Intravenous thrombolysis with alteplase is an effective treatment for ischaemic stroke when applied during the first 4.5hours, but less than 15% of patients have access to this technique. Mechanical thrombectomy is more frequently able to recanalise proximal occlusions in large vessels, but the infrastructure it requires makes it even less available.
MethodsWe describe the implementation of code stroke in Asturias, as well as the process of adapting various existing resources for urgent stroke care in the region. By considering these resources, and the demographic and geographic circumstances of our region, we examine ways of reorganising the code stroke protocol that would optimise treatment times and provide the most appropriate treatment for each patient.
ResultsWe distributed the 8 health districts in Asturias so as to permit referral of candidates for reperfusion therapies to either of the 2 hospitals with 24-hour stroke units and on-call neurologists and providing IV fibrinolysis. Hospitals were assigned according to proximity and stroke severity; the most severe cases were immediately referred to the hospital with on-call interventional neurology care. Patient triage was provided by pre-hospital emergency services according to the NIHSS score.
ConclusionsModifications to code stroke in Asturias have allowed us to apply reperfusion therapies with good results, while emphasising equitable care and managing the severity-time ratio to offer the best and safest treatment for each patient as soon as possible.
La trombólisis intravenosa con alteplasa es un tratamiento efectivo para el ictus isquémico si se aplica dentro de las primeras 4,5 horas, pero al que acceden <15% de los pacientes. La trombectomía mecánica recanaliza más obstrucciones proximales en las grandes arterias, pero necesita una infraestructura que la hace menos disponible.
MétodosSe detalla la evolución del código ictus en el Principado de Asturias y la adaptación del mismo a los sucesivos recursos para la atención urgente al ictus en la región. Teniendo en cuenta dichos recursos, las circunstancias poblacionales y geográficas de nuestra región, se plantea la reorganización del código ictus buscando la optimización del tiempo y la adecuación a cada paciente.
ResultadosReparto de las ocho áreas sanitarias de Asturias para derivar los pacientes candidatos a tratamientos de reperfusión hacia los dos hospitales donde se dispone de Unidad de Ictus y guardia de Neurología, con posibilidad de aplicar la fibrinólisis IV. Este reparto se realizó en función de la proximidad y la gravedad de los mismos, derivando todos los casos más graves directamente al hospital que dispone de guardia de Neurorradiología Intervencionista. El cribado del paciente se realizó por los Servicios de Emergencias Extrahospitalarias según la escala NIHSS.
ConclusionesLas modificaciones en el código ictus de Asturias permiten ofrecer tratamientos recanalizadores con buenos resultados, buscando la equidad y optimizando el manejo del binomio gravedad-tiempo para ofrecer a cada paciente el tratamiento óptimo en el menor plazo de tiempo posible y en condiciones de seguridad.
Stroke is the most frequent cause of permanent disability in adults and one of the leading causes of death both in Spain and throughout the Western world, resulting in enormous personal suffering and a high cost to society.1 In the case of Spain, the cumulative incidence of cerebrovascular disease per 100 000 people older than 24 years has risen to 218 new cases in men and 127 in women.2
Intravenous thrombolysis with tissue plasminogen activator (tPA) is an effective treatment for acute ischaemic stroke if administered within 4.5hours from symptom onset.3 In the case of proximal large-vessel occlusion, however, mechanical thrombectomy appears to be more effective, although until now no studies have provided conclusive evidence.3–10 In any case, the sooner these treatments are administered, even within the time window, the greater their effectiveness.11
Code stroke is a system of patient identification and follow-up whose objective is to ensure that acute stroke patients have access to a cerebrovascular reference centre in the minimum time possible. This system requires that emergency services, primary care centres, and local hospitals of a specific area work in close coordination with the stroke reference centre, where specialised seamless care is offered to patients.12
Occasionally, treatments directed towards rapid and effective arterial recanalisation are based on advanced interventional neuroimaging or neuroradiology techniques, which are only available at tertiary centres. Therefore, code stroke should include several levels of care, or types of healthcare centres, to provide the most suitable treatment for each case.13
Code stroke has been proven to be effective, reducing time from symptom onset to diagnosis and specialised treatment, as well as increasing the number of patients attended in stroke units and those treated with fibrinolytics.14
Public healthcare resources in AsturiasAsturias is a single-province autonomous community with a total area of 10603.57km2 and 1068 165 inhabitants (according to 2014 data from Spain's National Statistics Institute). This region has the highest mortality rate in Spain (11.77 deaths per 1000 population) and the lowest birth rate (6.91 births per 1000 population), which results in a negative growth rate and progressive population ageing. The bulk of this population is concentrated in the central area of Asturias, while the eastern and western areas are depopulating.
The terrain is rugged, which historically has meant difficulties in communication. In recent years, the construction of motorways has to some extent alleviated this problem, but in some rural areas access is still limited.
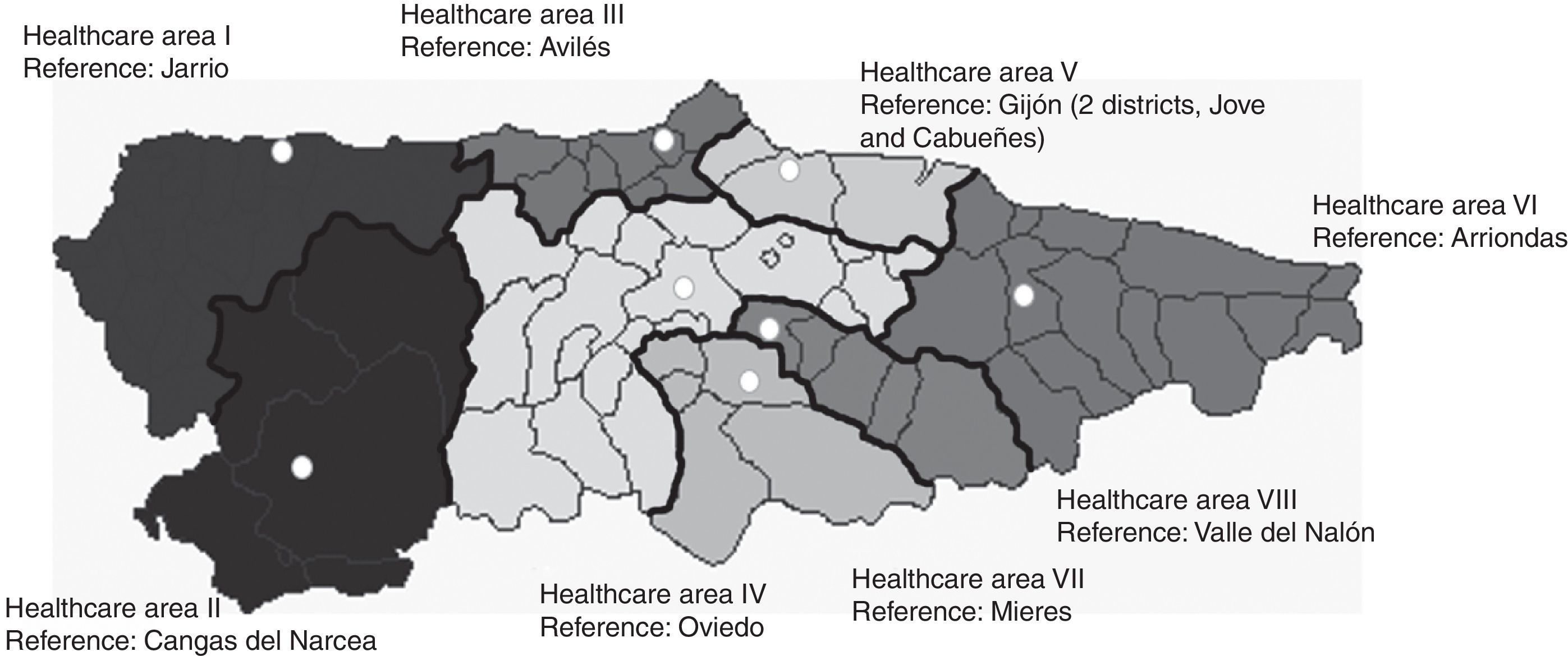
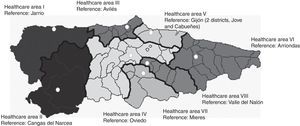
The health service is organised into 8 administrative areas (Fig. 1), each of which has one hospital as a base, except for area V, which is divided into 2 districts and has, accordingly, 2 reference hospitals. In total there are 66 health centres in the region. Of the 9 hospitals mentioned, only the Hospital Universitario Central de Asturias (HUCA), in Oviedo, has a neurology department. Another 5 hospitals (Cabueñes and Jove, in Gijón, as well as Avilés, Valle del Nalón, and Mieres) have neurology sections in the internal medicine departments. In addition, one hospital, Jarrio, has an on-staff neurologist. The remaining 2, in Cangas del Narcea and Arriondas, do not have any neurologists on staff. There are stroke units with 24-hour on-call neurologists at the HUCA and the Hospital de Cabueñes, and on-call neurointerventionists and a neurosurgery department exclusively at the HUCA.
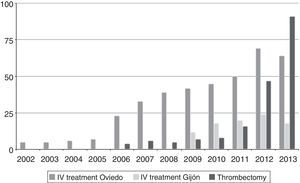
Changes in acute stroke care in AsturiasThe first intravenous fibrinolysis took place in the Hospital Universitario Central de Asturias in February 2001 under a compassionate use protocol. At that time there were no stroke units in the region, and patients who had undergone fibrinolysis were subsequently monitored in the intermediate care unit, which pertained to the intensive care unit. That was the first version of code stroke, although at that point it was solely for patients from healthcare district IV, where the HUCA is the reference hospital. In 2005, code stroke was established regionally. It provided healthcare to the whole region and was centralised in Oviedo, since the HUCA continued to be the only hospital which offered fibrinolytic treatment for stroke, as well as the only one with on-call neurologists. A year later, the HUCA conducted the first neurointerventional procedures, which were only available in the mornings.
In 2008, the first stroke unit in Asturias was created in the Hospital de Cabueñes, and in 2009, the HUCA and the Cabueñes both began to offer intravenous fibrinolytic treatment. The Hospital de Cabueñes served as the reference hospital for its health district (V) and the HUCA for the rest of the region. In 2010, the HUCA inaugurated the second stroke unit. That same year neurointerventionists began to use stent-retrievers, although this treatment remained available only in the mornings.
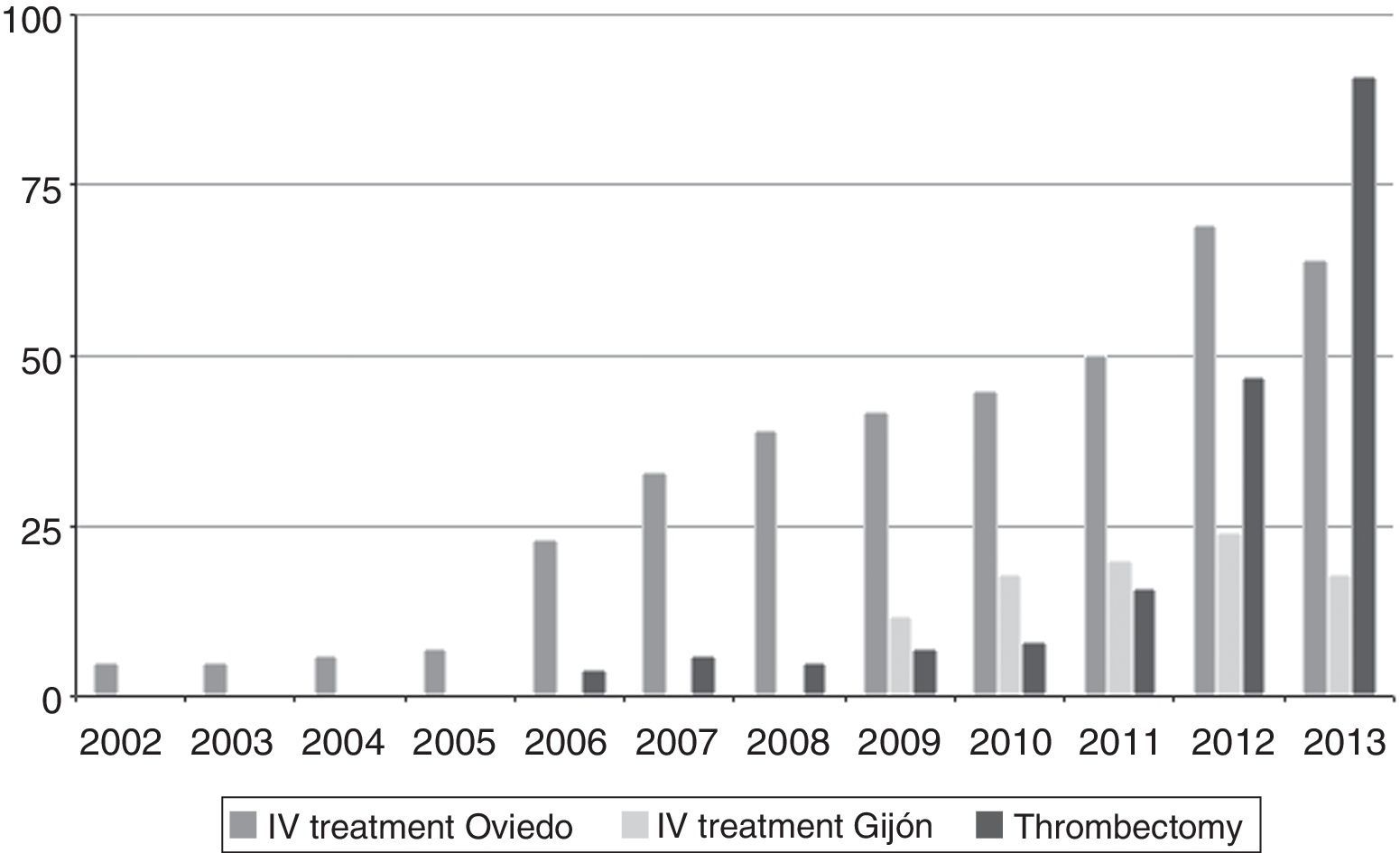
These progressive steps resulted in an increase in the number of patients who benefited from the new treatments. Fig. 2 shows the changes in the number of treated patients between 2002 and 2013.
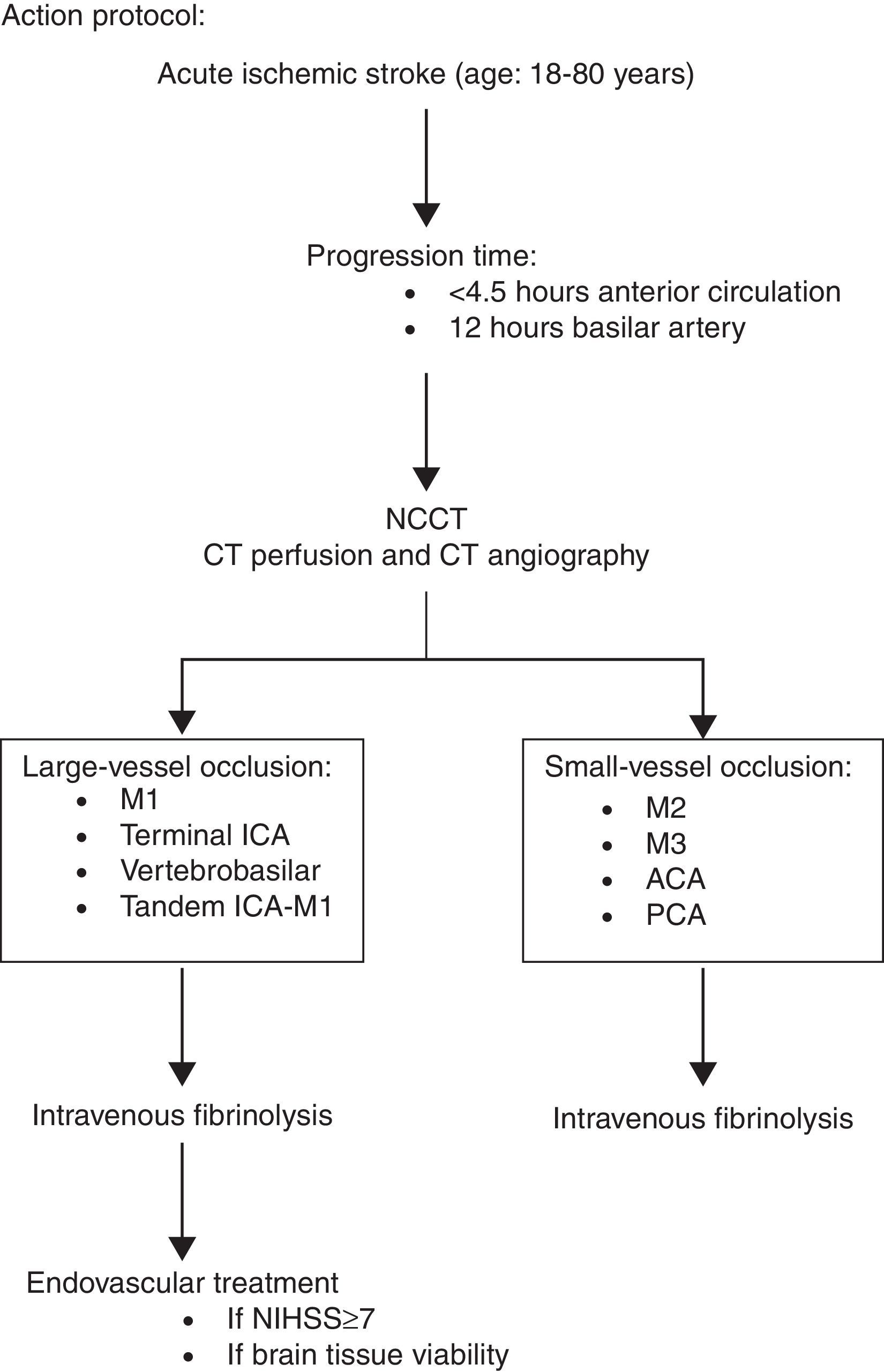
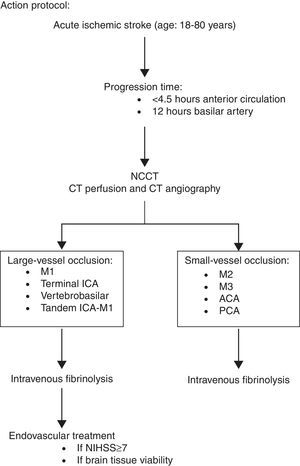
Code stroke protocol 2013In June 2012, the HUCA introduced its on-call neurointerventional service. For the first time, mechanical thrombectomy techniques, including the use of extraction devices such as stent-retrievers, were available 24hours a day, 7 days a week. The acute stroke treatment protocol was modified to include this new therapeutic option as shown in the algorithm in Fig. 3, following the recommendations agreed upon by the ad hoc SEN's Cerebrovascular Disease Study Group.15 It should be noted that people up to 80 years of age are eligible for interventional treatment. When our protocol was implemented, these treatments had not yet been well validated, and several studies conducted at that time included patients only from within that age range.5,8,10 However our current protocol should be modified in light of the results of new clinical trials.4,6,7,9
Until then, the regional code stroke had established that patients from area V should be referred to the Hospital of Cabueñes, as it was the reference hospital for that area, much as patients from the rest of the region used the HUCA, in Oviedo, as their reference hospital. It was quickly noted that the introduction of neurointerventional techniques resulted in inequality of treatment standards. Patients referred to Oviedo could undergo intra-arterial procedures as soon as these were indicated, while patients who were treated in Gijón had to be transported to Oviedo once the inefficacy of the IV treatment was confirmed, with the ensuing delays (over an hour in the majority of cases). In addition, Gijón did not have a multimodal CT scanner in the emergency department so radiological findings could not be used to indicate intra-arterial treatment. Indication was based solely on patients’ clinical assessment and response to treatment.
The most important variable predicting how an acute stroke patient will respond to recanalisation is the time elapsed between symptom onset and initiation of treatment.16 However, a second element to consider when assessing acute stroke treatment is the poor effectiveness of fibrinolysis for large-vessel occlusions. Only one in 3 patients treated with IV recombinant tPA within the first 3hours after symptom onset will return to a modified Rankin Scale score of 0 or 1.17 However, if the occlusion is located in the proximal middle cerebral artery only 15% to 20% of cases will recanalise in the 2hours following recombinant tPA infusion, and the numbers are even lower for occlusions in the carotid or basilar arteries.18
This leads us to the dilemma of prehospital stroke assessment: patients should be treated as quickly as possible, which means moving them to the closest hospital that can administer IV fibrinolysis, but those with more severe strokes will benefit little from that treatment and would be better off going straight to centres with the capacity for more advanced treatment. The problem that arises is how to do the prehospital triage and decide where to transport each patient.
The probability of presenting a large-vessel intracranial occlusion is directly proportional to stroke severity as measured by the National Institutes of Health Stroke Scale (NIHSS).19 In the United States, where prehospital care is primarily administered by paramedics, simple stroke assessment scales for use in situ have been designed to improve stroke diagnosis. The Los Angeles motor scale has demonstrated the capacity to predict the presence of large-vessel occlusions (scores≥4) with a sensitivity of 0.81, a specificity of 0.89, and an overall accuracy of 0.85.20 This scale is being used in a number of prehospital stroke triage programmes in the U.S.21
Prehospital care in Spain is provided by healthcare teams which each consist of a doctor and a nurse. In Asturias, emergency medical service staff members receive instruction in the application of NIHSS and when code stroke is activated in our region, prehospital care teams assess stroke severity using this scale. There is a strong correlation between NIHSS scores reported by emergency medical service doctors and those from the neurologists in our setting, which supports the validity of patient triage by prehospital personnel.22
Various studies have concluded that a threshold of 10 points on this scale reliably discriminates between patients with large-vessel occlusions (eventual intravascular treatment candidates) and those without.11,23
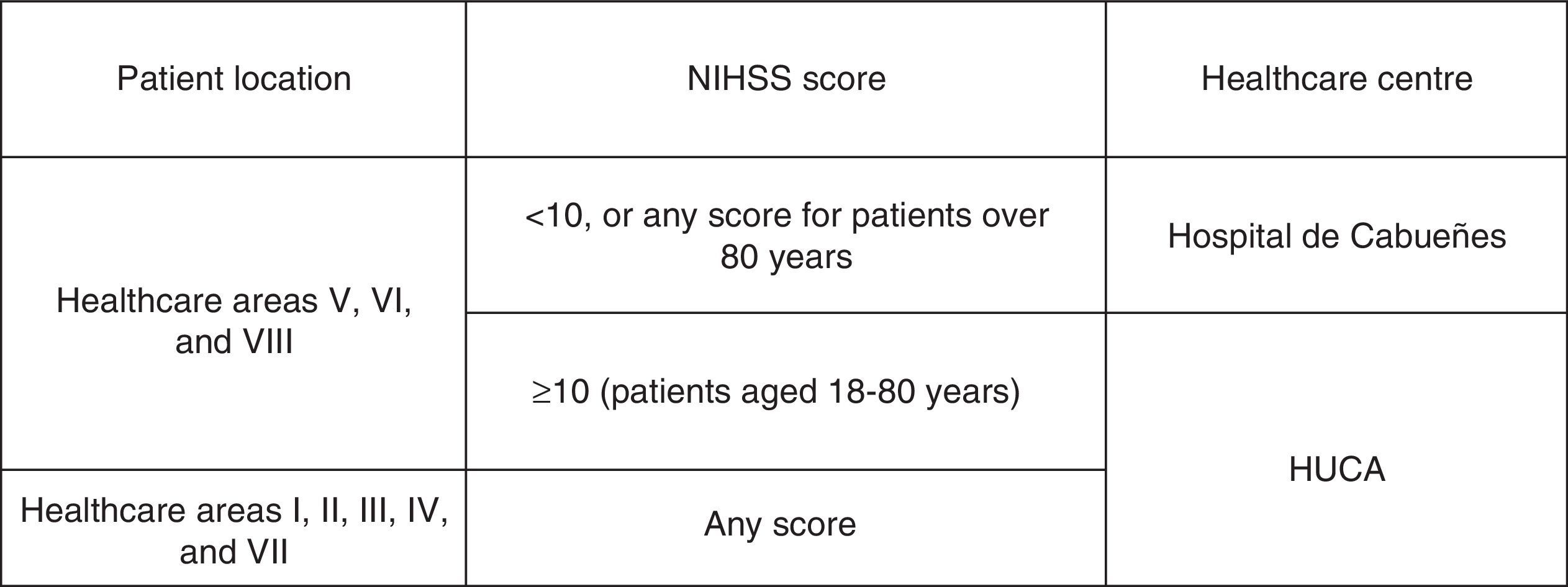
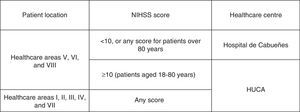
Considering these results, the following territorial structure was established for acute stroke care (Fig. 4):
- •
The Hospital de Cabueñes is the primary stroke centre for patients from areas V, VI, and VII. The exclusion criteria are:
- o
NIHSS score≥10
- o
Patients taking anticoagulants
- o
Patients for whom IV fibrinolysis is contraindicated but who could undergo mechanical thrombectomy
- o
- •
Patients from the rest of the healthcare areas of Asturias and those from areas V, VI, and VII who meet the previously mentioned requirements are taken directly to the Hospital Universitario Central de Asturias.
The latest version of the Asturian code stroke protocol offers recanalisation to acute stroke patients in an equitable manner, minimising geographical limitations and optimising management of the severity-time ratio in order to offer each patient the best possible treatment in the least time.
Additional changes should be made to further the knowledge of the general population and prehospital emergency care and primary care professionals with regards to stroke warning signs and the best way to proceed when the first symptoms occur. Without these additional changes, the percentage of patients receiving treatment will reach a ceiling despite any further therapeutic advances.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Benavente L, Villanueva MJ, Vega P, Casado I, Vidal JA, Castaño B, et al. El código ictus de Asturias. Neurología. 2016;31:143–148.