In-hospital stroke (IHS) is a frequent event, but its care priority level is not well established in many hospitals. IHS care at our centre has been redefined by implementing a training programme for medical personnel not usually involved in stroke management, in order to optimise IHS detection and treatment. This study evaluates results from the training programme.
MethodsIt was a prospective longitudinal intervention study. Neurologists experienced in vascular diseases developed a training programme for medical personnel. We recorded incidence, epidemiological data, reason for hospitalisation, department, aetiology, severity (NIHSS), time from symptom onset to neurological assessment, use of endovascular thrombolysis, exclusion criteria for untreated patients, and 90-day outcome (mortality/disability) in 2 patient groups: patients experiencing IHS in the 6 months before (PRE) and the 6 months after the training programme (POST).
ResultsSixty patients were included (19 PRE, 41 POST) with a mean age of 75.3±12.5; 41% were male. There were no differences between groups regarding assessment time, treatment administered, or morbidity/mortality. Overall, 68.3% of the patients were assessed in <4.5hours; however, only 6 patients (10%) were able to undergo endovascular therapy. This situation was mainly due to pre-existing disability (26%) and comorbidity (13%).
ConclusionsMore IHS code activations were recorded after the training programme. However, that increase was not accompanied by a higher percentage of treated patients or improvements in patient prognosis during the study period, and these findings could probably be explained by the high rates of pre-existing disability and comorbidity in this series.
El ictus intrahospitalario (IIH) es frecuente, pero su atención preferente no está bien establecida en muchos centros hospitalarios. En nuestro centro, como medida de calidad asistencial, se intentó reorganizar la atención al IIH mediante un programa de formación teórica y entrenamiento a profesionales sanitarios no implicados habitualmente en el manejo de pacientes con ictus, para optimizar la detección y el tratamiento del IIH. Se evalúan resultados del programa de formación.
MétodosEstudio prospectivo longitudinal de intervención. Se elaboró un programa de formación a personal médico y enfermería. Se registró a los pacientes con IIH pre (PRE) y posformación (POST) (6 meses cada grupo) y se evaluaron los datos de incidencia, datos epidemiológicos, motivo de ingreso y servicio, etiología, severidad, tiempo hasta evaluación por Neurología, tratamiento recanalizador (trombólisis intravenosa/intravascular), criterios de exclusión en no tratados y pronóstico (mortalidad/discapacidad) en ambos grupos.
ResultadosSe identificó a 60 pacientes con IIH, con una edad media de 75,3 ± 12,5, 41% hombres; 19 PRE/41 POST. Sin diferencias entre grupos en el tiempo de evaluación, el tratamiento o la morbimortalidad. El 68,3% de ellos fueron evaluados en < 4,5h, de los cuales solo fue posible administrar tratamiento recanalizador en 6 pacientes (10%), debido fundamentalmente a dependencia previa (26%) y comorbilidad (13%).
ConclusionesEl programa de formación realizado permite un mayor número de activaciones de código ictus intrahospitalario. Sin embargo, en el periodo evaluado, esto no se tradujo en mayor porcentaje de pacientes tratados o mejor pronóstico, probablemente debido a la discapacidad previa y comorbilidad elevada en esta serie.
Cerebrovascular diseases are the third leading cause of death in the Western world, the leading cause of physical disability in adult populations, and the second leading cause of dementia.1 Stroke care has advanced significantly in the past few years. Early and specialised care has been proved to be effective. Early identification of symptoms enables applying specific treatments to selected patients in the first hours after the event.2 The chain of stroke care includes a prehospital-to-hospital and an in-hospital phase.3 Code stroke is a system for patient selection and emergency transferral intended to minimise travel and exploration times, increase the number of cerebral infarct patients treated with thrombolysis, and increase the number of patients with access to care in an acute stroke care unit.4
Between 5% and 15% of all strokes occur in hospitalised patients, who tend to present a poorer functional prognosis and higher mortality rates (up to 54%). These patients often undergo incomplete studies and do not usually benefit from revascularisation therapy during the acute phase, or from the care typically provided by stroke units.5 These patients should be evaluated by a neurologist in a shorter time than non-hospital patients, since hospital arrival times are not an issue. Patients experiencing in-hospital strokes (IHSs) usually present more contraindications for systemic fibrinolysis, but they are potential candidates to receive endovascular treatment.6,7 Previous studies indicate that IHSs are associated with greater delays in performing additional tests and administering fibrinolytic treatment.8 This tendency is explained by the delay in contacting the neurologist and in performing additional tests (fundamentally brain computed tomography [CT]).9 This can be due to an erroneous perception of the urgency and the severity of the stroke on the part of the first professional to evaluate the patient (nursing staff) or the non-neurologist assigned to the patient's case.10 If a stroke occurs in a hospitalised patient, inpatient ward personnel do not know the protocol to follow in most cases of acute stroke. Furthermore, symptoms are often attributed to other causes, since patients may present multiple diseases and greater comorbidity than other stroke patients.11 Training initiatives aimed at medical personnel usually do not address patients who suffer strokes once hospitalised. A national multicentre registry of 273 IHS documented in 13 hospitals showed that emboligenic heart disease and discontinuation of antithrombotics were correlated with IHS. One-third of these patients did not receive neurological care until 6hours after the stroke and 17% did not receive intravenous fibrinolysis for the sole reason of delay in contacting the neurologist.12 Therefore, IHS care should be considered a key target for improving the quality of stroke care overall. Parc de Salut Mar has had a well organised stroke care protocol since 2004, but priority care for IHS was not well defined. To organise IHS care, we conducted a specific theoretical and practical training programme aimed at healthcare professionals from non-neurology departments and who do not normally provide stroke care. Within this organisational system, creating an IHS code for hospitalised patients and providing specific training to staff will improve the quality of care given to IHS patients, especially in the context of a complex institution divided into 4 centres at different locations in the city of Barcelona. The system allows immediate action protocols and specific treatments to be applied as they are in cases of stroke occurring outside the hospital.
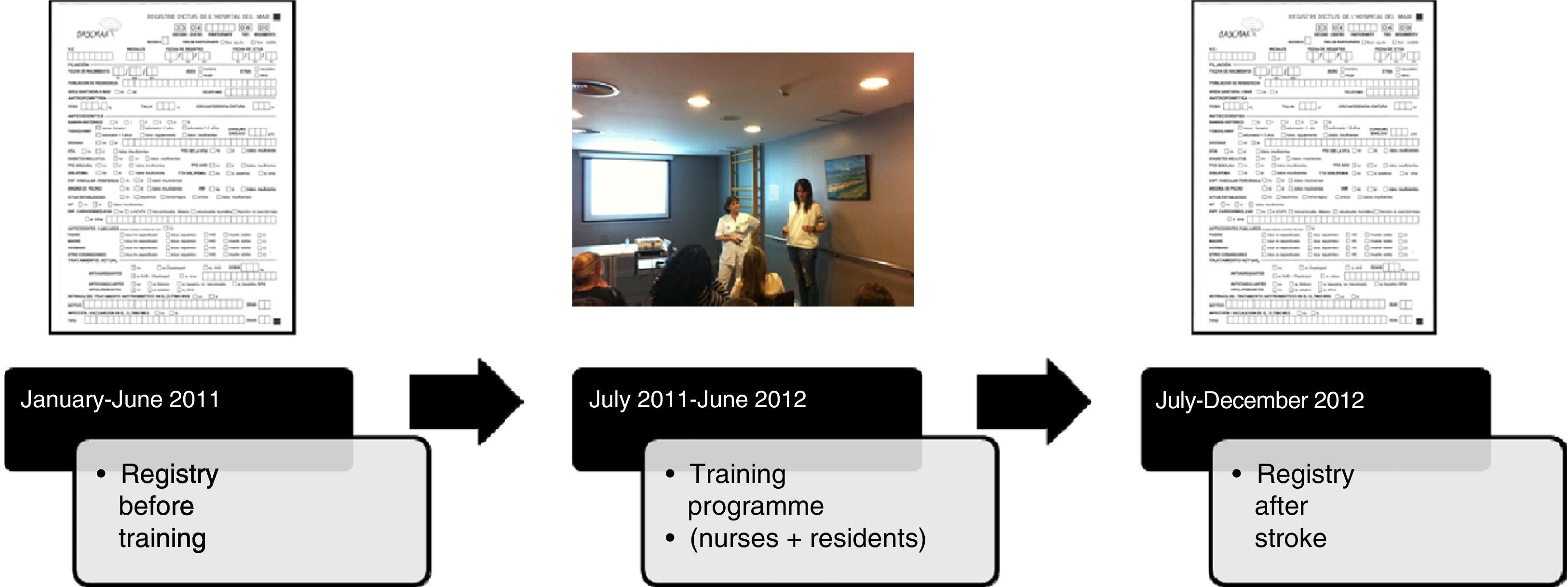
Patients and methodsStudy populationThis is a prospective longitudinal intervention study conducted over 2 years (2011-2012) in the neurology department at Hospital del Mar. Fig. 1 shows a timeline of the study.
Parc de Salut Mar is the only public hospital providing care to the residents of 3 of the 10 health districts in the city of Barcelona, and thus serves a total of 305000 inhabitants. Hospital del Mar is the main healthcare centre in the hospital consortium, and it offers tertiary care to patients with acute stroke. Hospital de Esperança functions as complementary centre to Hospital del Mar, while social healthcare and mental healthcare are provided by Centre Fórum and Centre Dr. Emili Mira. Continuous neurological care and acute-phase treatment are offered by Hospital del Mar exclusively.
A registry of cases of IHS was kept for 6 months to ascertain IHS incidence in Parc de Salut Mar before starting the training programme. This programme was aimed at nursing staff (permanent and substitutes) from different inpatient wards and residents from specialities other than neurology and not usually involved in caring for stroke patients. Nursing assistants could also attend. We excluded the emergency department, the intensive care unit, and the paediatric department, which have specific protocols and are highly specialised; additionally, the patients they admit are unlikely to suffer a cerebrovascular event.
Training was extended to all centres making up Parc de Salut Mar: Hospital del Mar, Hospital de la Esperança, Centre Fòrum, and Centre Dr. Emili Mira.
We designed a specific training programme focusing on knowledge of stroke symptoms and signs, care protocols for acute stroke (in-hospital code stroke), and therapeutic alternatives during the acute stage. This programme was presented as a seminar lasting 1.5hours and covering the following subjects:
- 1.
IHS. Definitions and dimensions of the problem.
- 2.
Identifying strokes. Key warning symptoms. Cincinnati Prehospital Stroke Scale.
- 3.
Transient ischaemic attack: an overlooked emergency.
- 4.
Current treatment possibilities for acute stroke (stroke units, systemic thrombolysis, and intra-arterial thrombolysis).
- 5.
How to act in the event of a suspected IHS.
The seminar was presented by a team consisting of a nurse from the stroke care unit and a neurologist specialising in cerebrovascular disease. Both travelled to each centre to teach nursing staff during different shifts (morning, afternoon, and night). Attendance was compulsory and substitutes were hired to replace those who attended the course. The seminar was presented in a single session for each group, with groups consisting of approximately 15 people. For doctors (residents), a single session was presented at Hospital del Mar, and attendance was voluntary.
One of the training sessions was filmed so that it would be accessible to the largest possible number of professionals from different hospitals through e-learning systems. To this end, we combined the training courses taught in our centre in single virtual file accessible over the Internet via the Parc de Salut Mar virtual school (@pren).
Additionally, we posted informative posters in the inpatient units at each centre. This poster displayed a validated scale with the most frequent symptoms of stroke (Cincinnati Prehospital Stroke Scale),13 the basic initial steps to take in the event of suspected stroke (time of onset, vital signs), and the protocol for activating an IHS code at any of the Parc de Salut Mar hospitals.
Variables analysedIschaemic stroke was confirmed by the on-call neurologist at Hospital del Mar. A CT scan was performed for all patients to rule out other neurological disorders. If ischaemic origin was confirmed, a CT angiography study was performed to confirm arterial occlusion. Patients presenting symptoms more than 4.5hours after onset underwent a multimodal magnetic resonance imaging scan to evaluate diffusion-perfusion mismatch. All patients were prospectively included in the BASICMAR database, a continuous record of patients with acute stroke treated by the neurology department at Hospital del Mar.14
In this study, we included data intended to establish incidence, time to intervention, and treatments administered to IHS patients. We recorded epidemiological data, ward and reason for admission, any previously withdrawn antithrombotic treatments, type of stroke, clinical severity (NIHSS scale15), time for evaluation by the neurology department, (intravenous/intra-arterial) thrombolysis, exclusion criteria for untreated patients, and prognostic data (mortality/disability). Patients with ischaemic stroke at less than 4.5hours from onset were treated with intravenous tissue plasminogen activator (tPA). Exclusion criteria for delivering fibrinolytic treatment were based on the SITS-MOST protocol.16 Patients with progression times of more than 4.5hours, persistent arterial occlusion after intravenous recombinant tPA, or a contraindication for intravenous treatment, underwent intravascular treatment provided there were no contraindications.
Strokes were classified according to the TOAST criteria (Trial of Org 10172 in Acute Stroke Treatment) as atherothrombotic, cardioembolic, lacunar, rare, and of undetermined aetiology.17
Statistical analysisData are presented as mean±standard deviation (SD) or medians with interquartile range (Q1-Q3) for continuous variables, and as frequencies and percentages for categorical variables. We performed a descriptive analysis of data and compared variables from patients observed before and after the training sessions. The t-test and the Chi-square test were used to assess differences between means for continuous variables, and percentages for categorical variables, respectively. SPSS 13.0 software was used for the statistical analysis.
ResultsA total of 564 nurses and nursing assistants completed the training representing 100% of the nursing staff at the inpatient wards at the Parc de Salut Mar hospital consortium. The breakdown by centre was as follows: 213 nurses and 60 nursing assistants from Hospital del Mar; 51 nurses and 9 assistants from Hospital de la Esperança; 144 nurses and assistants from Centre Fòrum; and 87 assistants from Centre Dr. Emili Mira. The training session for doctors was attended by 66 residents of a total of 211 listed in the 2010 resident registry (31.3%).
According to the records taken before training (January-June 2011), we evaluated a total of 232 strokes of which 19 were IHS (8.1%). The training programme was presented at the different centres between July 2011 and June 2012. Records taken after stroke training (July-December 2012) report that out of 273 stroke patients, 41 (15%) had cases of IHS. Therefore, the number of patients recorded as having IHS was higher after training (P=.018). Global incidence of IHS during the 12-month follow-up period was 11.9%.
Regarding stroke type, most of these 60 total cases (19 before and 41 after training) were ischaemic strokes (56 cases, 93%, including 4 transient ischaemic attacks); the remainder were cerebral haemorrhages (4 cases). Stroke type according to the TOAST classification was as follows: 8 atherothrombotic (14%), 25 cardioembolic (45%), 1 lacunar (2%), 9 other (16%), and 13 of undetermined aetiology (23%).
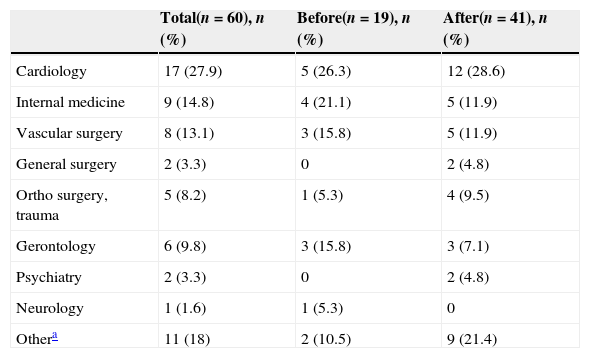
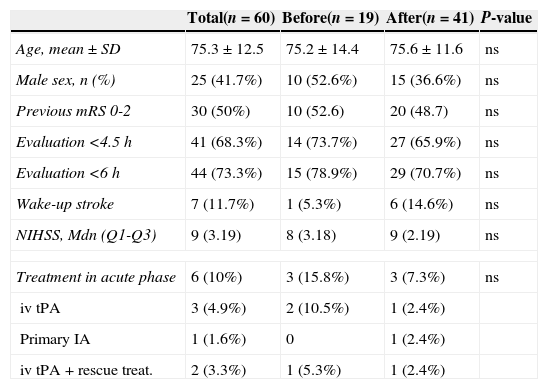
There were no differences between the admitting department distribution between the 2 periods (Table 1). Most patients had been admitted to the cardiology ward, followed by the internal medicine, gerontology, and vascular surgery wards. Table 2 shows the differences between groups treated before and after training regarding demographic data (age, sex, and previous disability), time to evaluation after stroke, clinical severity, and acute-phase treatment. No differences were observed between patients assessed during the 2 periods.
Inpatient units to which patients with IHS were admitted: breakdown before and after training.
| Total(n=60), n (%) | Before(n=19), n (%) | After(n=41), n (%) | |
|---|---|---|---|
| Cardiology | 17 (27.9) | 5 (26.3) | 12 (28.6) |
| Internal medicine | 9 (14.8) | 4 (21.1) | 5 (11.9) |
| Vascular surgery | 8 (13.1) | 3 (15.8) | 5 (11.9) |
| General surgery | 2 (3.3) | 0 | 2 (4.8) |
| Ortho surgery, trauma | 5 (8.2) | 1 (5.3) | 4 (9.5) |
| Gerontology | 6 (9.8) | 3 (15.8) | 3 (7.1) |
| Psychiatry | 2 (3.3) | 0 | 2 (4.8) |
| Neurology | 1 (1.6) | 1 (5.3) | 0 |
| Othera | 11 (18) | 2 (10.5) | 9 (21.4) |
Inter-group differences before and after training regarding demographic data (age, sex, and pre-existing disability), time to evaluation after stroke, clinical severity, and acute-phase treatment.
| Total(n=60) | Before(n=19) | After(n=41) | P-value | |
|---|---|---|---|---|
| Age, mean±SD | 75.3±12.5 | 75.2±14.4 | 75.6±11.6 | ns |
| Male sex, n (%) | 25 (41.7%) | 10 (52.6%) | 15 (36.6%) | ns |
| Previous mRS 0-2 | 30 (50%) | 10 (52.6) | 20 (48.7) | ns |
| Evaluation <4.5h | 41 (68.3%) | 14 (73.7%) | 27 (65.9%) | ns |
| Evaluation <6h | 44 (73.3%) | 15 (78.9%) | 29 (70.7%) | ns |
| Wake-up stroke | 7 (11.7%) | 1 (5.3%) | 6 (14.6%) | ns |
| NIHSS, Mdn (Q1-Q3) | 9 (3.19) | 8 (3.18) | 9 (2.19) | ns |
| Treatment in acute phase | 6 (10%) | 3 (15.8%) | 3 (7.3%) | ns |
| iv tPA | 3 (4.9%) | 2 (10.5%) | 1 (2.4%) | |
| Primary IA | 1 (1.6%) | 0 | 1 (2.4%) | |
| iv tPA+rescue treat. | 2 (3.3%) | 1 (5.3%) | 1 (2.4%) | |
IA: intra-arterial; iv: intravenous; mRS: modified Rankin Scale; Mdn (Q1-Q3): median (interquartile range); NIHSS: NIH Stroke Scale; ns: not significant; tPA: tissue plasminogen activator.
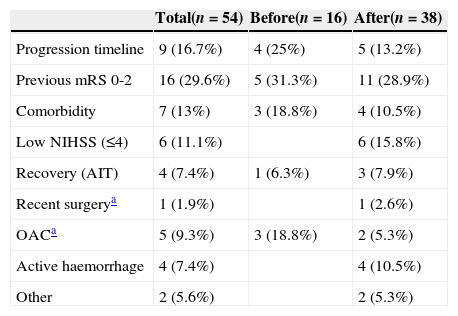
A total of 6 patients received recanalisation therapy during the acute phase (10%), 3 in each period. The percentage of IHS cases out of the total number of recanalisation therapies performed was 6.5% before training and 7.6% after training. Regarding exclusion criteria for administering fibrinolytic treatment, we observed that the main criterion was previous disability in almost 30% of the patients during both periods, followed by progression time (16.7%), comorbidity (10.5%), and symptom severity. Data are included in Table 3. Again, no differences were found between the 2 periods assessed.
Main exclusion criteria for the administration of fibrinolytic treatment during the acute phase.
| Total(n=54) | Before(n=16) | After(n=38) | |
|---|---|---|---|
| Progression timeline | 9 (16.7%) | 4 (25%) | 5 (13.2%) |
| Previous mRS 0-2 | 16 (29.6%) | 5 (31.3%) | 11 (28.9%) |
| Comorbidity | 7 (13%) | 3 (18.8%) | 4 (10.5%) |
| Low NIHSS (≤4) | 6 (11.1%) | 6 (15.8%) | |
| Recovery (AIT) | 4 (7.4%) | 1 (6.3%) | 3 (7.9%) |
| Recent surgerya | 1 (1.9%) | 1 (2.6%) | |
| OACa | 5 (9.3%) | 3 (18.8%) | 2 (5.3%) |
| Active haemorrhage | 4 (7.4%) | 4 (10.5%) | |
| Other | 2 (5.6%) | 2 (5.3%) |
OAC: oral anticoagulants; mRS: modified Rankin Scale; Other: Osler–Weber–Rendu syndrome, diagnostic uncertainty.
Patients’ prognosis regarding disability and mortality was similar in both periods; 41.6% were independent after 3 months, and mortality amounted to 25%.
DiscussionMost hospitals that create protocols for acute stroke treatment have focused on outpatients who actively seek hospital care or are transferred from outpatient clinics. As such, the IHS code is applied exclusively in the emergency department. Acute stroke care is a priority for the neurology department at Parc de Salut Mar. The neurologist takes the lead role from the beginning of the process, allowing him or her to assess all cases and apply specific diagnostic-therapeutic protocols. In addition, nursing staff from the emergency department and stroke unit are directly involved in caring for these patients. Within this organisational system, creating an IHS code for hospitalised patients and offering staff specific training will improve the quality of care given to IHS patients, especially in the context of a complex institution divided into 4 centres at different locations in the city of Barcelona.
This study has evaluated the results from a training programme carried out in the different hospitals belonging to the Barcelona's Parc de Salut Mar consortium. The project lasted 3 years, during which time it took 2 full years to present the training programme to our healthcare personnel (2011-2012). The 100% attendance rate achieved by the nursing staff is a striking figure. It should be recalled, however, that the training took place during normal working hours and substitutes were hired to cover shifts, making attendance more feasible. Attendance by doctors (residents) was lower at 31.3%. We can confirm, based on the records kept for one year, that IHS is frequent in our setting since it represents almost 12% of the total number of acute strokes evaluated in our hospital. This percentage is similar to others reported by previously published series.5,7,18 IHS is frequent in patients who have undergone surgery, experienced potentially iatrogenic procedures (cardiac catheterisation), had their antithrombotic drugs withdrawn, and who have heart disease. This being the case, IHS presents in patients admitted to the cardiology and vascular surgery service, which also explains the higher incidence of cardioembolic stroke in this population; this type is more frequent in patients with a history of heart disease.12
During the study period, no delays in clinical evaluation on the part of the neurology department have been detected that would make it impossible to perform recanalisation treatment during the acute phase. Likewise, the percentages of treatments administered are similar in the 2 periods evaluated (15.8% before training, and 7.3% after training), although both remain lower than the overall rate of fibrinolysis in our centre (18%). Previous studies have shown that longer delays are associated with the detection and evaluation of IHS; only 15% are assessed by a doctor in less than 3hours. Furthermore, despite eschewing travel time to the hospital, some studies have cited a longer door-to-needle time in cases of IHS treated with fibrinolysis.8 This phenomenon was not observed in our series, since almost 70% of the patients were assessed in less than 4.5hours. These data were observed both before and after the training. We believe this achievement may be due to the fact that Parc de Salut Mar is a comprehensive stroke centre. Also, its neurology department, which has had an on-call neurology service since 2001 and a code stroke system since 2004, can ensure prompt acute stroke care and treatment when the event is identified early on. Furthermore, departments with a higher incidence of IHS, and which work closely with the neurology department, are more aware of the possibility of stroke in their patients. Their staff (doctors and nurses) usually contact the neurologist promptly if they detect warning symptoms. Those departments less familiar with stroke detection were the ones to activate more IHS codes after training, while this parameter remained largely unchanged in departments with a higher incidence of stroke. Therefore, we suggest that a specific training programme focusing on these departments could be particularly useful to promote the early detection of IHS cases.
The main limitation of our study is that IHS patients were evaluated in only one of our hospitals, during a very short time period (6 months for each group). This makes it difficult to find statistically significant differences between the ‘before’ and ‘after’ groups. The patient total was also characterised by a high percentage of pre-existing disability and comorbidity which would also be likely to affect these results. It would be very difficult to repeat the programme in the future, whether in our institution or at another hospital, since it requires substantial financial outlay to employ substitute staff and thereby ensure attendance. Furthermore, the lecturers need to make a considerable effort, basically referring to time spent travelling to the different centres, and because they are required to teach during different shifts for a total of 4 to 6hours daily.
Knowledge acquired by the attendees could not be evaluated objectively. All attendees were surveyed about their knowledge on acute stroke before they attended the sessions. This survey was distributed again 6 months after training to detect any improvements. However, since only a small minority of the attendees filled out the survey after training (only 22%), comparing knowledge between the 2 periods was not possible.
We believe that defining a care protocol for each of these separate centres and providing graphic reference material to all inpatient wards, making it available to all staff, constitute progress. Although we did not obtain direct results, we highlight our interaction with staff from the different centres and the satisfaction of having provided a solid training programme which contributed to the knowledge, motivation, and capability of healthcare personnel faced with such a prevalent entity as acute cerebrovascular event.
We conclude that the IHS training programme conducted in the Parc de Salut Mar hospitals has significantly increased the number of IHS codes activated for its patients. However, during the period evaluated here, this initiative did not result in a higher percentage of patients receiving treatment during the acute phase or in any improvements in functional prognosis.
FundingThis project was financed by the Programa de Calidad del Parc de Salut Mar in its 2010 call for projects Projectes de Millora de Qualitat.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Rodríguez Campello A, Cuadrado Godia E, Giralt Steinhauer E, Rodríguez Fernández E, Domínguez A, Romeral G, et al. Detección de ictus intrahospitalario: evaluación de resultados de un programa de formación y entrenamiento a personal médico y de enfermería. Neurología. 2015;30:529–535.
This study was presented orally at the 65th Annual Meeting of the Spanish Society of Neurology (2013).