Endovascular therapies (intra-arterial thrombolysis and mechanical thrombectomy) after acute ischaemic stroke are being implemented in the clinical setting even as they are still being researched. Since we lack sufficient data to establish accurate evidence-based recommendations for use of these treatments, we must develop clinical protocols based on current knowledge and carefully monitor all procedures.
DevelopmentAfter review of the literature and holding work sessions to reach a consensus among experts, we developed a clinical protocol including indications and contraindications for endovascular therapies use in acute ischaemic stroke. The protocol includes methodology recommendations for diagnosing and selecting patients, performing revascularisation procedures, and for subsequent patient management. Its objective is to increase the likelihood of efficacy and treatment benefit and minimise risk of complications and ineffective recanalisation. Based on an analysis of healthcare needs and available resources, a cooperative inter-hospital care system has been developed. This helps to ensure availability of endovascular therapies to all patients, a fast response time, and a good cost-to-efficacy ratio. It includes also a prospective register which serves to monitor procedures in order to identify any opportunities for improvement.
ConclusionsImplementation of endovascular techniques for treating acute ischaemic stroke requires the elaboration of evidence-based clinical protocols and the establishment of appropriate cooperative healthcare networks guaranteeing both the availability and the quality of these actions. Such procedures must be monitored in order to improve methodology.
El tratamiento endovascular (trombólisis farmacológica intraarterial y trombectomía mecánica) en el ictus isquémico agudo se está implantando en la práctica clínica cotidiana, aunque continúa en desarrollo su investigación. En ausencia de datos suficientes que permitan fundamentar sólidamente las recomendaciones para su uso, es necesario elaborar protocolos de actuación basados en el conocimiento acumulado, así como monitorizar las actuaciones.
DesarrolloTras revisión bibliográfica, en reuniones de trabajo de expertos para llegar a un consenso, se ha elaborado un protocolo de actuación que incluye indicaciones y contraindicaciones para la aplicación de tratamiento endovascular y recomendaciones referentes a la metodología de diagnóstico y selección de los pacientes, de los procedimientos de revascularización y manejo posterior, con el objetivo de incrementar las probabilidades de eficacia y beneficio del tratamiento y minimizar los riesgos de complicaciones y de recanalización fútil. En función del análisis de las necesidades asistenciales y los recursos disponibles se ha elaborado un sistema organizativo de colaboración interhospitalaria, para asegurar la accesibilidad al tratamiento garantizando el menor tiempo de respuesta y una relación coste/eficacia favorable. Incluye un registro prospectivo común con fines de monitorización para detectar oportunidades de mejora.
ConclusionesPara la implantación de técnicas endovasculares de tratamiento del ictus isquémico agudo es imprescindible la elaboración de protocolos de actuación basados en las evidencias disponibles y el establecimiento de sistemas adecuados de organización asistencial para garantizar el rigor y la eficacia de las actuaciones. Es necesario monitorizar los procedimientos con el fin de optimizar la metodología.
Early reperfusion of ischaemic tissue is one of the main objectives in treating acute ischaemic stroke. Today, this statement is much more than a theoretical guideline. Studies have fully demonstrated that this can be achieved and that progress among patients with early reperfusion is significantly better than in those without.
Systemic intravenous thrombolysis (SIT) with intravenous tissue plasminogen activator (IV-tPA) has been shown to be effective in stroke patients with no contraindications if delivered in the 4.5hours after an acute ischaemic stroke. The procedure is currently used in daily clinical practice. The fundamental limitations of this treatment are its narrow therapeutic window and the fact that it is less effective in cases of large-vessel occlusions (internal carotid, initial segment of the medial cerebral artery, basilar artery) or large thrombi. In addition, it is contraindicated in patients whose characteristics indicate a higher risk of haemorrhagic complications.1–7
Different endovascular therapies (EVT) have been developed in order to recanalise arteries using endovascular approaches. These approaches include pharmacological intra-arterial thrombolysis (IAT) and mechanical thrombectomy (MT) with different extraction devices.8–10 The principal objective is to achieve more effective recanalisation by acting in situ (especially for large vessel occlusions), decreasing haemorrhagic complications, and widening the window of opportunity for the intervention. This is intended to make the treatment effective in a larger number of patients. Theoretical advantages aside, the shortcomings of endovascular therapy are that the technique is more complex, requires more time to perform, and incurs a risk of intraoperative complications. It is also possible to obtain a result with a good radiological appearance but no clinical benefit (futile recanalisation).11,12 Strict and appropriate patient selection is needed in such cases in order to provide a favourable risk–benefit ratio. The definition of the selection criteria may be affected not only by the time factor and by clinical data such as age or stroke severity,11 but also by factors that let doctors identify persistence of viable tissue (penumbra) and the presence of effective collateral circulation. This is done using multimodal neuroimaging techniques.7,13–15
Two clinical trials studying pharmacological thrombolysis using recombinant prourokinase16,17 and some case series with rtPA18–20 show that these agents induce recanalisation effectively when applied by the intra-arterial route (IA). Treated patients in these studies showed better clinical progress than controls (40%–49% vs. 25%–39%). The window of opportunity for this treatment is 6hours in the anterior territory and up to 24hours in the posterior territory.9 However, only the PROACT II study17 found that IAT contributed significantly to better progress for patients. A meta-analysis of available studies shows that IAT increases the recanalisation rate and the figures for good clinical progress. It also increases the frequency of haemorrhagic complications, but not the mortality rate.8 Studies have not yet been able to show that IAT is more effective than intravenous thrombolysis (IVT), although some suggest this is the case.20 This claim has been linked to the fact that patients are treated later and suffer more severe effects due to having large-vessel occlusions.
Some series and one meta-analysis show that administering thrombolytic agents through an IA line after a failed IVT is a safe and effective method for recanalisation. However, the level of evidence is insufficient to prove this technique more clinically effective than another.21–25 Combination therapy (IVT followed by pharmacological EVT or better yet, MT) in selected cases of IVT failure seems to be a reasonable option. This is especially true when we consider that being able to use endovascular treatment is no reason to rule out IVT if the patient is within the time window and there are no contraindications.26 Studies are currently underway to evaluate this combination. The IMS III study was recently halted due to futility, but its definitive results have yet to be published.27
MT achieves a recanalisation rate of 45% to 82% depending on the device used, and it can be combined with locally administered thrombolytic drugs.28–32 Studies show a higher probability of good outcomes among patients whose recanalisation procedure was satisfactory, although as a whole, the percentage of patients with favourable outcomes is no higher than among patients treated with IAT or IVT. Nevertheless, we should be aware that the latter group's prognosis is necessarily poorer, given that all have large vessel cerebral occlusions, a more severe clinical status with higher scores on the NIHSS, and that they are generally treated at a later time. MT studies are associated with symptomatic haemorrhages in up to 10% of the cases, with mortality rates as high as 34%. The therapeutic window in these cases is up to 8hours for the anterior territory and as much as 24hours in the posterior territory.9,10,26,33
Although available evidence is based on only a few randomised clinical trials, small series, and prospective databases, EVT seems to be a promising alternative, and its use is growing in clinical practice.34,35 However, the effectiveness of this treatment is still under investigation, and many points have yet to be clarified. As stated before, doctors require reliable criteria that will allow them to predict which patients will benefit from treatment and which will not in order to manage risks while making the process more cost-effective. With this in mind, we must establish action protocols requiring that treatments be carried out only in those hospitals with experience and the necessary equipment (stroke unit and vascular surgery operating room). We must also set up inter- and intrahospital cooperative networks to guarantee that all patients who may benefit from these therapies will be treated in those hospitals on an emergency basis. Such systems will respond correctly to the needs of the population according to the available resources.36,37 It is also necessary to keep common databases to record all cases, procedures, and complications. This way, doctors can monitor the effectiveness of the intervention and improve the protocol as needed.
The goal of organising an on-call neurointerventional network will only be achieved through good planning and cooperation among hospitals aimed at guaranteeing that endovascular treatment will be available in a specific health district. The protocol we present was prepared for this purpose.
DevelopmentThis endovascular treatment protocol for acute ischaemic stroke is the result of cooperation between neurologists pertaining to the Madrid Association of Neurology's Stroke Forum and interventional neuroradiologists in Madrid-area hospitals. It was drawn up within the framework of Madrid's regional stroke care plan, and it is supported by that plan's inter-hospital coordinated care network.37
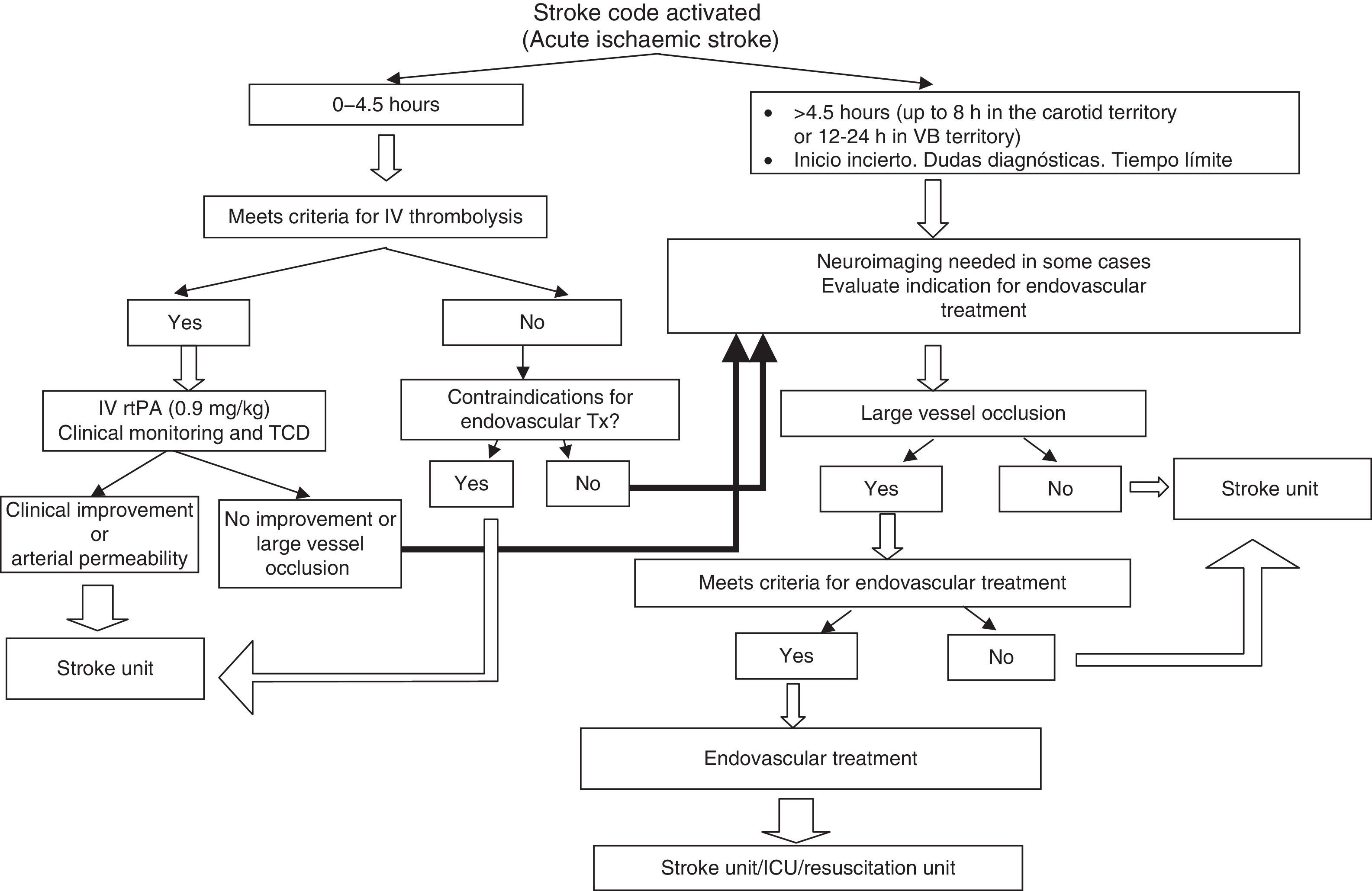
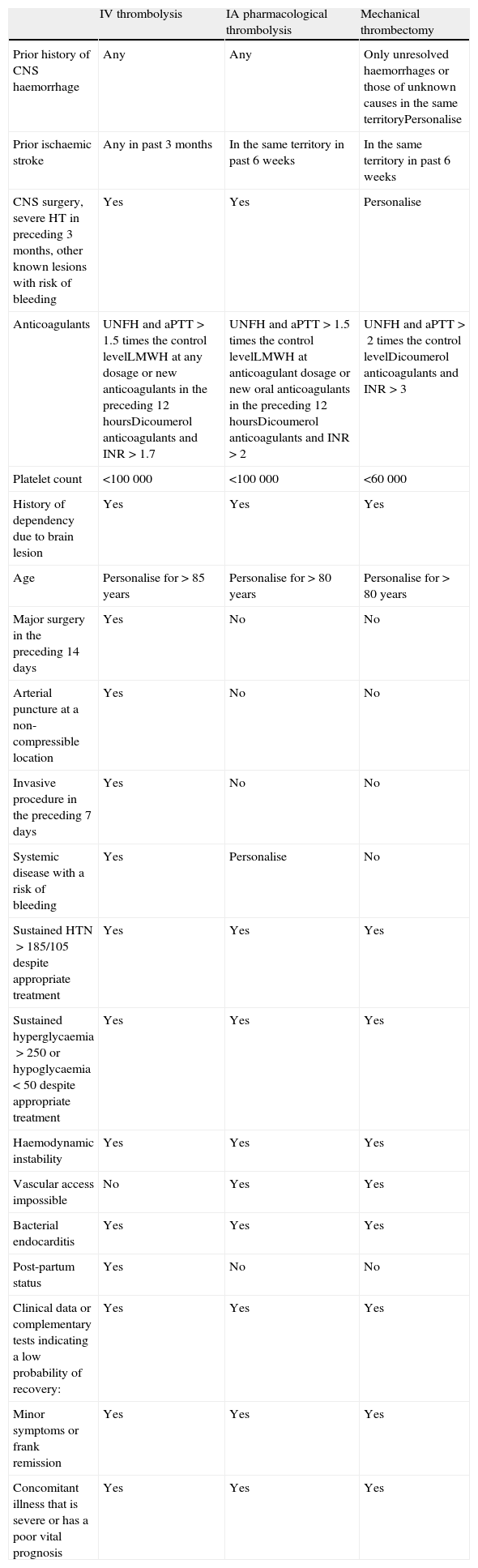
The protocol is based on evidence discovered in a review of the most relevant literature, and it was written in working sessions held by the Drafting Committee. Drafts were then discussed by the Ad Hoc Committee to reach the final consensus that is reflected in this copy. Indications and contraindications for administering treatment are included (Table 1). The study also presents recommendations for diagnostic methods and patient selection, a flowchart for decision-making (Fig. 1), recommendations for revascularisation procedures, and a common prospective database including all subjects for whom treatment was authorised in order to monitor the process as a whole. Experts established indications and contraindications that would increase the procedure's probability of being effective and beneficial and minimise the risk of complications and the probability of futile recanalisation.
Contraindications for different revascularisation procedures in acute ischaemic stroke treatment.
| IV thrombolysis | IA pharmacological thrombolysis | Mechanical thrombectomy | |
| Prior history of CNS haemorrhage | Any | Any | Only unresolved haemorrhages or those of unknown causes in the same territoryPersonalise |
| Prior ischaemic stroke | Any in past 3 months | In the same territory in past 6 weeks | In the same territory in past 6 weeks |
| CNS surgery, severe HT in preceding 3 months, other known lesions with risk of bleeding | Yes | Yes | Personalise |
| Anticoagulants | UNFH and aPTT>1.5 times the control levelLMWH at any dosage or new anticoagulants in the preceding 12 hoursDicoumerol anticoagulants and INR>1.7 | UNFH and aPTT>1.5 times the control levelLMWH at anticoagulant dosage or new oral anticoagulants in the preceding 12 hoursDicoumerol anticoagulants and INR>2 | UNFH and aPTT>2 times the control levelDicoumerol anticoagulants and INR>3 |
| Platelet count | <100000 | <100000 | <60000 |
| History of dependency due to brain lesion | Yes | Yes | Yes |
| Age | Personalise for>85 years | Personalise for>80 years | Personalise for>80 years |
| Major surgery in the preceding 14 days | Yes | No | No |
| Arterial puncture at a non-compressible location | Yes | No | No |
| Invasive procedure in the preceding 7 days | Yes | No | No |
| Systemic disease with a risk of bleeding | Yes | Personalise | No |
| Sustained HTN>185/105 despite appropriate treatment | Yes | Yes | Yes |
| Sustained hyperglycaemia>250 or hypoglycaemia<50 despite appropriate treatment | Yes | Yes | Yes |
| Haemodynamic instability | Yes | Yes | Yes |
| Vascular access impossible | No | Yes | Yes |
| Bacterial endocarditis | Yes | Yes | Yes |
| Post-partum status | Yes | No | No |
| Clinical data or complementary tests indicating a low probability of recovery: | Yes | Yes | Yes |
| Minor symptoms or frank remission | Yes | Yes | Yes |
| Concomitant illness that is severe or has a poor vital prognosis | Yes | Yes | Yes |
LMWH: low molecular weight heparin; UNFH: unfractionated heparin; IA: intra-arterial; IV: intravenous; HTN: hypertension; CNS: central nervous system; HT: head trauma; aPTT: activated partial thromboplastin time.
Candidates for endovascular treatment (IAT and/or MT) are those patients with the following conditions and none of the contraindications listed in the subsequent section:
- 1.
Acute ischaemic stroke caused by demonstrated occlusion of one or more large-calibre cerebral arteries (internal carotid, trunk of the middle cerebral artery [M1, M2], basilar artery; if other large-calibre arteries are occluded [ACA or PCA], the indication will be determined based on the individual's clinical profile).
- 2.
Moderate to severe neurological deficit (this criterion should be adjusted according to the effect of the deficit on the patient).
- 3.
Subjects presenting one or more of the following conditions:
- 3.1
Time after event greater than 4.5hours.
- •
For hemispheric strokes, the upper limit is 8hours.
- •
The upper limit for occlusion of the basilar artery is 12hours in cases with established maximum deficit following the vascular event, and 24hours for fluctuating or progressive-onset cases.
- •
- 3.2
Intravenous thrombolysis is contraindicated in all of the following situations:
- •
Patient on heparin anticoagulant treatment whose partial thromboplastin time>1.5 times the control level and who has taken LMWH or new oral anticoagulants in the previous 12hours; patient treated with dicoumerol derivative with an INR>1.7.
- •
Platelet count<100000.
- •
Recent history of major surgery (14 days).
- •
Recent arterial puncture in a non-compressible site or recent surgery (7 days).
- •
Systemic disease with a risk of bleeding.
- •
Stroke in the preceding 3 months.
- •
Post-partum status.
- •
Prior history of central nervous system haemorrhage.
- •
Other.
- •
- 3.3
IVT failure (persistence of the arterial occlusion and neurological deficit) within the therapeutic window for an endovascular procedure.
- 3.1
Table 1 summarises the contraindications for each of the different reperfusion treatments (IVT, IAT, MT). Below, we list specific contraindications for endovascular procedures.
General contraindications for any endovascular procedure- •
Haemorrhagic stroke
- •
Old age as a contraindication may be waived depending on the patient's condition. Patients younger than 80 are generally considered candidates. Procedures are performed with caution in patients older than 80, since their probability of a favourable outcome will be significantly lower.
- •
Dependent status (EmR≥3 due to prior cerebral injury).
- •
History of dementia or severe concomitant illness or disease with a poor short-term vital prognosis.
- •
Treatment would be administered outside of time limits listed above.
- •
Absence of large-vessel arterial occlusion.
- •
Clinical data or complementary tests indicating small to no chance of recovery:
- a.
Established severe deficit (NIHSS>25, except in posterior territory stroke, prolonged coma (>6hours) or complete and persistent abolition of brainstem reflexes.
- b.
Neuroimaging scans show evidence of there being no recoverable tissue (one or more of the conditions listed below are met).
- b.1
Within the therapeutic window:
- 1.
Patients with a CT revealing frank hypodensity covering more than a third of the middle cerebral artery territory.
- 2.
ASPECTS<7 in simple CT.
- 3.
In posterior stroke, CT or MRI evidence of an extensive lesion in the brainstem.
- b.2
Time since onset unknown or at the limit (in addition to the information in the previous section, the following may be useful for decision-making).
- 4.
Patients with diffusion-weighted MRI sequences showing lesions that cover more than two-thirds of the affected artery's territory.
- 5.
Discrepancy of less than 20% between flow and tissue damage parameters according to perfusion-weighted CT or diffusion/perfusion-weighted MRI.
- 1.
- b.1
- •
Lessening or frank improvement of symptoms before the procedure can be started, and absence of confirmed arterial occlusion.
- •
Extensive ischaemic stroke in the same vascular territory in the 6 preceding weeks (a stroke in another territory would not contraindicate endovascular treatment).
- •
Arterial hypertension above 185/105mm Hg at the start of the procedure and which does not respond to appropriate treatment.
- •
Hyperglycaemia>250mg/dL or hypoglycaemia<50mg/dL persisting despite proper treatment.
- •
Haemodynamic instability.
- •
Vascular access impossible.
- •
Bacterial endocarditis.
- a.
- •
Prior history of intracranial haemorrhage (mechanical thrombectomy is an option for patients with a prior haemorrhage of known aetiology that resolved completely with treatment, or haemorrhage in a different vascular territory).
- •
Recent CNS surgery or severe head trauma in the preceding 3 months.
- •
Known CNS lesion with a risk of haemorrhage (aneurysm, AVM). In such cases, the decision to perform mechanical thrombectomy should be made on an individual basis.
- •
Vasculitis.
- •
Platelet count<100Y000/mm3.
- •
Treatment with heparin and aPTT>1.5 times the control level, treatment with LMWH at anticoagulant doses, treatment with non-dicoumarol oral anticoagulants in the preceding 12hours, or treatment with dicoumarol anticoagulants and INR>2.
- •
Platelet count<60000/mm3.
- •
Treatment with heparin and aPTT>2. Treatment with oral anticoagulants and INR>3.
Decision-making in high risk situations should be done on a case-by-case basis, taking additional parameters into account and using specific treatment measures to prevent complications.
- •
Pregnancy.
- •
Allergy to contrast material.
- •
Kidney failure.
The stroke code protocol will be activated for all patients with acute stroke at less than 8hours after onset.36,37
Patients with acute stroke will be evaluated by the on-call neurologist in the emergency department according to that hospital's protocols.37
- •
The medical history will contain time of symptom onset, concomitant treatments and previous illnesses, comorbidities, and baseline condition. The NIHSS score and the patient's weight will be recorded after examination.
- •
All patients will be studied with a full blood count, clinical biochemistry and coagulation tests, and an ECG. Vital constants will be monitored and any changes in glycaemia, blood pressure, oximetry, and temperature will be treated to maintain values within recommended limits.2,33
- •
All patients will undergo such emergency neuroimaging studies as are deemed necessary for the case. Objectives are as follows: apply necessary treatment as early as possible and correctly identify patients who may be candidates for endovascular surgery.
- •
All patients will undergo simple CT on an emergency basis.
- •
Assessment of the arterial occlusion by means of a neurovascular sonography study (Doppler or duplex transcranial and supra-aortic trunk studies), CT, D-SAT; or non-invasive angiography (CT or MR angiography).
- •
Non-invasive angiography should generally be performed prior to interventional procedures, but if this is not possible, a neurovascular sonography study may be sufficient to demonstrate arterial occlusion.
- •
Perfusion CT or MRI with diffusion/perfusion-weighted sequences. These techniques are necessary for selecting cases in special circumstances, such as those in which time of onset is undetermined or those at the therapeutic time limit. They are not strictly necessary within the therapeutic time limit, but they may be performed, provided they do not delay treatment, as an aid to selecting patients with a penumbra covering more than 20% of the territory of the affected artery, or excluding those with no evidence of viable tissue. We must be aware that a perfusion/diffusion mismatch is not necessarily useful for selecting patients for endovascular treatment.
If EVT is indicated due to IVT failure, the procedure must be initiated with no unnecessary delays. To this end, we recommend monitoring the arterial occlusion as intravenous treatment is being administered; if large-vessel occlusion persists and there is no clinical improvement 30minutes after treatment, doctors should activate the EVT protocol.
Technical procedureThe revascularisation procedure and its management will be adjusted to each individual case. This will be a joint decision made by the neurology and neuroradiology teams.
An anaesthetist will be required to administer the type of sedation or anaesthesia deemed appropriate for each case. Sedation is generally preferred to anaesthesia provided that the patient will be able to cooperate and remain still.
Post-treatment actionsOnce the procedure has been completed, the patient will be transferred to the stroke unit, or else to the ICU/critical care unit if anaesthesia or intubation was used, or if the patient has haemodynamic instability or impaired breathing.
Patient care will then follow stroke-unit protocols for patients with acute stroke.2,33
Setting up a coordinated care systemPublic healthcare systems with limited resources must impose cost-efficient care strategies.36,38 Obtaining the most advanced technology for all hospitals is not a sustainable approach, and therefore healthcare professionals and government authorities must come together to analyse the population's care needs and tailor resources to meet those needs. Although we lack precise data required to determine exactly how many patients in the Madrid Region would be candidates for EVT, an estimate can be prepared using hospital records. The conclusion is that 2 centres of reference performing EVT every day would be sufficient. To ensure equal care for the entire population, care networks promoting inter-hospital cooperation would be needed to guarantee that all patients would have access to this resource, under optimum conditions, 24hours a day and 365 days a year. An on-call interventional schedule with weekly rotations between 3 hospitals has been set up. This was made possible thanks to a protocol ensuring that treatment would be provided uniformly; it was established by consensus of all hospitals in Madrid with EVT capability. The purpose of this coordinated care system is to lower response time as much as possible in order to indicate and apply treatments with no unnecessary delays. As a result, proper selection and management of the patient in the on-call interventional hospital will be a top priority.
Staff from neurology and neurointerventional units and hospital administrators have coordinated the activities of necessary personnel and arranged on-call schedules outside of normal working hours according to needs and available resources in order to meet the goal described above. Meanwhile, non-hospital emergency services (paramedics and first responders) actively participate in this organisational system by guaranteeing immediate patient transfers and patient management according to the established protocols.37
The patient is first examined by a neurologist at a stroke-unit hospital and identified as a candidate for EVT according to inclusion/exclusion criteria and results from any pertinent complementary tests. The hospital on call for EVT will then be notified, and the first neurologist will reach an agreement with the on-call hospital's neurologist and interventional neuroradiologist regarding treatment indication and transferring the patient. If the second team is not at the same hospital as the patient, informed consent is needed before the patient can be transferred. The team performing EVT will obtain the informed consent for the procedure itself. Non-hospital emergency services assign top priority to these transfers, which make use of life support ambulances. The on-call hospital will also receive a copy of all documents, including the informed consent sheet for transferring the patient to that hospital. The treating hospital will be responsible for gathering data for the database.
All tests performed must be made available to the neurology–neuroradiology team at the receiving hospital (via the simplest method in each case: digital files, photographic film, web access, etc.). The team at the receiving hospital will then determine if any complementary tests should be repeated, while avoiding any unnecessary treatment delays.
All hospitals’ computer systems and communications will be made web-accessible so that doctors can view complementary test results while making decisions as members of an inter-hospital committee. Implementing effective telemedicine (‘telestroke’) programmes may also help with patient selection.38
The patient's return to the referring hospital should be coordinated once the procedure is complete and the patient is stable, usually within 24hours. This prevents saturation of the on-call hospital so that it can continue providing service.
DiscussionEVT is a treatment alternative that is used increasingly by experienced teams of neurologists and interventional neuroradiologists in order to achieve reperfusion of brain tissue and reduce morbidity and mortality associated with acute ischaemic stroke. It has been shown to be feasible, effective, and safe in selected patients.9,26,34,35
Given its status as a new technique, however, it is still undergoing research and technical development.10 In addition to devising safer and more effective extraction devices, this development aspect includes processes such as selecting patients according to criteria that go beyond age, profile, and time since onset. More advanced criteria would provide doctors with a more reliable idea of which subjects would benefit from treatment and which subjects might experience treatment failure or be at risk for complications.11,12 These criteria are established in order to identify potentially salvageable tissue (ischaemic penumbra), and they are based on new imaging techniques, the size of the thrombus and the affected blood vessel, and collateral circulation measurements.7,13,14
Implementing techniques that are both complex and evolving will require proper training of the healthcare professionals involved, as well as the creation of protocols based on available evidence. Compliance with these protocols will ensure strict and unvarying criteria for patient selection and treatment administration. The end goal will be to obtain desired benefits for patients while minimising both risks and costs.
Since clinical trials have not yet clarified a number of uncertain points, all activity must be documented in exhaustive prospective databases. Analysis of these databases will therefore allow doctors to monitor and improve procedures, and promote the scientific advances that will be needed to clear up unanswered questions. Experience in this field is growing as results from monitoring procedures accumulate; techniques are being improved and so are selection criteria. As a result, protocols that are in use today are likely to undergo modifications.
These complex, costly procedures cannot be carried out in all hospitals, so they must be performed in hospitals with stroke units and the necessary technical equipment and staff. These hospitals should be well-equipped and there must be enough of them to meet the needs of the districts they serve. In any case, limiting the number of hospitals cannot result in limiting access to them. Coordinated care systems must be developed to ensure that all patients with acute-phase stroke who may benefit from EVT will receive an assessment and specific treatments on an emergency basis, regardless of their place of residence. If such care systems are to be established, health authorities and healthcare professionals must come together to correctly analyse patients’ needs and allot the necessary resources.10,37,39 This will involve informing the population, training emergency service professionals at both hospital and non-hospital levels, and setting up a functional network of hospitals connected by good communication systems to permit inter-hospital consults and rapid, smooth patient transfers. Lastly, emergency transport must be organised such that personnel understand that transfers are top priority and know which hospital's neurointerventional team is on call and will be receiving each patient according to established criteria.
ConclusionImplementing endovascular techniques for treating acute ischaemic stroke will require action protocols based on available evidence. It also calls for well-designed healthcare coordination systems that make EVT accessible to everyone and monitor procedures to ensure their methodological rigour, effectiveness, and safety.
Conflicts of interestThe authors have no conflicts of interest to declare.
We would like to thank the following people for their input and comments in work sessions: Yolanda Aladro (Hospital Universitario de Getafe), Aitziber Aleu, Javier Barriga (Hospital de Fuenlabrada), Julio Domingo (Hospital Universitario Severo-Ochoa), María Araceli Gartia (Hospital Universitario Príncipe de Asturias), Carlos Gómez-Escalonilla (Hospital Universitario Clínico San Carlos), Raquel González (Hospital Universitario Puerta de Hierro), Jaime González-Valcárcel (Hospital Universitario Ramón y Cajal), Concepción Murrieta (Hospital Infanta Leonor), Alicia Parra (Hospital Universitario Príncipe de Asturias), María Rabasa (Hospital de Fuenlabrada), Aurelio Vega (Hospital Universitario Puerta de Hierro).
Coordinators:
María Alonso de Leciñana (Stroke Unit, Department of Neurology, Hospital Universitario Ramón y Cajal, IRyCIS), Exuperio Díez Tejedor (Neurology Department and Stroke Centre, Hospital Universitario La Paz, IdiPAZ).
Writers:
Jaime Díaz (Stroke Unit, Department of Neurology, Hospital Universitario 12 de Octubre), José Antonio Egido (Stroke Unit, Department of Neurology, Hospital Universitario Clínico San Carlos), Andrés García Pastor (Stroke Unit, Department of Neurology, Hospital Universitario Gregorio Marañón), Patricia Martínez-Sánchez (Neurology Department and Stroke Centre, Hospital Universitario La Paz, IdiPAZ), José Vivancos (Stroke Unit, Department of Neurology, Hospital Universitario La Princesa).
Participants:
Eduardo Bárcena (Interventional Neuroradiology, Hospital Universitario La Princesa), Jorge Campello (Interventional Neuroradiology, Hospital Universitario 12 de Octubre), Enrique Castro (Interventional Neuroradiology, Hospital Universitario Gregorio Marañón), Patricia Calleja (Stroke Unit, Department of Neurology, Hospital Universitario 12 de Octubre), José Luis Caniego (Interventional Neuroradiology, Hospital Universitario La Princesa), Elisa Correas (Neurology Department and Stroke Centre, Hospital Universitario La Paz, IdiPAZ), Antonio Cruz (Stroke Unit, Department of Neurology, Hospital Universitario Ramón y Cajal, IRyCIS), Fernando Díaz-Otero (Stroke Unit, Department of Neurology, Hospital Universitario Gregorio Marañón), Eduardo Fandiño (Interventional Neuroradiology, Hospital Universitario Ramón y Cajal, IRyCIS), Andrés Fernández Prieto (Interventional Neuroradiology, Hospital Universitario La Paz, IdiPAZ), Fernando Fortea (Interventional Neuroradiology, Hospital Universitario Gregorio Marañón), Blanca Fuentes (Neurology Department and Stroke Centre, Hospital Universitario La Paz, IdiPAZ), Alfonsa Friera (Interventional Neuroradiology, Hospital Universitario La Princesa), Remedios Frutos (Interventional Neuroradiology, Hospital Universitario La Paz, IdiPAZ), Ana García-García (Stroke Unit, Department of Neurology, Hospital Universitario Clínico San Carlos), Alberto Gil (Interventional Neuroradiology, Hospital Universitario Clínico San Carlos), Antonio Gil-Nuñez (Stroke Unit, Department of Neurology, Hospital Universitario Gregorio Marañón), Francisco Gilo (Stroke Unit, Department of Neurology, Hospital Universitario La Princesa), Luis López-Ibor (Interventional Neuroradiology, Hospital Universitario Clínico San Carlos), Begoña Marín (Interventional Neuroradiology, Hospital Universitario La Paz, IdiPAZ), Antonio Martínez-Salio (Stroke Unit, Department of Neurology, Hospital Universitario 12 de Octubre), Jaime Masjuan (Stroke Unit, Department of Neurology, Hospital Universitario Ramón y Cajal, IRyCIS), José Carlos Méndez (Interventional Neuroradiology, Hospital Universitario Ramón y Cajal, IRyCIS), Pedro Navia (Interventional Neuroradiology, Hospital Universitario 12 de Octubre), Florentino Nombela (Stroke Unit, Department of Neurology, Hospital Universitario La Princesa), Gemma Reig (Stroke Unit, Department of Neurology, Hospital Universitario La Princesa), Gerardo Ruiz-Ares (Neurology Department and Stroke Centre, Hospital Universitario La Paz, IdiPAZ), Carmen Sánchez (Stroke Unit, Department of Neurology, Hospital Universitario 12 de Octubre), Carmen Serna (Stroke Unit, Department of Neurology, Hospital Universitario Clínico San Carlos), Patricia Simal (Stroke Unit, Department of Neurology, Hospital Universitario Clínico San Carlos), Francisco Villoria (Interventional Neuroradiology, Hospital Universitario Gregorio Marañón), Álvaro Ximenez-Carrillo (Stroke Unit, Department of Neurology, Hospital Universitario La Princesa).
Addendum
Three recently published clinical trials examine the efficacy of endovascular treatment in ischaemic stroke.40–42 First of all, these trials show that endovascular treatment is not superior to treatment with rtPA40; furthermore, systematically providing endovascular treatment after thrombolysis is not effective.41 Secondly, they indicate that using multimodal CT or MR neuroimaging techniques to identify persistent tissue in the ischaemic penumbra does not aid in selecting patients for endovascular treatment.42 These results must be validated by further studies and they do not modify the recommendations in this protocol.
Please cite this article as: Alonso de Leciñana M, Díaz-Guzmán J, Egido JA, García Pastor A, Martínez-Sánchez P, Vivancos J, et al. Tratamiento endovascular en el ictus isquémico agudo. Plan de Atención al Ictus en la Comunidad de Madrid. Neurología. 2013;28:425–434.
The affiliation of the authors and the composition of the Committee are contained in Appendix A.