Amyotrophic lateral sclerosis (ALS) is a neurodegenerative disease characterised by rapid clinical deterioration. Survival times in patients with the condition range between 15.7 and 47 months from disease onset (mean, 29.1 months), depending on the series.1,2 The clinical features of the disease are heterogeneous and have been attributed to the combination of neurological signs and symptoms of upper and lower motor neuron dysfunction and death.3
Dysarthria and tongue atrophy with fasciculations are salient clinical features of bulbar- and bulbospinal-onset ALS, and also appear at later stages of spinal-onset ALS. Abnormalities of the tongue are caused by damage to the hypoglossal nucleus, which leads to flaccid dysarthria, a typical feature of lower motor neuron dysfunction. Upper motor neuron death results in corticobulbar tract dysfunction, which causes spastic dysarthria. Nasal voice may be observed in some patients with ALS who have no structural alterations in the tongue.4 Previous studies of patients with ALS report an incidental finding called the “bright tongue sign” in sagittal MR images of the brain. This sign has been associated with degeneration of the tongue and proposed as a useful radiological feature for diagnosing ALS.5–8 However, the significance of this magnetic resonance imaging (MRI) finding is still unknown. All patients with ALS and tongue abnormalities undergo brain MRI scans. However, clinicians frequently pay little attention to these abnormalities if patients show clinical signs of tongue atrophy and fasciculations.
We present a series of patients with ALS and tongue abnormalities, displaying a correlation between clinical and radiological (MRI) findings (bivariate analyses, t test, chi-square test, Mann–Whitney U test). We analysed the following clinical data: phenotype at baseline, disease severity, and progression time at the time of the MRI scan. We evaluated 43 patients with ALS according to the revised El Escorial clinical and neurophysiological diagnostic criteria.9 All patients completed the revised ALS Functional Rating Scale (ALSFRS-R) at baseline. Tongue hyperintensity, as compared to surrounding soft tissue, on T1-weighted FLAIR sequences was considered abnormal. On MR images: (1) the tongue completely fills the oral cavity; (2) it has a round shape; (3) the dorsal surface of the tongue forms an arch which touches the hard and the soft palate; and (4) the apex touches the posterior surface of the incisor teeth. The absence of at least 2 of these criteria was interpreted as constituting a structural abnormality of the tongue. Furthermore, we compared these findings to those of sagittal T1-weighted MR images from 15 sex- and age-matched healthy individuals.
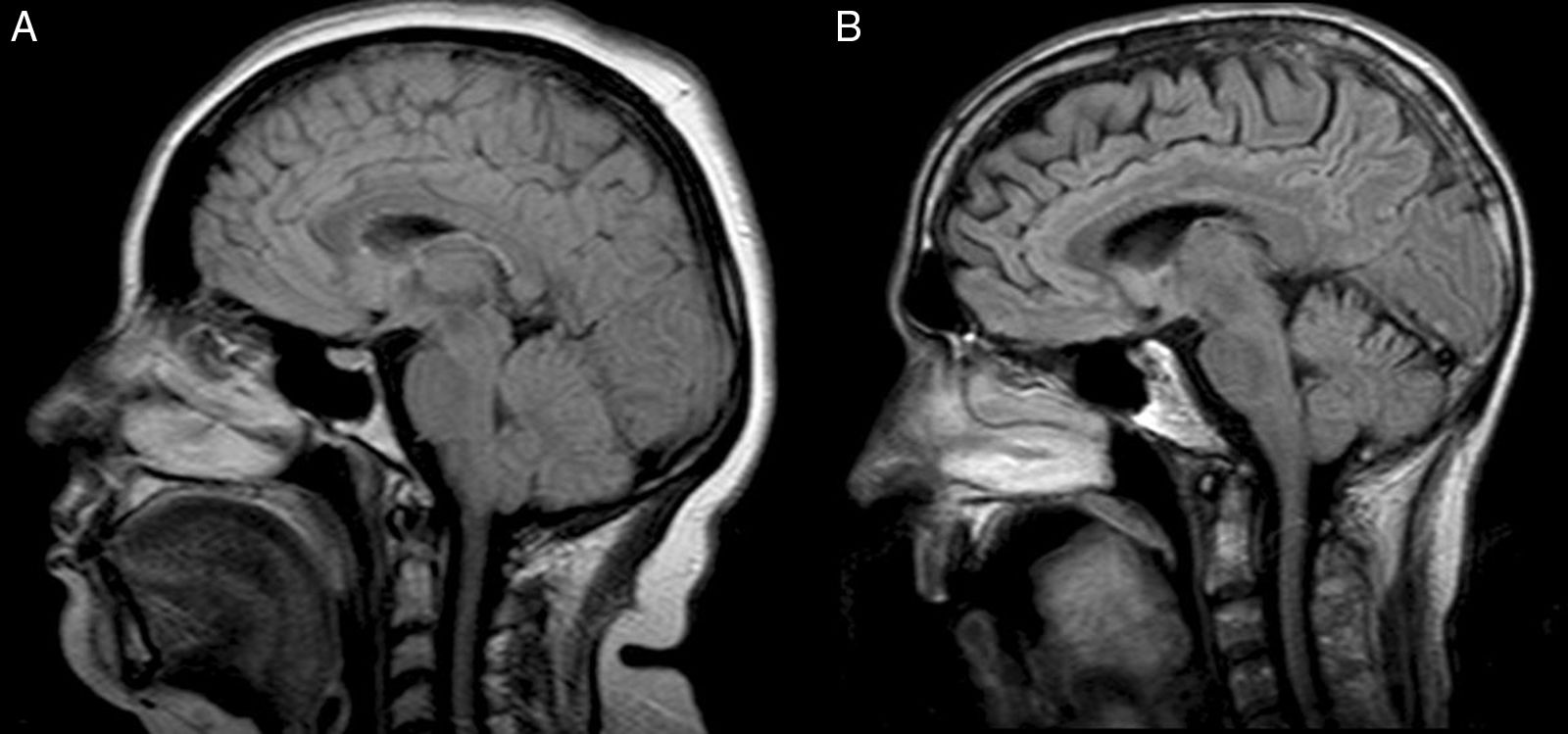
Tongue MRI results were normal in 19 patients (44%) and abnormal in 24 (54%) (Fig. 1). Mean disease progression time was 10 months in patients with normal MRI findings, and 18 months in patients with tongue abnormalities (P=.0071). No statistically significant association was found between disease severity and clinical phenotype. However, the patients with tongue abnormalities scored lower on the ALSFRS-R (29±6.01) than those with normal MRI findings (32.47±9.14).
MRI scan. Sagittal, T1-weighted FLAIR sequence. (A) A 41-year-old woman with bulbospinal-onset ALS manifesting 6 months previously. The shape, position, and signal intensity of her tongue were normal, including the internal structures. (B) A 49-year-old man with bulbospinal-onset ALS manifesting 23 months previously. Abnormalities can be observed in the shape, position, and signal intensity of the tongue; the internal structure is lost.
In ALS, clinical alterations of the tongue are caused by the death of lower motor neurons of the hypoglossal nerve and upper motor neurons of the motor cortex, which results in corticobulbar tract dysfunction.8 Over half of the patients in our series displayed clinical and radiological structural abnormalities of the tongue. We found an association between presence of MRI abnormalities and disease progression time. MRI hyperintensity is thought to be due to the replacement of tongue muscles, which atrophy due to chronic denervation, with fatty tissue.5 We found no association between ALS phenotype (bulbar, bulbospinal, or spinal) and the presence of MRI abnormalities; however, patients who scored lower than 30 on the ALSFRS-R were found to be more likely to display tongue abnormalities.
Presence of structural MRI abnormalities in the tongue does not constitute a reliable diagnostic criterion for ALS, but rather a complementary diagnostic criterion for lower motor neuron involvement in patients with ALS. Early detection of these alterations may indicate greater disease severity.
Author's contributionAll authors contributed to the manuscript and meet the ICMJE criteria for authorship.
Please cite this article as: Martínez HR, Escamilla-Ocañas CE, González-Garza MT, Moreno Cuevas JE. Anormalidades clínicas y por resonancia magnética en lengua de pacientes con esclerosis lateral amiotrófica. Neurología. 2018;33:276–278.