Fibrinolysis with recombinant tissue plasminogen activator (rt-PA) improves stroke prognosis when administered within the first 4.5hours of the ischemic event. The treatment is contraindicated in certain clinical situations, however, such as in early recurrence of stroke. According to recently published clinical trials,1–5 intra-arterial mechanical thrombectomy after thrombolysis in proximal occlusions of intracerebral arteries achieves higher reperfusion rates and results in fewer clinical sequelae than thrombolysis alone. However, there is still little evidence on the feasibility and safety of this treatment for patients experiencing early recurrence of ischemic stroke. We describe the case of a patient undergoing 2 mechanical thrombectomies in 28hours due to reocclusion of the right middle cerebral artery (MCA).
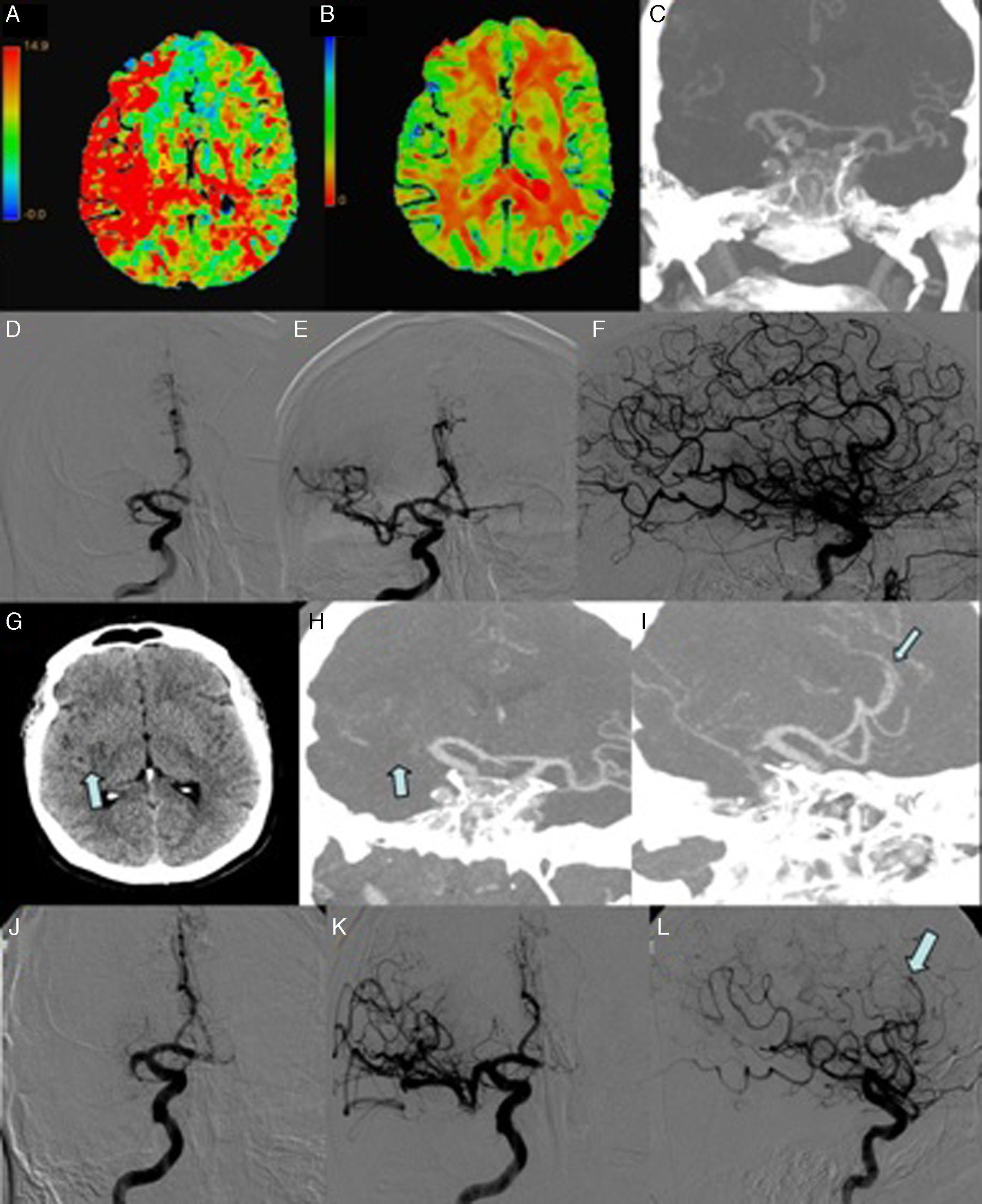
Our patient, a 58-year-old man, was an obese former smoker who experienced sudden-onset left hemiparesis and hemihypaesthesia (NIHSS=13). A de novo atrial fibrillation (AF) was detected during the patient's transit to hospital. AF spontaneously reverted to sinus rhythm. A CT scan performed upon the patient's arrival at hospital revealed no anomalies. Fibrinolysis was started 75minutes from symptom onset, with no improvement. The patient was consequently transferred to our hospital to be evaluated for eligibility for neurosurgery. A brain CT-angiography detected a proximal occlusion of the right MCA (Fig. 1A-F). We conducted an arteriography; recanalisation was achieved using a stent retriever (TICI grade 3; time to recanalisation: 240minutes). Our patient experienced no neurological sequelae 24hours after the procedure and displayed sinus rhythm during monitoring. A follow-up CT scan performed 24hours after thrombolysis revealed a hypodense lesion in the right insula and lenticular nucleus; intravenous heparin was administered as secondary prevention.
First ischemic stroke (A-F). (A) Multiparametric CT scan: map of mean transit time showing delayed blood flow in the territory of the right MCA. (B) Multiparametric CT scan: map of cerebral blood volume revealing low volume in the right lenticular nucleus. (C) CT-angiography: occlusion of the M1 segment of the right MCA. (D) Angiography: occlusion of the M1 segment of the right MCA. (E and F) Complete recanalisation (TICI grade 3) was achieved with 2 passes. 28hours after the first event (G-L). (G) Brain CT scan showing a small infarction in the right insula and lenticular nucleus (arrow). (H) CT-angiography: occlusion of the M1 segment of the right MCA (arrow). (I) CT-angiography: occlusion of the A3 segment of the right ACA (arrow). (J) Angiography (AP projection): occlusion of the M1 segment of the right MCA. (K and L) Recanalisation of the MCA (TICI grade 2B) and persistent occlusion of the A3 segment of the right ACA (arrow).
Twenty-eight hours after the first recanalisation procedure, and coinciding with an episode of AF, our patient displayed sudden-onset left hemiparesis, hemihypaesthesia, and hemianopsia (NIHSS=14). A multiparametric CT scan revealed reocclusion of the right MCA and a favorable mismatch (Fig. 1G-L). A second mechanical thrombectomy achieved recanalisation (TICI grade 2B; time to recanalisation: 150minutes). An occlusion in a distal branch (A3) of the right anterior cerebral artery (ACA) was detected but not treated. The second procedure achieved less satisfactory results (NIHSS=6 at 24 hours); a follow-up brain CT scan revealed an increase in the volume of the previously detected ischemic lesion, affecting the right internal capsule.
We resumed anticoagulation with intravenous heparin 3 days after the second episode. A transthoracic echocardiogram revealed moderate ventricular dysfunction (LVEF=35%) and posterior-inferior hypokinesia.
The rate of early recurrence of cerebral infarction depends on stroke etiology. Very early recurrence of thromboembolic events has been observed in prothrombotic states caused by malignant processes.6 In our patient, reocclusion occurred at 28hours from the first recanalisation procedure; this recurrence is considered to be “early” for cardioembolic stroke, given that the risk of recurrence in these patients is approximately 6.9% in the first 2 weeks, with a mean time to recurrence of 12 days.7
In view of the small size of the first infarction and the fact that our patient had no hemorrhagic complications, we started anticoagulation treatment according to the most recent American Heart Association stroke prevention guidelines.8 We opted for intravenous unfractionated heparin, given its rapid anticoagulation effects and good safety profile. For these 2 reasons (early recurrence and anticoagulation), fibrinolytic treatment was contraindicated in the second stroke episode. Therefore, and given the presence of an intracerebral proximal occlusion, thrombectomy was found to be the only treatment alternative.
Very few cases similar to ours have been published in the literature, which may reflect a publication bias (cases with less favorable results may have not been published). In fact, to our knowledge only 2 published cases have described the potential benefits of repeated mechanical thrombectomy during the acute phase of stroke.9,10 Laible et al.10 described the case of a patient undergoing thrombectomy for the second time in 24hours due to a prothrombotic state. Lee et al.,9 in turn, published the case of a patient with AF who experienced a recurrence 6 days after the first procedure; this was successfully managed with repeated mechanical thrombectomy.
In our case, reocclusion was treated with a second thrombectomy; the second cardioembolic stroke was managed at an earlier stage, resulting in an acceptable clinical outcome and no complications associated with the procedure. Our case suggests that mechanical thrombectomy is a safe procedure for patients experiencing early stroke recurrence, leading to more favorable functional outcomes in a group of patients with no other treatment alternatives.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Quintas S, López Ruiz R, Ximénez-Carrillo Á, Zapata-Wainberg G, Gilo F, Bárcena-Ruiz E, et al. Recurrencia precoz de infarto cardioembólico tratada con éxito mediante una segunda trombectomía. Neurología. 2017;32:551–554.
This case report was presented in the outstanding posters section at the 67th Annual Meeting of the Spanish Society of Neurology under the title “Doble intervencionismo: tratamiento de un reinfarto precoz” (repeated thrombectomy for early recurrence of stroke).