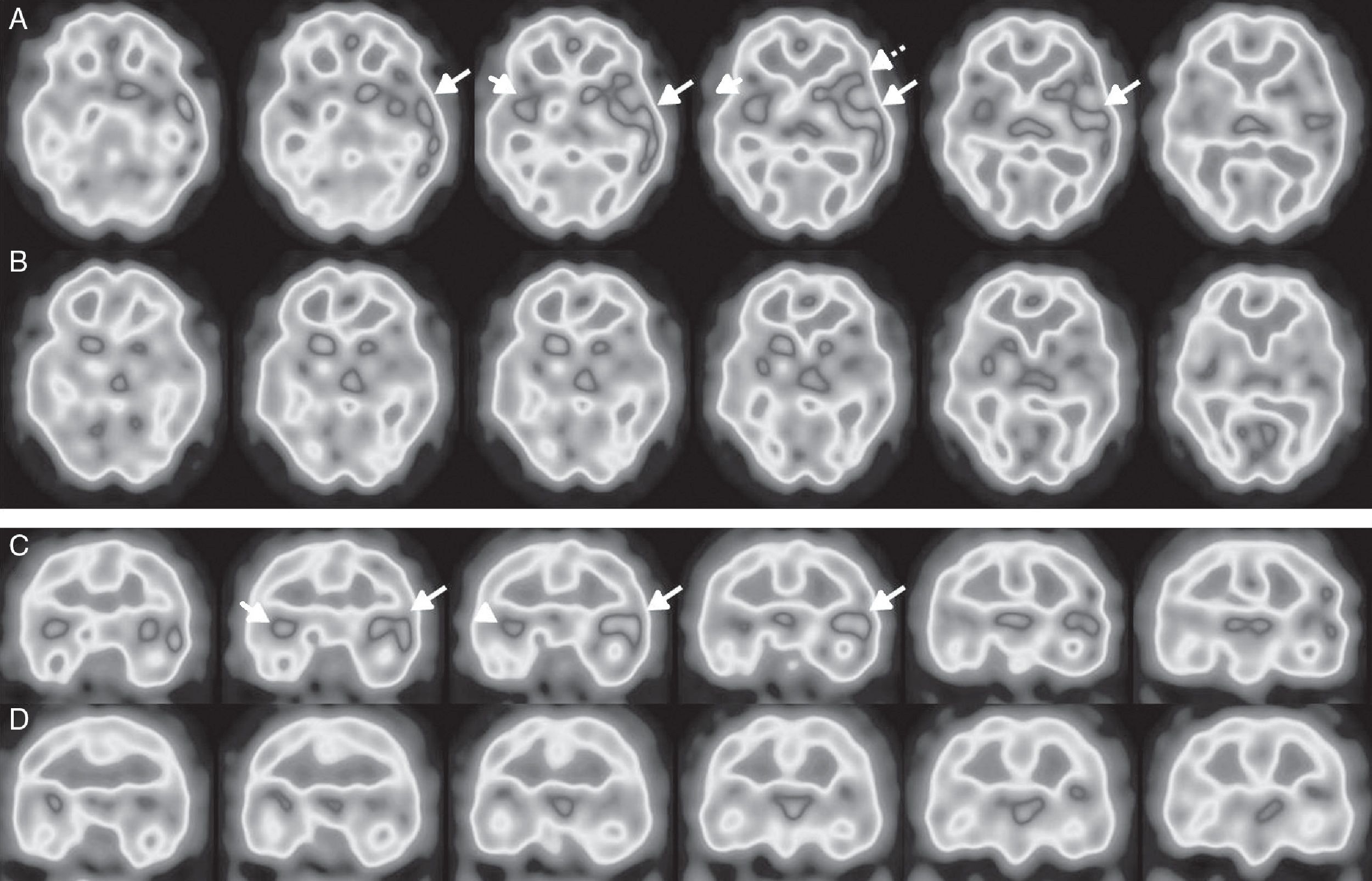
Anti-N-methyl-d-aspartate (NMDA) receptor encephalitis was first described in 2007. The most frequent forms result from extracellular antibody-mediated autoimmunity.1 Prognosis improves with early, aggressive immunotherapy; aetiological diagnosis is therefore essential. Diagnosis is based on the detection of anti-NMDA receptor antibodies in the serum and cerebrospinal fluid (CSF).2 MRI usually shows normal findings or mild alterations.3 Given the lack of specificity and the frequently subacute onset of symptoms, brain perfusion SPECT with 99mTc-HMPAO may be helpful for establishing a diagnosis, ruling out other conditions and revealing findings suggestive of encephalitis. However, SPECT findings in patients with anti-NMDA receptor encephalitis vary; alterations may affect one or both temporal lobes,4,5 and involve such other regions as the frontal lobe.3,6 We present the case of a 34-year-old man who was admitted with a 2-week history of progressive language impairment, which worsened in the days prior to admission. The examination revealed symptoms of aphasia associated with alexia and acalculia, as well as neuropsychiatric manifestations (agitation and delirium). At the age of 14 years, our patient had experienced an episode of refractory epilepsy, which was diagnosed as Rasmussen encephalitis and left no neurological sequelae. An EEG performed at admission revealed moderate, bilateral, frontotemporal, focal slow wave activity, predominantly affecting the left hemisphere, with no evidence of status epilepticus. Head CT and brain MRI scans revealed no alterations. Given suspicion of limbic encephalitis, we performed a brain perfusion SPECT with 99mTc-HMPAO, which showed hyperperfusion in the left temporal cortex; hyperperfusion in the right temporal cortex was less marked and less extensive. These findings are compatible with limbic encephalitis (Fig. 1A and C). Tests for anti-NMDA receptor antibodies in the CSF yielded positive results. The results of a chest, abdomen, and pelvis CT scan and a serum tumour marker test ruled out a paraneoplastic origin. The patient was diagnosed with non-paraneoplastic anti-NMDA receptor encephalitis and treated with corticosteroids, immunoglobulins, and rituximab. Clinical progression was unstable; language impairment and neuropsychiatric manifestations persisted, motor symptoms (myoclonus and rigidity, with no clear epileptogenic focus) worsened, and the patient developed symptoms of dysautonomia. Neurological symptoms improved progressively with cyclophosphamide. A follow-up brain SPECT scan performed 5 months after the initial symptoms showed near-complete resolution of the alterations (Fig. 1B and D). Other successfully treated patients with this type of encephalitis have also shown disappearance or improvement of abnormal findings in brain perfusion SPECT3,4 or 18F-FDG-PET.7 Brain perfusion SPECT played a crucial role in the diagnosis of this type of encephalitis given the atypical initial symptoms; language impairment of subacute onset suggested other diagnoses.
Brain perfusion SPECT scan with 99mTc-HMPAO, performed at diagnosis. Axial (A) and coronal (C) sequences showing hyperperfusion in the left temporal cortex (long arrows), predominantly in the superior lateral area and the insula, and extending to the adjacent frontotemporal area (Broca area) (dotted arrow). Hyperperfusion was less marked and less extensive in the right temporal cortex (short arrows). A follow-up study conducted after 5 months (B and D) revealed nearly complete resolution of abnormal brain perfusion.
Please cite this article as: Suárez JP, Domínguez ML, Gómez MA, Portilla JC, Gómez M, Casado I. SPECT cerebral de perfusión con 99mTc-HMPAO en el diagnóstico y seguimiento de la encefalitis con anticuerpos contra el receptor NMDA. Neurología. 2018;33:622–623.