We present the case of a 51-year-old male patient, a smoker, with history of arterial hypertension and diabetes mellitus and no personal or family history of psychiatric disorders, who was brought to the emergency department after he reported hearing voices and feeling a nearby presence, which he could not see but was able to hear and feel. Both the voices and the felt presence were perceived from his left side. Furthermore, the patient’s relatives reported a one-week history of short episodes of disconnection from his surroundings. The patient only reported severe headache. He did not complain with regard to the voices or the felt presence, which he considered to be real, and was unaware of the episodes of disconnection. The neurological examination revealed left superior homonymous quadrantanopia, left-sided visual extinction, and left-sided sensory extinction. An emergency head CT scan revealed a hypodense area in the right temporoparietal region, with no contrast uptake, coinciding with an MRI lesion suggestive of acute ischaemic stroke (Fig. 1). During hospitalisation, psychotic symptoms progressed to paranoid delusions of voices and felt presence. The patient was wary and became verbally aggressive when it was suggested that the voices and presence were not real. We prescribed symptomatic treatment with risperidone dosed at 1 mg/8 h. Given the atypical age of onset for primary psychosis, the co-presence of an acute brain lesion, and the occurrence of new episodes of disconnection, we requested an emergency EEG study, suspecting ictal psychosis. The EEG study, of 40 min’ duration, detected 3 focal epileptic seizures lasting 1-2 min, starting in the right centroparietal region, as well as postictal slowing in the right centrotemporal region (Fig. 2). Interictal EEG revealed right temporal focal slowing. In terms of clinical signs during the episodes of paranoid delusion, the patient gazed to the left, stopping any activity, and uttered some out-of-context yet well-structured sentences; level of consciousness was preserved. During the EEG study, he reported feeling the presence to his left side. Given that EEG findings supported the suspected diagnosis of ictal psychosis, altered perception (voices, felt presence) and thought (paranoid delusion) were interpreted as symptoms of psychic focal seizures (or cognitive seizures, according to the 2017 ILAE classification1) secondary to the acute ischaemic lesion. We started antiepileptic treatment with levetiracetam at up to 1500 mg/12 h. As the patient presented only a partial response, we added phenytoin dosed at up to 100 mg/8 h, which achieved substantial improvements: delirium (voices and felt presence) resolved and the patient began to question his perceptions. He was discharged, presenting no further events; he is currently not receiving antipsychotics but continues treatment with levetiracetam dosed at 1500 mg/12 h.
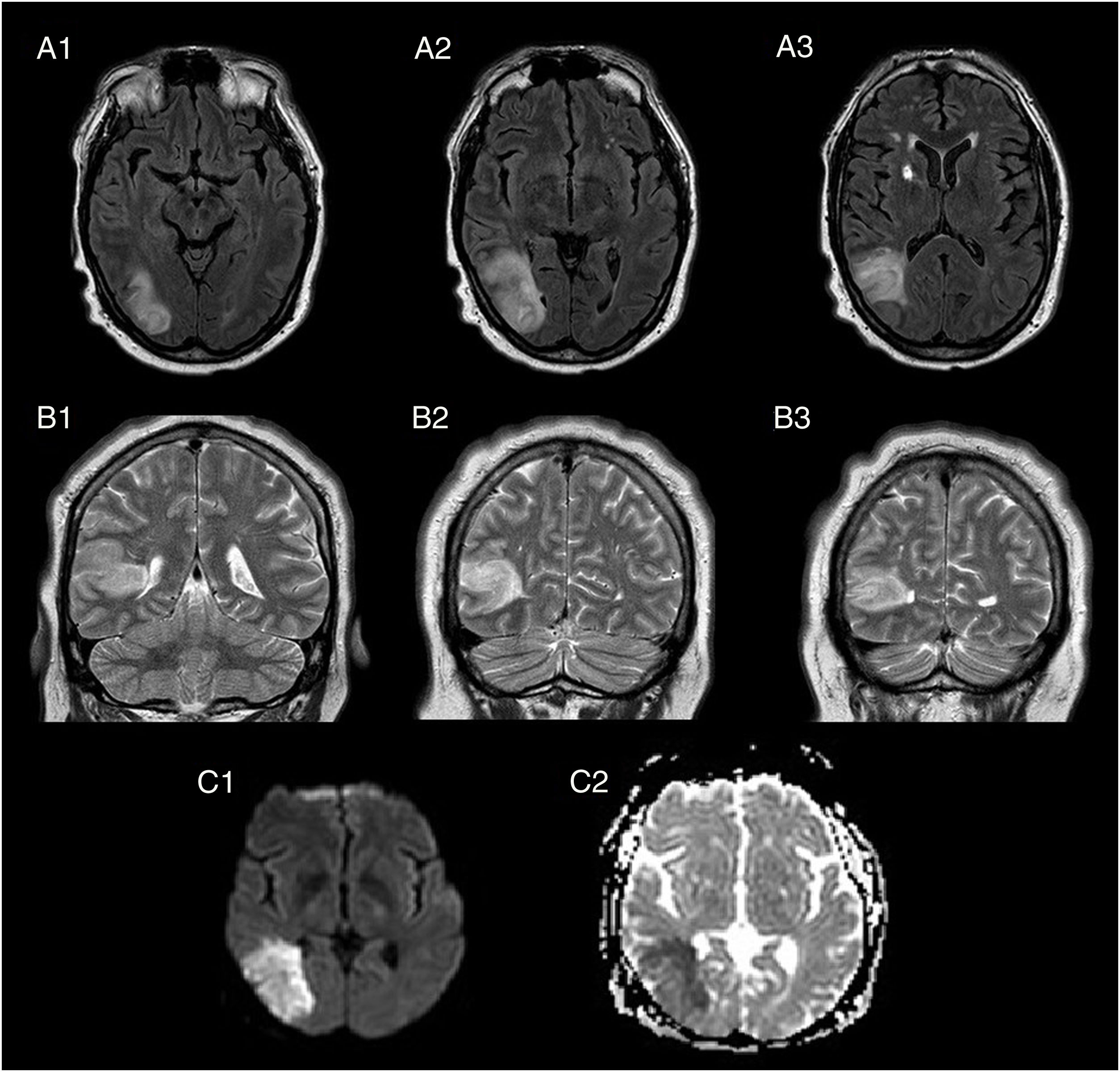
Brain MRI: FLAIR sequences, axial plane (A1-A3); T2-weighted sequences, coronal plane (B1-B3); diffusion-weighted sequences, axial plane (C1 = tDWI, C2 = ADC). The images reveal a hyperintense cortical-subcortical lesion in the right temporal lobe on T2-weighted and FLAIR sequences (A1-B3), involving the right middle and inferior temporal gyri and extending to the ipsilateral peritrigonal region and occipital horn of the lateral ventricle. Hyperintensity in diffusion-weighted sequence (C1), with low signal in the ADC map (C2).
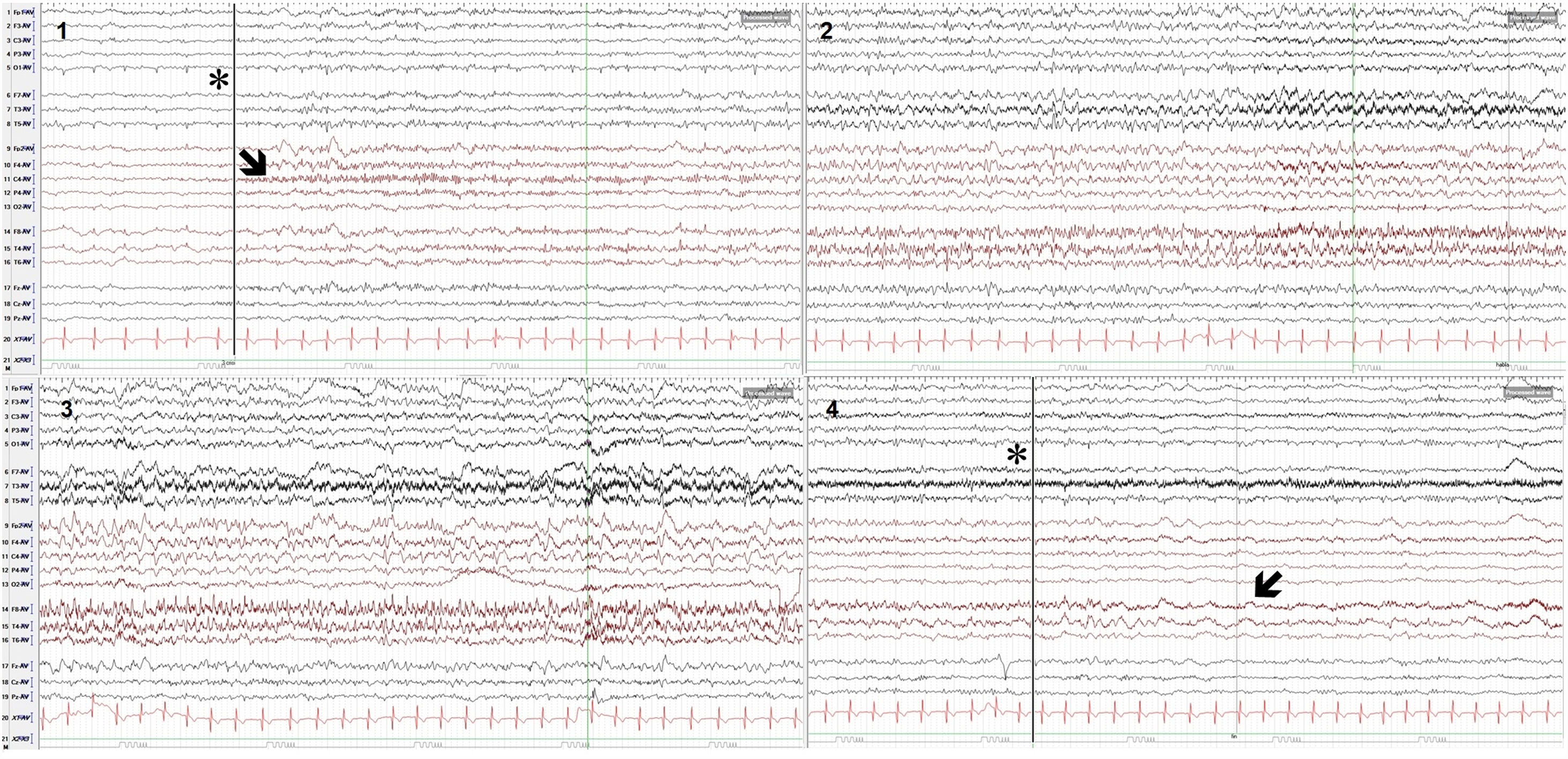
Surface electroencephalography: epileptiform activity during one of the seizures. Electrodes were placed according to the international 10-20 system. Monopolar recording (AV: average); sensitivity: 10 mV; high-frequency filter: 70 Hz; 30-s epochs. The recording shows 4 epochs: seizure onset (epoch 1, asterisk and vertical line), with fast rhythmic activity in the right centroparietal region and midline (C4-P4-Cz; epoch 1, arrow), which increases in amplitude and propagates to adjacent derivations, leading to slow, regular, rhythmic activity (theta/alpha waves), with sharp waves in frontotemporal regions, predominantly on the right side (epochs 2 and 3), until seizure resolution (epoch 4, asterisk and vertical line), and postictal slowing in the right centrotemporal region (epoch 4, arrow).
Psychotic symptoms are reported in up to 7% of patients with epilepsy,2 a prevalence rate twice as high as that calculated in the general population (3%).2,3 In epileptic patients, psychosis is classified as ictal, postictal, or interictal, depending on its temporal relationship with seizures.4–6 In ictal psychosis, psychotic symptoms constitute the clinical manifestation of epileptic activity.4 Postictal psychosis starts after a seizure, following a lucid period lasting hours or days.4–6 Interictal psychosis appears during seizure-free intervals.4–6 Several neuroanatomical and neurophysiological mechanisms explain the pathogenesis of psychosis in patients with epilepsy.4 From a neuroanatomical viewpoint, the type of epilepsy most frequently associated with psychosis is temporal lobe epilepsy involving the hippocampus and amygdala. Involvement of other limbic structures and the frontal lobe has also been associated with ictal psychosis. Furthermore, the dopaminergic system, involved in psychosis, also plays a role in epilepsy, causing glutamate hyperactivity and GABA hypoactivity.7 Therefore, psychosis may be a non-incidental finding in epileptic patients.
Our patient had a form of ictal psychosis. The condition is characterised by hallucinations, affective disorders, and delirium.6 Our patient also presented the peculiar “feeling of a presence.” The “feeling of a presence” is defined as the illusion or perception that somebody, whom the patient cannot see, is in his or her immediate surroundings.8 This phenomenon is explained by a disorder of own body perception; somatosensory inputs are projected outside the intrapersonal space toward the extrapersonal space as a result of lesions in temporoparietal association areas responsible for bodily self-consciousness.8,9 This feeling of a presence has previously been described in isolated cases as a semiological manifestation of epileptic seizures.8–10 We should therefore rule out epilepsy in patients with lesions to association areas involved in bodily self-consciousness who report feeling a presence. Our patient presented feeling of a presence, auditory hallucinations, and delusional ideation as symptoms of ictal psychosis.
Author contributionsAll authors contributed intellectual content to this study and approved the final version of the manuscript.
Conflicts of interestThe lead author presented this case in the 2018 edition of the Esteve Epilepsy Clinical Case Contest and won the first prize in the general category, receiving €1500 to be used exclusively to cover the costs of attending a national or international epilepsy congress or an epilepsy training course. This clinical case was included in the 3rd edition of an online training course on clinical cases of epilepsy offered by Esteve. As stipulated in the contest terms and conditions, any intellectual property rights corresponding to the case report remain the property of Esteve and may be ceded to a third party. The leading author obtained permission from Esteve to submit this case report to Neurología. The manuscript submitted for publication in Neurología is not an identical reproduction of the text and images of the case presented at the contest, but constitutes an adaptation meeting the publication requirements of the journal.
We would like to thank Dr Íñigo Garamendi Ruiz, an epilepsy expert from the neurology department at Hospital Universitario Cruces.
Please cite this article as: Moreno-Estébanez A, Marinas Alejo A, Ontiveros Navarro SJ, Bilbao Villabeitia I. Epilepsia: una historia de voces y fantasmas. Neurología. 2020;35:608–611.