Atherosclerosis of the basilar artery is the most frequent cause of basilar thrombosis,1 which is one of the most serious neurovascular diseases with an 80% rate of death or disability.2,3 However, there are no randomised clinical trials addressing the treatment of acute basilar occlusion.4 At present, endovascular treatment for acute stroke is provided in cases of demonstrated arterial occlusion in which intravenous thrombolysis fails or is contraindicated, although experience with endovascular treatment for acute stroke due to intracranial atherosclerosis is limited. Results from the SAMMPRIS study were recently published after patient recruitment had been halted ahead of schedule.5 These results support intensive medical treatment over endovascular treatment in cases of non-disabling stroke caused by symptomatic intracranial stenosis of more than 70%. These results have led researchers to reconsider the indications for endovascular treatment in cases of intracranial stenosis. We present 2 patients with critical and symptomatic basilar artery stenosis who underwent stent placement during the acute phase.
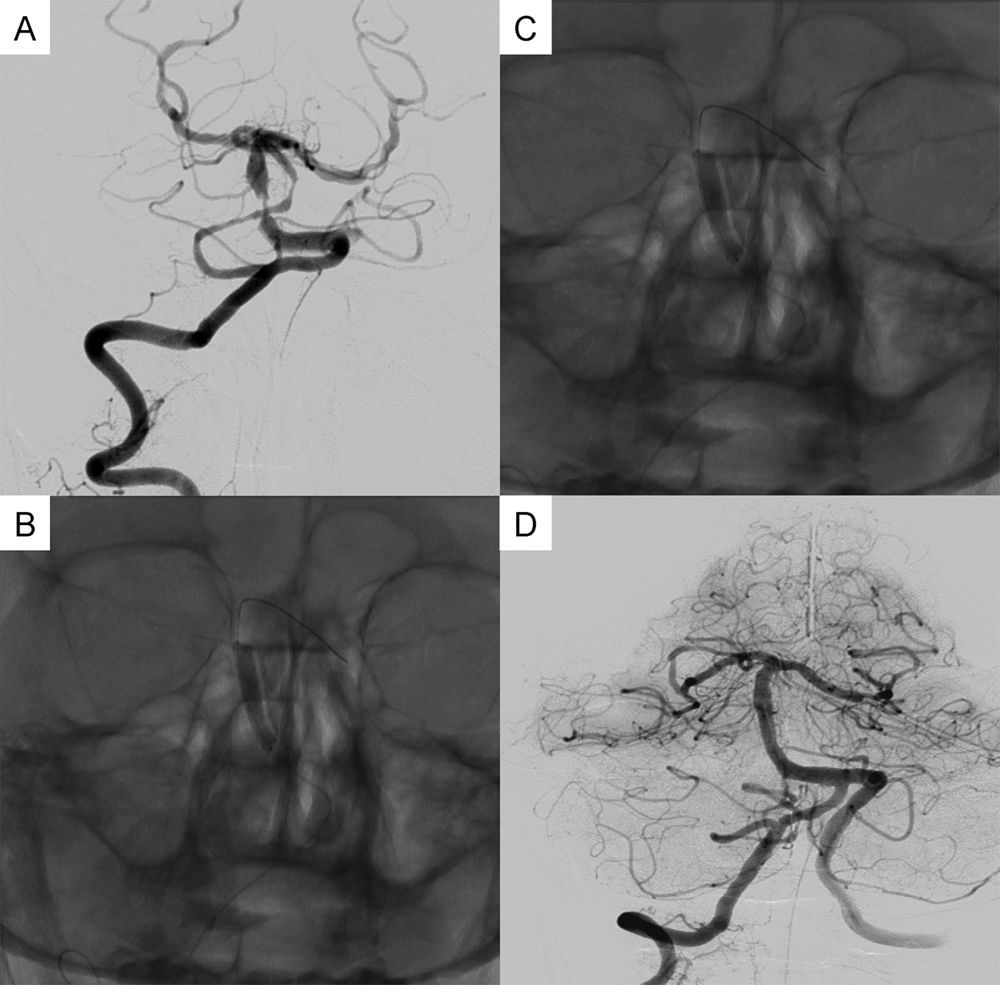
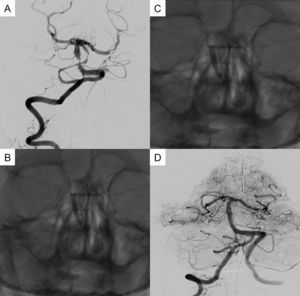
Case 1. We present the case of a male smoker aged 62 years with high blood pressure and dyslipidaemia. In the preceding year, he had experienced several 10-minute episodes of dizziness, dysarthria, binocular diplopia, and weakness, tingling, and clumsiness in extremities on the left side. Episodes were becoming increasingly frequent. He was admitted due to a new transient ischaemic attack and diagnosed with basilar stenosis using transcranial Doppler ultrasound (mean velocity of 200cm/s). The patient was scheduled for stent placement. While waiting for the stent, he presented a new episode with dysarthria, left hemiplegia, and left-side eye deviation. Cranial CT revealed no relevant changes; CT angiography displayed critical stenosis of the basilar artery. The patient's clinical symptoms improved and had completely disappeared within 1 hour. Nevertheless, we opted for urgent endovascular treatment for stenosis by placing a Pharos Vitesse® balloon-expandable stent 4×20 (Micrus®) and administering heparin and dual antiplatelet therapy (Fig. 1).
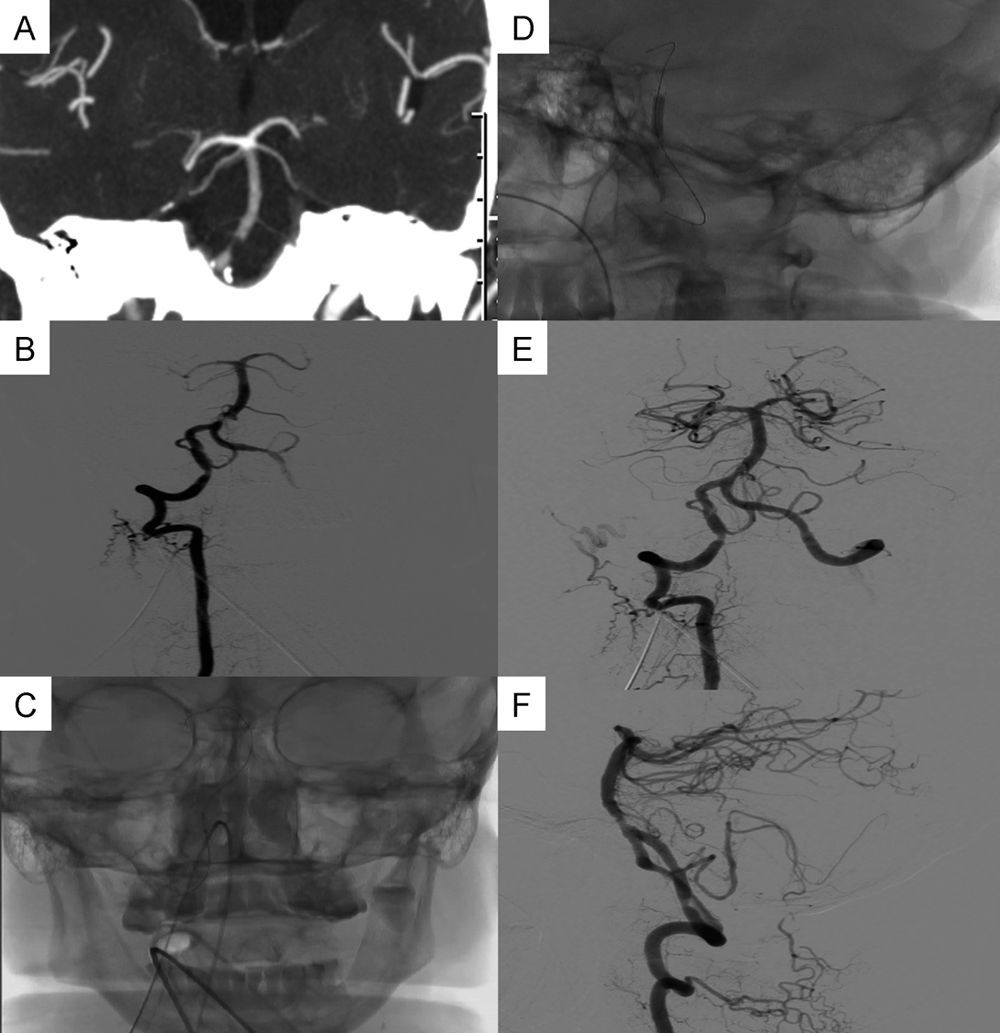
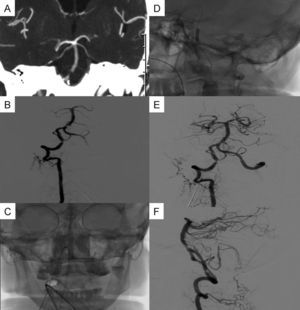
Case 2. We present a male aged 63 with a history of arterial hypertension and ischaemic heart disease. While exercising, he experienced sudden-onset drowsiness, right hemianopia, visual agnosia, and nystagmus (NIHSS 4). Intravenous thrombolysis with rtPA was delivered; the patient exhibited symptoms of dysarthria, miotic pupils, left-sided deviation of head and eyes, right supranuclear facial paresis, and tetraparesis (NIHSS 17). Doctors performed a CT angiography which showed critical basilar artery stenosis with decreased distal filling. The patient was then referred to our centre for endovascular treatment. Angiography showed 40% stenosis of the right vertebral artery and critical stenosis in the proximal third of the basilar artery (Fig. 2). The patient underwent angioplasty and placement of a Wingspan® self-expandable stent 4×20 (Stryker®) while receiving antiplatelet therapy with aspirin. The procedure took place 9hours and 50minutes after the onset of the first symptoms and 7hours and 30minutes after clinical impairment. The MRI revealed a left temporo-occipital infarction with haemorrhagic transformation (HI2). The patient recovered well, except for experiencing anterograde memory loss which resolved in the subsequent weeks.
Intracranial atherosclerosis is increasingly being recognised as an important cause of ischaemic stroke.6 Treatment takes place on 3 levels and includes stabilising atheromatous plaque, preventing the formation or break-up of thrombi resulting from a complication of the plaque, and improving blood flow and perfusion. The SAMMPRIS study has shown that patients with non-disabling TIA or stroke associated with severe stenosis of the intracranial artery (above 70%) present a lower stroke rate during the first 30 days when receiving aggressive medical treatment, compared to the group of patients treated with angioplasty and Wingspan® stent placement. After 30 days, the number of patients with stroke was the same in both groups.
We chose acute endovascular treatment for our clinical cases due to the risk of recurrence, progression, or recalcitrance of the neurological deficit. In both cases, prognosis was favourable. Patients presented no complications after 2 years of follow-up. Both cases were treated prior to the publication of results from the SAMMPRIS study. As a result, at least in the first case, we do not know how the patient would have progressed with intensive medical treatment prior to being admitted. These 2 patients had stenosis of the basilar artery with haemodynamic failure. The different autoregulation mechanisms (vasodilation, increased oxygen extraction ratio) probably failed in both cases. Haemodynamic impairment may also lead to local thrombophilia.7 Therefore, the risk of recurrence and progression of the neurological deficit is considered high when revascularisation is lacking. In this case, endovascular treatment (as shown by case 1) rapidly improves the haemodynamic state, which is difficult to achieve using medical treatment only.
There are few studies on the acute treatment of basilar artery stroke and most of them refer to patients with complete occlusion,4,8 which mainly compare antiplatelet monotherapy, intravenous fibrinolysis, and intra-arterial fibrinolytic therapy. In addition, data concerning basilar atherosclerosis are scarce. As shown by the angiography conducted during endovascular treatment for acute stroke, basilar stenosis is a frequent cause of basilar artery occlusion,1 whether after use of a thrombus extraction device or after administration of a fibrinolytic drug. After this step, definitive treatment consists of stent placement or angioplasty. However, we may also find cases of severe stenosis without occlusion, as in case 2, which also require this treatment.
Atherosclerosis is a systemic disease, and with this in mind, using medical treatment as the first option is both logical and consistent with available evidence. However, endovascular treatment may be indicated as the first choice in some situations. We suggest that critical stenosis of the basilar artery associated with clinical instability and haemodynamic impairment may be a new indication for acute endovascular treatment. The purpose of this treatment is to avoid stenosis progression and prevent a fatal or disabling stroke. However, clinical trials will be necessary in order to demonstrate treatment benefits in this group of patients.
Please cite this article as: Matias-Guiu JA, et al. Estenosis crítica de arteria basilar asociada a inestabilidad clínica: propuesta de una nueva indicación de tratamiento endovascular agudo. Neurología. 2013;28:321–2.