Pseudo-occlusion (PO) of the cervical internal carotid artery (ICA) is defined as a flow artefact on CT angiography or digital subtraction angiography (DSA) images that mimics a complete occlusion of the extracranial carotid artery, when this arterial segment is in fact patent, with occlusion of the intracranial segment.1 This finding may influence the management of patients attended in the emergency department due to acute stroke, leading to misdiagnosis of tandem occlusion of the extracranial–intracranial ICA or arterial dissection and resulting in endovascular treatment being delayed or even ruled out.
We present the case of a patient with acute ischaemic stroke due to a thrombus in the left intracranial ICA that created an image of carotid PO at the cervical level. A brief literature review is provided.
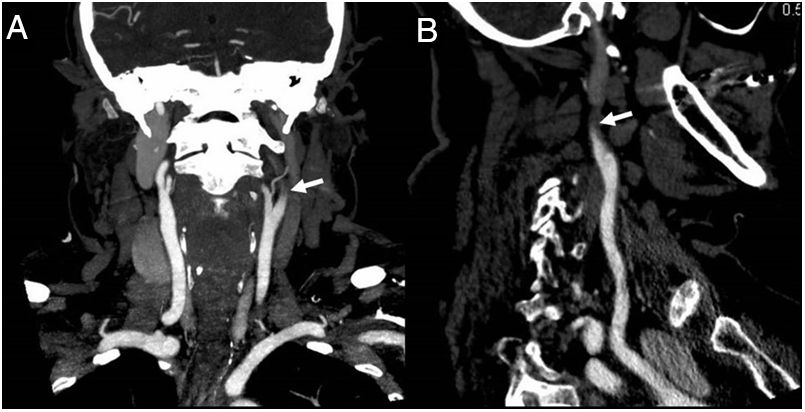
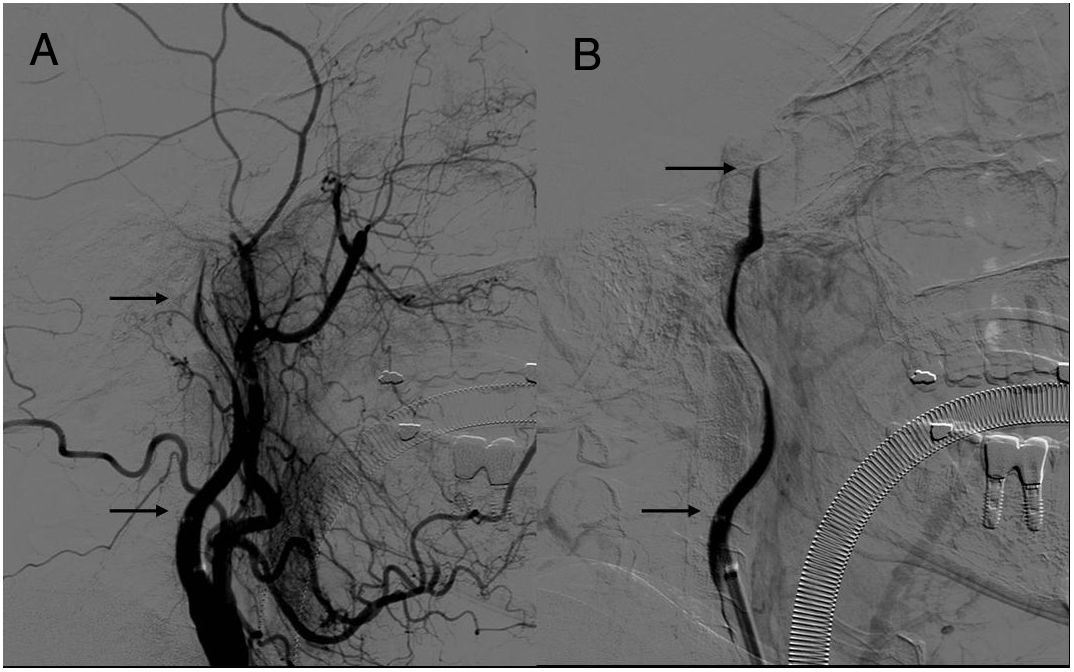
Our patient was a 55-year-old woman, with a history of smoking, arterial hypertension, dyslipidaemia, and paroxysmal atrial fibrillation, for which she was not receiving anticoagulant treatment. She awoke with speech difficulties and weakness in the right limbs and was taken to the emergency department. The neurological examination revealed predominantly motor mixed aphasia, right homonymous hemianopsia with conjugate eye deviation to the left, right faciobrachiocrural hemiparesis, and right hemihypaesthesia. She presented an NIHSS score of 22 points. An emergency brain CT scan showed loss of cortico-subcortical differentiation of the left insula and hypodensities in the left caudate and lenticular nuclei, scoring 7 on the ASPECTS scale. A CT perfusion scan showed an extensive penumbra and the results of a CT angiography study suggested occlusion of the left ICA from its origin, displaying the carotid slim sign (Fig. 1); these findings were considered to suggest carotid artery dissection. The patient was transferred to the interventional neurology department; DSA study showed contrast progressively flowing up through the left ICA to the intracranial portion (Fig. 2). After confirming the presence of arterial occlusion in the terminal portion of the left ICA only, we performed thrombus extraction by mechanical thrombectomy with a stent retriever, achieving complete recanalisation (TICI grade 3) with a single pass.
The following day the patient had improved, scoring 6 on the NIHSS scale. At a 3-month follow-up examination she presented minimal neurological impairment, scoring 1 on the modified Rankin Scale.
CT angiography findings of carotid PO, defined as a false image of complete extracranial occlusion due to fast scanning techniques and slowing or blockage of contrast flow due to a column of non-opacified blood, were first described by Kim et al.1 Some authors use the term “carotid pseudo-occlusion” to refer to a large lesion, generally atheromatous, that causes a high degree of stenosis (also referred to as subocclusive or preocclusive disease or critical stenosis) of the ICA.2 We use the term to refer to the acute phenomenon described at the beginning of the article.
Up to 46% of isolated occlusions of the intracranial ICA,3 and 11% of ischaemic strokes treated with endovascular techniques,4 may appear on imaging studies with carotid PO and occasionally flame-shaped tapering (characteristic of carotid dissection5) associated with a false image of occlusion. Although a multi-phase CT angiography or carotid Doppler ultrasound study may help in establishing a more precise diagnosis, the carotid PO images may be difficult to distinguish in up to 71% of cases, even after a DSA study with long acquisition times. In these cases, it may be necessary to perform a selective angiography study by inserting a microcatheter distally to the PO; in patients not presenting occlusion at this level, backfilling of the extracranial ICA will be observed when administering the contrast.3
In our patient, the false image of cervical carotid occlusion initially seemed to be associated with arterial dissection, but after administering contrast from the proximal portion of the affected ICA, we realised that this was a case of cervical carotid PO caused by a thrombus at the terminal segment of the ICA.
Cervical carotid PO is a relatively frequent phenomenon that can be observed in patients with stroke secondary to isolated occlusion of the intracranial ICA; it should be taken into account in patient management in order not to delay or rule out possible reperfusion treatment for eligible patients.
Please cite this article as: Tejada Meza H, Artal Roy J, Serrano Ponz M, Guelbenzu Morte S, Marta Moreno J. Pseudooclusión carotídea: un concepto a tener en cuenta en el ictus agudo. Neurología. 2020;35:344–345.